Women’s and men’s assessment of health and functional ability in HUNT 3 after a stroke
There is no difference in functional disability between women and men after having a stroke.
Bakgrunn: I Norge er det årlig cirka 15 000 sykehusinnleggelser på grunn av hjerneslag. Utenlandske studier har vist at flere kvinner enn menn rapporterer dårligere helse og funksjonsevne etter hjerneslag, men dette er lite undersøkt i Norge.
Hensikt: Undersøke om det er forskjell i kvinner og menns vurdering av helse, funksjonsevne, evne til å ivareta dagliglivets aktiviteter, og bruk av helsetjenester etter hjerneslag.
Metode: Tverrsnittstudie fra Helseundersøkelsen i Nord-Trøndelag (HUNT 3) innsamlet fra 2006–2008. Studien inkluderer 1190 personer som har hatt hjerneslag, 572 (48,1 prosent) kvinner og 618 (51,9 prosent) menn.
Resultat: 71,5 prosent kvinner og 73 prosent menn hadde kommet seg helt etter siste hjerneslag. Kun 6,2 prosent hadde svært alvorlig, alvorlig eller moderat funksjonssvikt. Kvinner ble sjeldnere innlagt på sykehus enn menn (p<0,001). Signifikant flere menn vurderte helsen som god etter hjerneslaget. Flere kvinner over 70 år brukte hjemmehjelp og hjemmesykepleie det siste året (p<0,001). Færre kvinner hadde venner som kan hjelpe dem (p=0,001).
Konklusjon: Det er ingen forskjell i funksjonssvikt mellom kvinner og menn etter hjerneslag. De fleste klarer seg uten hjelp til å vaske seg, dusje, kle på seg, legge seg, stå opp og spise. Flere kvinner vasker klær og lager mat, mens flere menn kjører bil. Kvinnene bor oftere alene, bruker hjemmehjelp og hjemmesykepleie. En viktig implikasjon for sykepleiepraksis er å tilrettelegge individuell tilpasset behandling og opptrening.
Introduction
In 2012, according to the Norwegian Cardiovascular Disease Registry, there were 19 211 incidents of main diagnosis acute stroke in Norway (1). This resulted in 4262 out-patient consultations, 14 949 hospital admittances, and 12 387 hospital stays, for 10 672 patients (1). Of these patients 5632 were men and 5040 were women. After 28 days 10.9 per cent of the men and 16.4 per cent of the women were dead (1). Mortality after a stroke was lower in 2012 in Nord-Trøndelag than in most other counties, and higher among women than men (2).
Stroke is the third most frequent cause of death, after coronary heart disease and cancer, (3) and is the most important cause of severe disability (4). The Norwegian Stroke Registry, in 2013 comprising 53 hospitals in the country (some 76 per cent of the patients), reports that two out of five have completely recuperated after the stroke (5). According to WHO, some 15 million people worldwide suffer a stroke annually; of these one third die and one third suffer severe disability (6). Mortality has decreased in Norway over the past ten years. Important causes of this reduction are assumed to be increased focus on stroke, both in the medical community and in the media, in combination with fast emergency treatment (7,8). In spite of increased emphasis on prevention in recent years, the number of strokes has not decreased (3,9). The proportion is expected to rise as life expectancy increases (10). An estimated 55 000 persons who have suffered a stroke are currently living in Norway (3).
The risk factors for suffering a stroke are many, and mostly the same for women and men, with high blood pressure being the most important (5,11). The risk is higher for men than for women in Norway and other Scandinavian countries (3). Men are, on average, younger than women when they suffer their first stroke: 75 years opposed to 78 years in women. The number of men and women living with stroke is approximately the same, as there are more women in the older population (3,7).
The most typical functional outcome following a stroke is one-sided paralysis in the extremities or face, loss of sensation, difficulties with swallowing or speech, vision impairment, balance problems, neglect, consciousness disturbances, psychical disorders, pain, and bladder and bowel dysfunction (4). Other consequences, which may impact functional ability, are fatigue, depression, anxiety, and sleep disorders (12,13). However, a longitudinal study was recently published addressing functioning and degree of functional independence following brain haemorrhage in patients at Sørlandet Hospital. The study showed that two out of three did not need assistance with daily routine activities after about four years (14).
The stroke in and of it self, and how the body functions after the stroke, will affect the health of those suffering a stroke, and this again may increase the need for health services. Earlier studies have shown that women have more physical outcomes and limitations in daily activities than do men (15). A European study of persons who had suffered a stroke and been admitted to hospital showed that women more frequently experienced reduced functional ability and higher disability at three months after the stroke than did men (16). Two Swedish studies have shown that women suffer from poorer health than men up to three months after a stroke (17,18).
Studies from America, Asia, and Europe confirm that being female may be an important factor in the outcome and functional ability, both immediately following and in the long run, after a stroke (16,19,20). Even though earlier studies suggest that women have poorer functional ability than men, the findings are not univocal. Several studies have shown no significant differences in functional ability between women and men following a stroke when controlling for age, severity of the stroke, and functional ability prior to the stroke (17,21,22). Norwegian researchers have shown that women found it difficult to manage practical tasks and fulfil their various roles after a stroke (23-26). This is in line with an American study that shows that sociocultural factors such as gender roles, social support, access to resources, and depression may explain women’s poorer health and functional ability after a stroke (27).
A Norwegian study from 1997 concludes that women appear to suffer a higher reduction in functional ability after a stroke than do men (28). It is difficult to find similar, later Norwegian studies of gender differences in health, functional ability, and use of health services after a stroke. Additional and new knowledge is important on this subject in the Norwegian population. The purpose of this study is thus to see whether women and men assess their health and functional ability differently after a stroke, and whether there is a difference between women and men in the use of health services after a stroke.
Method
The study is based on data from The Nