Screening of nutritional risk among older persons
30–60 per cent of older adults in hospitals and nursing homes are malnourished. A well-suited screening tool is to detect the persons who are at risk of malnutrition.
Background: The prevalence of malnutrition among institutionalised and community-dwelling older persons with home nursing varies between 30–60 percent and 2–10 percent, respectively. An early determination of nutritional risk is important, to be able to initiate nutritional therapy and prevent malnutrition. However, it is unclear which screening tools are best suited for use in the two groups of older persons in need of care.
Objective: To identify screening tools that can determine the risk of undernutrition in institutionalised and community-dwelling older persons with home nursing, by examining the validity, reliability and acceptability of tools that have been identified.
Method: Systematic literature study. The searches were conducted in 2014 in the databases MEDLINE, Cinahl, Ovid Nursing and Food Science Source, PubMed, Embase and The Cochrane Central Register of Controlled Trials, and hand search of journals.
Results: We found four different screening tools, MNA-SF, SNAQ, MST and GNRI, reported in nine validation studies. MNA-SF was validated most times (four studies) and both sensitivity and specificity were high. MST was validated in one study with moderate specificity. The other tools showed moderate validity. None of the included studies examined the usefulness of the screening tool.
Conclusion: Four screening tools, MNA-SF, SNAQ, MST and GNRI, were validated in the two groups of elderly persons. MNA-SF was best suited to uncover nutritional risk in both groups, but more research is needed.
Keywords: Elderly, malnutrition, nutritional screening, review, screening tool
Introduction
Older adults are at risk for developing malnutrition (1, 2). Studies show that as much as 30-60 per cent of older adults in hospital and nursing homes (3-6) and 2-10 per cent of older adults living at home with home care services are malnourished (4, 5 ,7, 8). Older adults with dementia conditions are particularly at risk (9). One cause of malnutrition may be that health personnel do not properly identify risk factors such as poor appetite and eating disorders among the elderly. Several studies have uncovered inadequate routines and procedures for assessing food intake and nutritional state in various health institutions (10, 11).
It is important to focus on malnutrition in the health services as the condition can cause the patient increased suffering and death. Malnutrition leads to increased health care costs to society due to delayed recovery, readmissions and an increased need for home care services (12, 13). In 2009 the Norwegian Directory of Health published National medical guidelines for the prevention and treatment of malnutrition. Their goal is to identify persons who are malnourished or at risk for malnutrition in order to deliver nutritional therapy (14). According to these guidelines screening of nutritional risk shall be included in the nurse’s routine assessment of a patient. The regulations state that patients in nursing homes and elderly with home care services shall be screened for nutritional risk at admission or at the granting of home care services, and later be screened on a monthly basis.
Screening is used in a series of contexts within the health services and may be defined as examinations offered to apparently healthy persons to uncover a particular phenomenon or disease (15). Screenings for nutritional risk may identify persons at increased risk of malnutrition (16). A series of tools have been developed for this purpose (2, 13, 14, 17). The Norwegian Directory of Health recommends that health personnel use Mini Nutritional Assessment (MNA) and Malnutrition Universal Screening Tool (MUST) to screen for nutritional risk in elderly persons, and they point to Nutritional Risk Screening (NRS 2002), Subjective Global Assessment (SGA) and Ernæringsjournal [Nutritional journal] as alternative tools. To serve its purpose, a screening tool must measure what it is supposed to measure (be valid), and give the same result in repeated measurements (reliability). The Norwegian Directory of Health guidelines do not address the recommended screening tools’ validity and reliability (14).
"Older adults are at risk for developing malnutrition."
Several of the tools are developed for use in hospitals (2), and it is not clear whether they are suitable for screening for nutritional risk in elderly residents in nursing homes or in the home care services. Another important point that the guidelines do not touch upon, is whether the tool is easy to use (practical, quick and simple) for both nurses and patients (18,19). The purpose of this study is to identify screening tools suitable for uncovering risk of malnutrition in elderly residents in long-term care facilities, and among users of home care services. This is achieved by summing up what research says about validity, reliability and applicability.
Method
A systematic literature study was performed.
Search strategy
To identity relevant publications we performed systematic literature searches in the databases MEDLINE, Cinahl, Ovid Nursing of Food Science (via EBSCO), PubMed, Embase and The Cochrane Central Register of Controlled Trials (CENTRAL). The searches were carried out in February 2014 with a librarian with literature search competence. Search words included MESH terms in the various databases in addition to free search words. The following search words were combined in the searches:
- elderly, older adults, old age, aged
- community dwelling, home care, out-patients, primary health care, nursing home
- nutritional status, malnutrition, undernutrition, weight loss, and
- screening tools, assessment methods, tools, geriatric assessment, questionnaire.
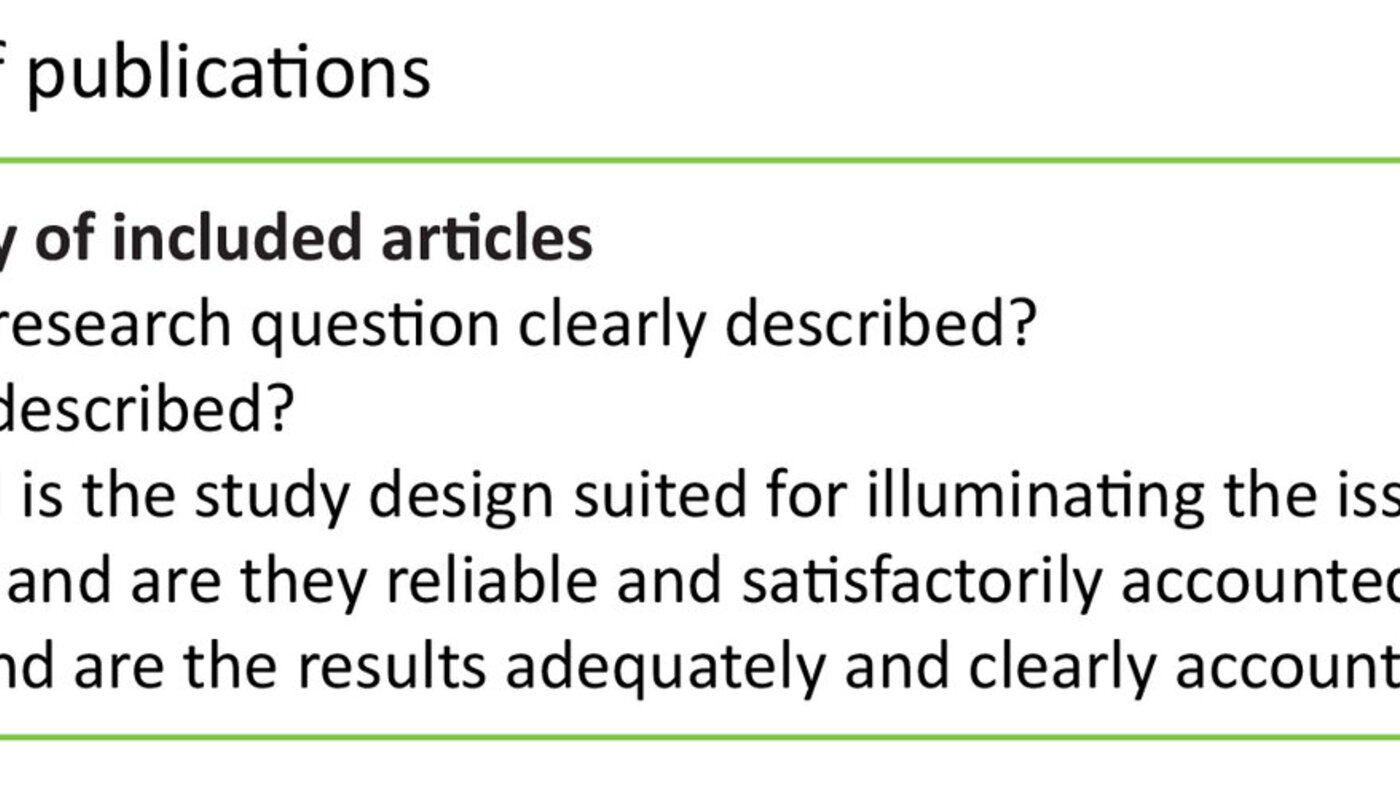
A survey of reference lists from key articles was performed. All identified articles were transferred to a data programme for processing and organisation of references, (EndNote X7) and screened for duplicates. All four authors subsequently went through the list of articles by looking at title and abstract and assessing the articles for inclusion. Disagreements were solved by discussion and reasons for exclusions were given. We then analysed the content in the included studies by reading the articles in accordance with recommendations in The Cochrane Handbook for Systematic Reviews of Interventions (20). As we included non-randomised studies, we used a pragmatic quality assessment model based on the Cochrane guidelines (Table 1).
Inclusion and exclusion criteria
The searches were limited to quantitative studies published in English, German, Norwegian, Swedish or Danish in peer-reviewed journals the past 15 years.
Inclusion criteria
- age ≥ 65
- community-dwelling with home care services
- resident in long-term care facility with nursing personnel present, such as nursing home or assisted living facility
- studies performed to validate one or several screening tools
Exclusion criteria
- studies designed to assess prevalence of nutritional risk or malnutrition
- studies that do not validate pure screening tools (16), but tools such as SGA and MNA, which are approved and valid methods for measuring nutritional status in elderly adults (21-23).
- validation of country-specific screening tools
- disease-specific target groups such as cancer patients, patients with Alzheimer’s disease or patients with various neurological diseases
- studies with ten or less patients
Assessment criteria
Assessments of criteria validity are generally made against a gold standard (24). In the absence of such a gold standard other criteria or reference methods must be used. In this study we chose to accept the following criteria or reference methods:
- tool for assessing nutritional status (SGA and MNA)
- objective assessment of nutritional status performed by health personnel
- nutritional assessment based on anthropometrics (weight, body mass index (BMI), arm muscle circumference etc.)
To evaluate correlation between the screening tool and the reference method we used the following outcome measures: sensitivity, specificity, positive (PPV) and negative predictive value (NPV). High sensitivity indicates that the test uncovers as many as possible of persons at risk for malnutrition (15). High specificity indicates that the test yields few false positives. Sensitivity and specificity and the prevalence of the condition give the predictive value of the screening method. PPV indicates the proportion of persons classified in the high-risk group and who are in fact at risk. NPV indicates the proportion of persons who are not categorised as high-risk and who are not (15, 25). Both PPV and NPV are given as percentages, and the higher the percentage, the better the screening. Low NPV indicates overdiagnosis.
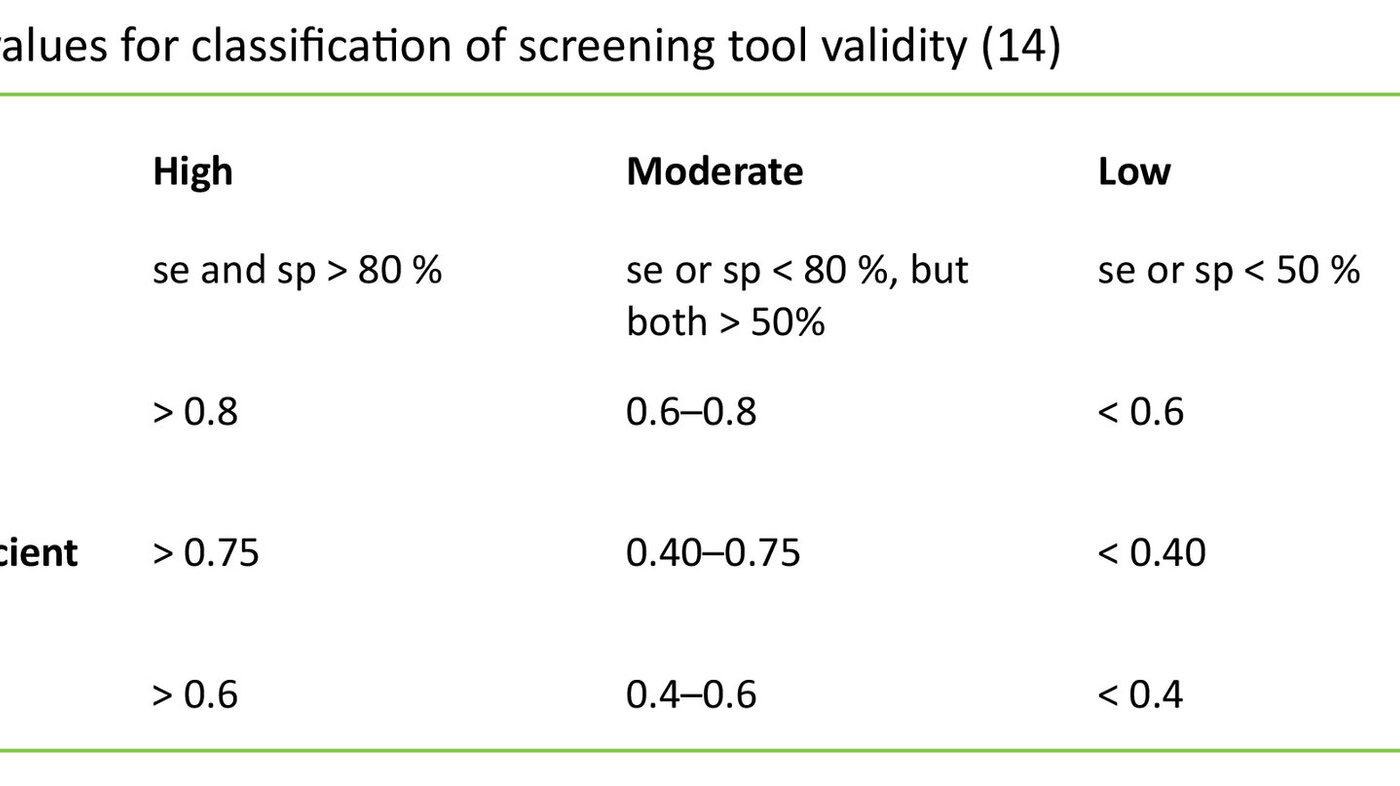
The following outcome measures were further included: area under the curve (AUC), correlation coefficient (CC) and kappa values (k). Receiver operator curves (ROC) indicate the relationship between true positives and false positives. The area under ROC (AUC) is a measure of the diagnostic value of the screening tool. AUC may vary between 0 and 1, where AUC = 0.5 indicates that the screening tool cannot distinguish between the groups, and AUC = 1 indicates perfect test. The correlation coefficient r indicates correspondence between two variables and will always be between -1 and 1. The closer r is to -1 or 1, the stronger the correlation between the two variables. Kappa value (k) is a reliability coefficient and indicates agreement between two measures. The kappa value will vary between 0 and 1, and the closer to 1, the greater the correlation. The cut-off values for these outcome measures are shown in table 2 (17).
The PRISMA recommendations (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) (26) were followed in reporting the publications.
Results
A flow-chart showing the search and selection process is shown in Figure 1.
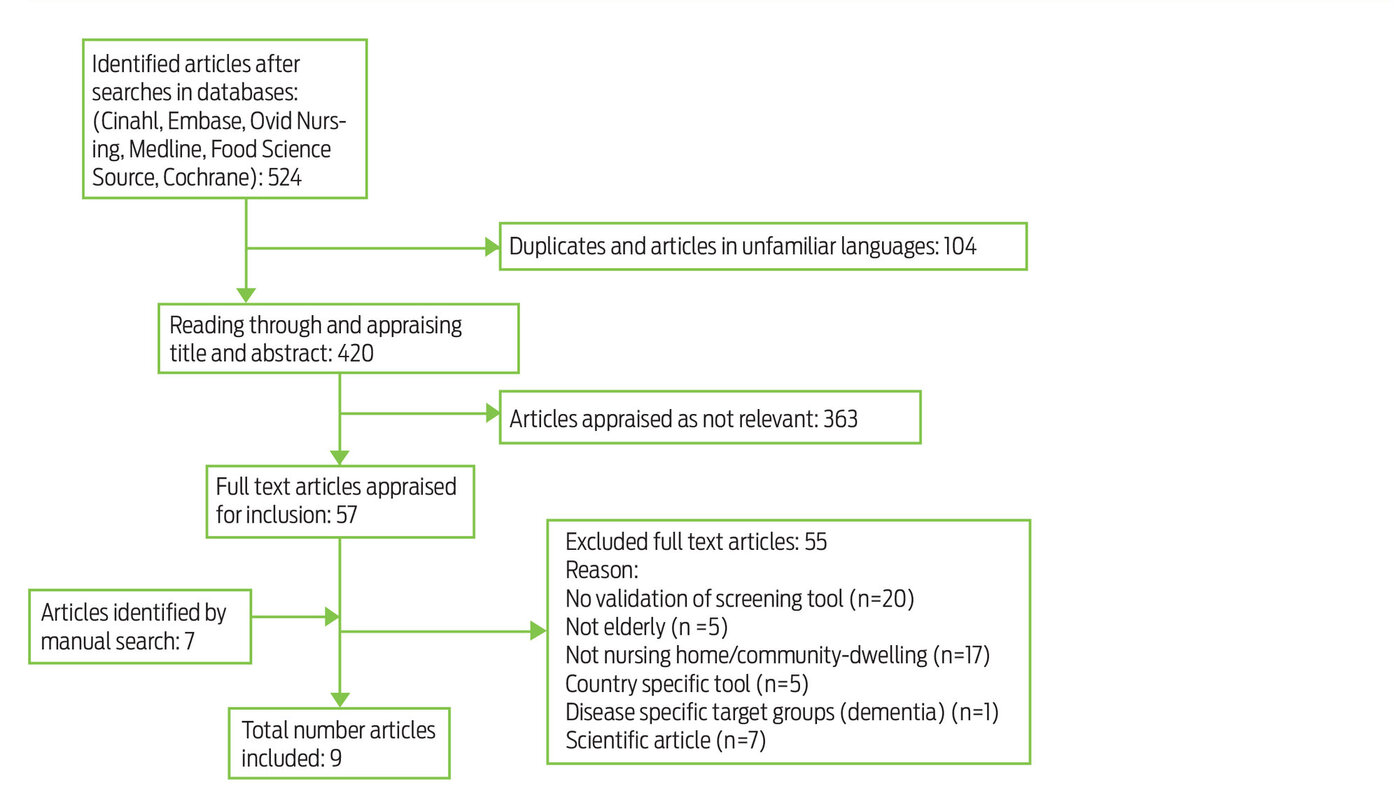
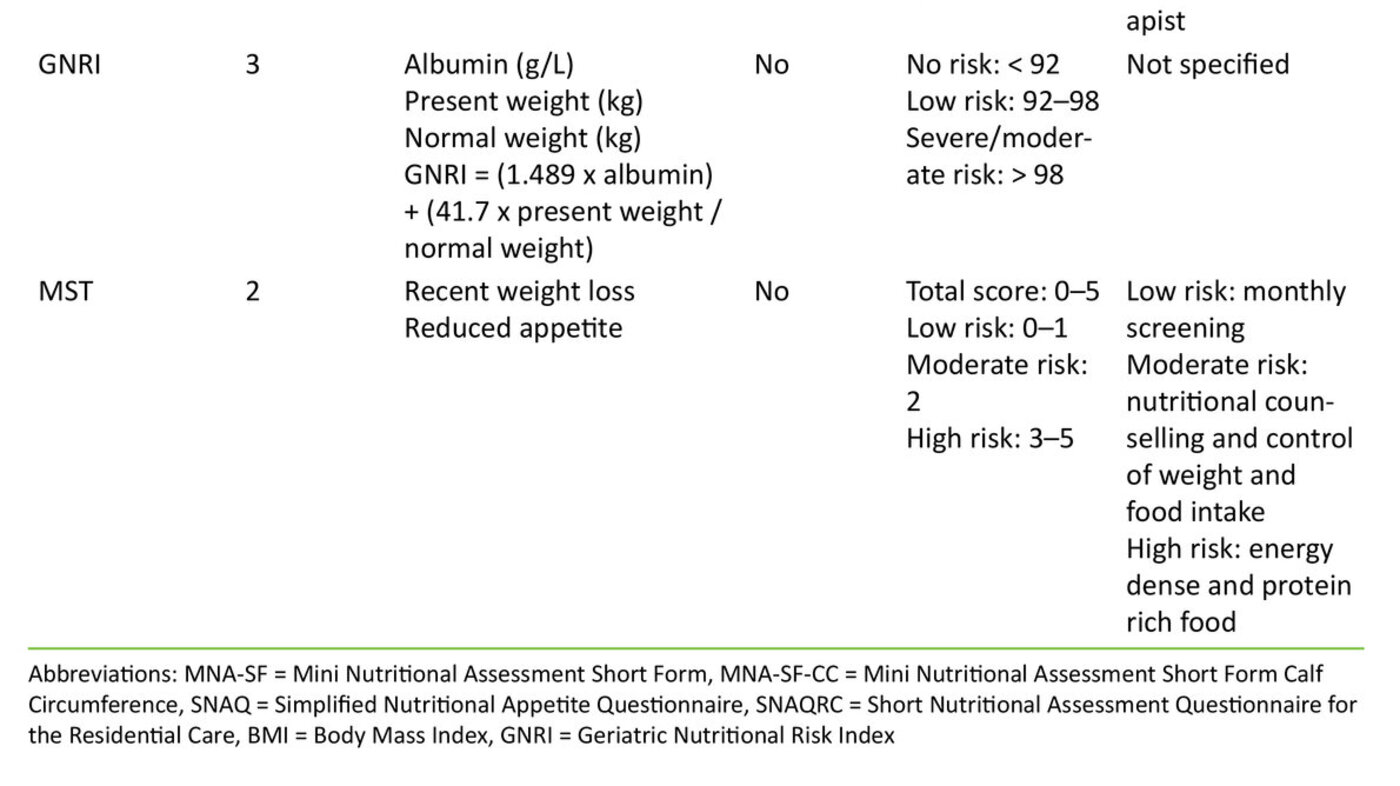
The literature searches yielded a total of 524 articles. After having removed duplicates of articles found in different databases and articles in unfamiliar languages, 420 articles remained. We assessed title and abstract of the studies in accordance with the inclusion criteria. This process resulted in 57 articles, which were read in full. We divided the articles between us and quality assured what had been abstracted by going through all articles together. An additional seven articles were found by going through reference lists of included articles and key survey articles. Of 64 articles 55 were excluded, mainly because they did not represent validation studies (n=20), or because the validation was not performed in a nursing home or among community-dwelling elderly (n=17). This literature review is thus based on nine articles and the validation of four distinct screening tools. Only one of these tools, MNA_Short Form (MNA-SF), has been translated into Norwegian. The validated screening tools are presented in Table 3.
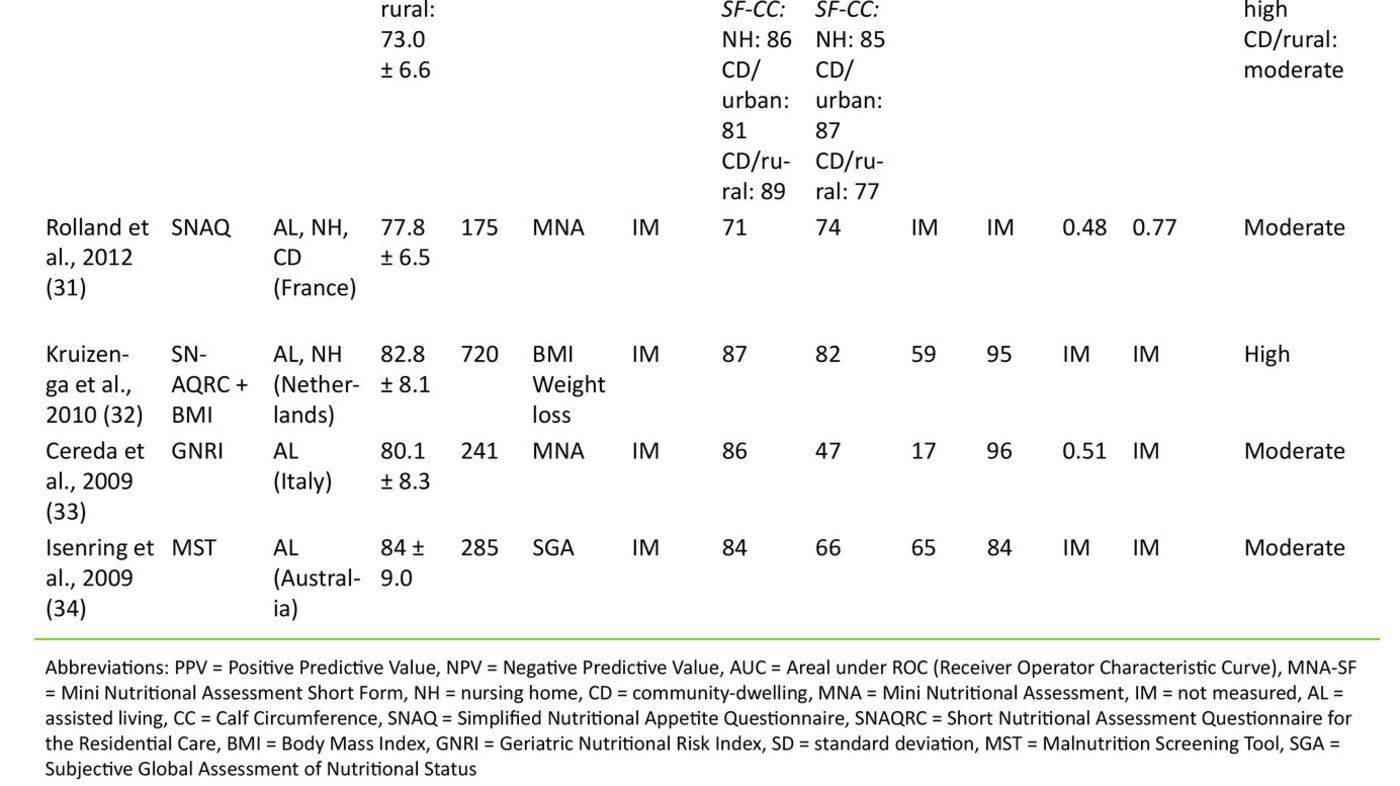
MNA-SF.Four studies (27-30) with a total 3599 (127-2603) elderly over 65 years assessed the validity of MNA-SF, including a variety, MNA-SF Calf Circumference (MNA-SF-CC), in which BMI is replaced with calf circumference. In all the studies the full version of MNA was used as a reference method. Three studies performed validation among both community-dwelling elderly and elderly residing in long-term care facilities (nursing home) (27, 29, 30). One study performed validation only in long-term care facility (assisted living) (28). The results from these studies showed that MNA-SF had moderate validity used among community-dwelling elderly and high when used in long-term care facilities (Table 4). Sensitivity among community-dwelling elderly varied between 74 – 89 per cent and the specificity between 77 – 95 per cent (21, 24). Among elderly in long-term care facilities the variation was 64 – 89 per cent and 82 – 100 per cent respectively (27, 29, 30). Two studies assessed percentage correlation between classification using the reference method (MNA), MNA-SF and MNA-SF-CC (29, 30).
"30–60 per cent of older people in hospitals and nursing homes are malnourished."
Among community-dwelling elderly there were 83 per cent and 91 per cent correlation between classifications done with MNA and MNA-SF and 72 per cent and 90 per cent between MNA and MNA-SF-CC. In long-term care facilities the corresponding correlation was 82 per cent and 83 per cent, and 76 per cent and 77 per cent respectively. Huhmann (35) investigated whether the screening results were the same when community-dwelling elderly completed a self-administered MNA-SF-version (MNA-SF-self), and health personnel completed MNA-SF (result not shown in table). The study included 463 elderly > 65 years and their care person. The correlation between answers from the elderly and the health personnel was 90 per cent for those who were classified as of normal weight, 89 per cent for those who were classified as at risk for malnutrition, and 99 per cent for the group classified as malnourished. The study concluded that the inter-rater-reliability is high, and that MNA-SF-Self may to advantage be used to screen nutritional status among community-dwelling elderly.
Simplified Nutritional Appetite Questionnaire (SNAQ).Two studies with a total 895 elderly assessed the validity of SNAQ and a version of SNAQ that includes BMI (SNAQ-BMI) (31, 32). SNAQ was validated among community-dwelling elderly and elderly in long-term care facilities and showed moderate validity in relation to MNA (31). SNAQ-MNI validated in long-term care facilities showed high sensitivity compared to MNA. A large proportion (PPV = 59 per cent), however, was classified as at risk without being so (32), i.e. overestimation of risk of malnutrition.
Geriatric Nutritional Risk Index (GNRI)was validated in a study with 241 elderly in long-term care facilities. The screening tool was validated against MNA and showed moderate validity (33). This was primarily due to low specificity and low positive predictive value (PPV = 17 per cent). This indicates that GNRI overestimates risk.
Malnutrition Screening Tool (MST). One study validated the screening tool MST among 285 elderly in long-term care facilities with SGA as reference method (34). The screening tool was moderately valid in this group, primarily due to moderate specificity and PPV.
The included validation studies did not assess the applicability of the tool.
Discussion
The purpose of this study was to identify screening tools suitable for uncovering risk of malnutrition in two groups of older adults: community-dwelling elderly receiving nursing services in the home, and elderly residents in long-term care facilities defined as nursing homes and assisted living. We found in total four screening tools – MNA-SF, SNAQ, MST and GNRI – that were validated in the two groups. MNA-SF was validated in four studies (27-30). Even though the studies are few, the number of participants was relatively large and the results relatively univocal with moderate to high validity when MNA was used as a reference method. There is thus basis for saying that MNA-SF is suitable for uncovering nutritional risk in elderly in long-term care facilities and among community-dwelling elderly. With regard to the tools SNAQ, MST and GNRI, few validation studies were carried out in the two groups of elderly. There is thus a need for more research in order to say anything about how well suited these tools are.
When assessing whether a tool is suitable for screening nutritional risk, it is important that it is able to identify the persons at risk of malnutrition. Such persons may then be followed up and their nutritional status assessed and efforts instituted to prevent the development of malnutrition. The sensitivity of the screening tool and NPV are thus important measures when judging validity (15, 25). The tools we found had high sensitivity, and SNAQ, MST and GNRI had high NPV as well. NPV for MNA-SF was estimated in only one study (27), and the value was satisfactory for community-dwelling elderly, but significantly lower in nursing homes. MNA-SF’s sensitivity seemed higher among community-dwelling elderly than among elderly in long-term care facilities. The difference may be due to the strong emphasis on mobility and cognitive function in MNA-SF (3), and the fact that mobility and cognition are the very functions that are impaired when elderly are admitted to nursing homes. Their basic nutritional needs may nevertheless be met to a higher degree than for community-dwelling elderly due to the presence of health personnel. Poor mobility and impaired cognition are thus probably more relevant in a screening tool adapted to community-dwelling elderly. A Norwegian study from 1994 showed that mobility problems and resulting difficulties with shopping for food were risk factors in the development of malnutrition in elderly persons (36).
"A screening tool is to uncover who is at risk for malnutrition."
MST is a frequently used screening tool. It is not developed specifically for the elderly, but is found to be valid for use in hospitals and in connection with outpatient clinic activity (37). We found one study that validated the tool among elderly in long-term care facilities (34). Earlier validation of MST with the same reference method (SGA) in hospital yielded higher sensitivity (92 – 100 per cent) and specificity (81 – 93 per cent) than what was found among elderly in long-term care facilities (38-40). This reflects that MST is possibly better suited in acute settings, for which the tool was originally developed (38).
Overdiagnosis is a known risk with all types of screening (41). Among the screening tools we assessed, GNRI had low sensitivity and low positive predictive value, indicating that overdiagnosis may be a problem if this tool is used. SNAQ and MST seemed to overdiagnose as well, albeit to a lower extent than GNRI. One may argue that overdiagnosing malnutrition is better than underdiagnosing it, as the treatment in the case of malnutrition is about giving extra attention to food and the availability of it and does not entail any danger to the patient. On the other hand, time is spent on persons who do not really need it, possibly incurring unnecessary costs to the health services. Screening entails a certain risk of overdiagnosis and a screening tool with the highest possible specificity and sensitivity should be chosen, and the screening should be targeted to groups with a known prevalence of malnutrition (15, 41).
Our findings suggest that the same screening tool cannot be used to identify risk for malnutrition among community-dwelling elderly, elderly in long-term care facilities and in hospital. This emphasises the need for validating the screening tool in the patient arena it is to be used. In a long-term care facility the tool must capture a gradual change in nutritional status from insufficient food intake and/or a change of needs. In patients who are admitted to hospital, the tool shall uncover an already present risk (34). In this context it is interesting to note that none of the tools recommended by the Norwegian Directorate of Health (14) for screening nutritional risk in elderly persons, are validated among elderly in nursing homes or in their own homes. The guidelines recommend that the full version of MNA and MUST be used in the primary health services, and that NRS 2002, SGA and Ernæringsjournal [Nutrition journal] be used as an alternative. MNA and SGA are not developed to be used as screening tools, but are tools to assess nutritional status (37). Neither MUST or NRS2002 are specifically developed for the elderly (2) and are also not validated in the two groups of elderly we were interested in. The Ernæringsjournal is not, as far as we know, validated.
A series of screening tools use height and weight to assess nutritional risk. Such measurements may be misleading in the elderly due to ageing and functional disturbances. A version of MNA-SF has been developed which uses calf circumference (MNA-SF-CC) rather than BMI. Other studies (42) have shown that calf circumference and upper arm circumference alone are good indications of nutritional status in elderly. Nevertheless, MNA-SF, which includes BMI, was found to give a somewhat better nutritional assessment than the use of CC (27). MNA-SF-CC is thus only recommended when measuring BMI is not possible. One of the advantages of SNAQ is that the tool focuses primarily on appetite and meals.
"MNA-SF is a well-suited screening tool for identifying older persons with increased risk of malnutrition.”
In the studies included, most tools are compared to the full version of MNA. MNA is a tool used to assess nutritional status. MNA is well validated, but when the tool is compared with a more extensive nutritional assessment that also includes registration of food intake and blood tests, low specificity is indicated (2). It may look as if MNA automatically includes fragile elderly in the category malnourished and thus gives false positives (2, 43). As MNA may have such weaknesses, one may question whether MNA is a suitable reference method for assessing criteria validity. In this context it is also important to point out that when using a reference method to validate a screening tool, the tool cannot be better than the reference method itself (17). This emphasises even more the need for more studies investigating the success of various screening tools in uncovering nutritional risk.
Reliability is also key to the assessment of a screening tool. One way of assessing reliability is examining whether the same result is obtained when different nursing personnel perform the screening. A series of people are involved in the screening of nutritional risk in nursing homes and in the home care services. For the screening to be reliable, it is essential that the result obtained is the same, independently of who performs the screening. None of the studies had investigated this, but one study compared the result from the nursing personnel’s screening with MNA-SF and the patient’s own completion of the form (MNS-SF-Self) (29). They found the results to be relatively similar. This should be investigated further as having the patient fill in the screening form would save time for nurses.
A screening tool as such uncovers only whether the elderly person is at risk for malnutrition. Nurses are in charge of attending to the nutritional needs of patients, and it is essential that nurses follow up with efforts such as small portions, frequent meals and nutritionally dense food (44) for patients found to be at risk of malnutrition.
Conclusion
This study shows that there is little research available assessing validity, reliability and applicability of screening tools to uncover risk of malnutrition in elderly in long-term care facilities and community-dwelling elderly receiving home care services. Available research shows that MNA-SF is a well-suited screening tool for this target group. SNAQ-BMI and MST can also be good screening tools in long-term care facilities, but seem to overdiagnose malnutrition. More research is needed, particularly with regard to reliability and applicability.
References
1. Mowé M. Behandling av underernæring hos eldre pasienter. Tidsskr Nor Lægeforen. 2002;122(8): 815–8.
2. van Bokhorst – de van der Schueren MAE, Guaitoli PcR, Jansma EP, de Vet HCW. A Systematic Review of Malnutrition Screening Tools for the Nursing Home Setting. Journal of the American Medical Directors Association. 2014;15(3):171–84.
3. Guigoz Y, Jensen G, Thomas D, Vellas B, et al. The Mini Nutritional Assessment (MNA®) Review of the literature – what does it tell us? / discussion. The Journal of Nutrition, Health & Aging. 2006;10(6):466–85; discussion 85–7.
4. Elia M, Zellipour L, Stratton R. To screen or not to screen for adult malnutrition? Clinical Nutrition. 2005;24:867-84.
5. Kaiser MJ, Bauer JM, Rämsch C, Uter W, Guigoz Y, Cederholm T, et al. Frequency of Malnutrition in Older Adults: A Multinational Perspective Using the Mini Nutritional Assessment. Journal of the American Geriatrics Society. 2010;58(9):1734-8.
6. Eide HK, Saltyte JB, Sortland K, Halvorsen K, Almeningen K. Prevalence of nutritional risk in the non-demented hospitalised elderly: a cross-sectional study from Norway using stratified sampling. Journal of Nutritional Science. 2015;4:e18.
7. Saletti A, Johansson L, Yifter-Lindgren E, Wissing U, Österberg K, Cederholm T. Nutritional status and a 3-year follow-up in elderly receiving support at home. Gerontology. 2005;51:192-8.
8. Söderhamn U, Dale B, Sundsli K, Söderhamn O. Nutritional screening of older home-dwelling Norwegians: a comparison between two instruments. Clin Interv Aging. 2012;7:383-91.
9. Rognstad M-K, Brekke I, Holm E, Linberg C, Lühr N. Underernæring hos eldre hjemmeboende personer med demens. Sykepleien Forskning. 2013;8(4):298–307.
10. Aagaard H. Mat og måltider i sykehjem. En nasjonal kartleggingsundersøkelse. Sykepleien Forskning. 2010;1(5):36–43.
11. Sortland K, Gjerlaug AK, Harviken G. Vektdokumentasjon, kroppsmasseindeks, måltidsfrekvens og nattefaste blant eldre sykehjemsbeboere – en pilotstudie. Vård i Norden. 2013;33(107):41–5.
12. Poulia K-A, Yannakoulia M, Karageorgou D, Gamaletsou M, Panagiotakos DB, Sipsas NV, et al. Evaluation of the efficacy of six nutritional screening tools to predict malnutrition in the elderly. Clinical Nutrition. 2012;31(3):378–85.
13. Kyle UG, Kossovsky MP, Karsegard VL, Pichard C. Comparison of tools for nutritional assessment and screening at hospital admission: A population study. Clinical Nutrition. 2006;25:409–17.
14. Guttormsen AB, Hensrud A, Irtun Ø, Mowé M, Sørbye LW, Thoresen L, et al. Nasjonale faglige retningslinjer for forebygging og behandling av underernæring. In: Helsedirektoratet (ed.). Helsedirektoratet, Oslo. 2009.
15. UK National Screening Committee. What is screening?: US Screening Portal; udatert. Available from: http://www.screening.nhs.uk/screening#fileid7942. (Downloaded 11.05.2015).
16. Charney P. Nutrition Screening vs Nutrition Assessment: How Do They Differ? Nutrition in Clinical Practice. 2008;23(4):366–72.
17. van Bokhorst-de van der Schueren MAE, Guaitoli PcR, Jansma EP, de Vet HCW. Nutrition screening tools: Does one size fit all? A systematic review of screening tools for the hospital setting. Clinical Nutrition. 2014;33(1):39–58.
18. Green SM, Watson R. Nutritional screening and assessment tools for use by nurses: literature review. Journal of Advanced Nursing. 2005;50(1):69–83.
19. Skipper A, Ferguson M, Thompson K, Castellanos V, Porcari J. Nutrition Screening Tools: An Analysis of the Evidence. Journal of Parenteral and Enteral Nutrition. 2011;36(3):292–8.
20. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0: The Cochrane Collaboration; 2011. Available from: www.cochrane-handbook.org.
21. Christensson L, Unosson M, Ek AC. Evaluation of nutritional assessment techniques in elderly people newly admitted to municipal care. European Journal of Clinical Nutrition. 2002;56(9):810.
22. Sacks G, Dearman K, Replogle WH, Cora VL, Meeks M, Canada T. Use of Subjective Global Assessment to Identify Nutrition-Associated Complications and Death in Geriatric Long-Term Care Facility Residents. Journal of the American College of Nutrition. 2000;19(5):570–7.
23. Guigoz Y. The Mini Nutritional Assessment (MNA) Review of the litterature – What does it tell us? The Journal of Nutrition, Health & Aging. 2006;10(6):466–87.
24. Ringdal K. Enhet og mangfold: samfunnsvitenskapelig forskning og kvantitativ metode. 3. ed. Fagbokforlaget, Bergen. 2013.
25. Ejlertsson G. Statistik för hälsovetenskaperna. Studentlitteratur, Lund. 2012.
26. Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche Pea. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. BMJ. 2009;339.
27. Borowiak E, Kostka T. Usefulness of short (MNA-SF) and full version of the Mini Nutritional Assessment (MNA) in examining the nutritional state of older persons. New Medicine. 2003;4:125–9.
28. Wikby K, Ek A-C, Christensson L. The two-step Mini Nutritional Assessment procedure in community resident homes. Journal of Clinical Nursing. 2008;17(9):1211–8.
29. Kaiser MJ, Bauer JM, Uter W, Donini LM, Stange I, Volkert D, et al. Prospective Validation of the Modified Mini Nutritional Assessment Short-Forms in the Community, Nursing Home, and Rehabilitation Setting. Journal of the American Geriatrics Society. 2011;59(11):2124–8.
30. Kostka J, Borowiak E, Kostka T. Validation of the modified mini nutritional assessment short-forms in different populations of older people in Poland. The journal of nutrition, health & aging. 2014;18(4):366–71.
31. Rolland Y, Perrin A, Gardette V, Filhol N, Vellas B. Screening Older People at Risk of Malnutrition or Malnourished Using the Simplified Nutritional Appetite Questionnaire (SNAQ): A Comparison With the Mini-Nutritional Assessment (MNA) Tool. Journal of the American Medical Directors Association. 2012;13(1):31–4.
32. Kruizenga HM, De Vet HCW, Van Marissing CME, Stassen EEPM, Strijk JE, Van Der Schueren MAEVB-D, et al. The SNAQRC, an easy traffic light system as a first step in the recognition of undernutrition in residential care. Journal of Nutrition, Health & Aging. 2010;14(2):83–9.
33. Cereda E, Pusani C, Limonta D, Vanotti A. The ability of the Geriatric Nutritional Risk Index to assess the nutritional status and predict the outcome of home-care resident elderly: a comparison with the Mini Nutritional Assessment. British Journal of Nutrition. 2009;102 (04):563–70.
34. Isenring EA, Bauer JD, Banks M, Gaskill D. The Malnutrition Screening Tool is a useful tool for identifying malnutrition risk in residential aged care. Journal of Human Nutrition and Dietetics. 2009;22(6):545–50.
35. Huhmann MB, Perez V, Alexander DD, Thomas DR. A self-completed nutrition screening tool for community-dwelling older adults with high reliability: A comparison study. The Journal of Nutrition, Health & Aging. 2013;17(4):339–44.
36. Mowé M, Bøhmer T, Kindt E. Reduced nutritional status in an elderly population (> 70 y) is probable before disease and possibly contributes to the development of disease. American Journal of Clinical Nutrition. 1994;59(2):317–24.
37. Isenring EA, Banks M, Ferguson M, Bauer JD. Beyond Malnutrition Screening: Appropriate Methods to Guide Nutrition Care for Aged Care Residents. Journal of the Academy of Nutrition & Dietetics. 2012;112(3):376–81.
38. Ferguson M, Capra S, Bauer J, Banks M. Development of a Valid and Reliable Malnutrition Screening Tool for Adult Acute Hospital Patients. Applied Nutritional Investigation. 1999;15(6):458–64.
39. Raja R, Lim AV, Lim YP, Lim G, Chan SP, Vu CKF. Malnutrition screening in hospitalised patients and its implication on reimbursement. Internal Medicine Journal. 2004;34(4): 176-81.
40. Isenring E, Cross G, Daniels L, Kellett E, Koczwara B. Validity of the malnutrition screening tool as an effective predictor of nutritional risk in oncology outpatients receiving chemotherapy. Support Care Cancer. 2006;14(11):1152–6.
41. Zahl P-H. Vitenskapelige kriterier for innføring og evaluering av screening. Tidsskr Nor Lægeforen. 2003;123(3):333–6.
42. Donini L, Poggiogalle E, Morrone A, Scardella P, Piombo L, Neri B, et al. Agreement between different versions of MNA. The Journal of Nutrition, Health & Aging. 2013;17(4):332–8.
43. Vellas B, Villars H, Abellan G, Soto M, Rolland Y, Guigoz Y, et al. Overview of the MNA – Its history and challenges. The Journal of Nutrition, Health & Aging. 2006;10(6):456–63.
44. Helsedirektoratet. Kosthåndboken – veileder i ernæringsarbeid i helse- og omsorgstjenesten. Helsedirektoratet, Oslo. 2012.










Comments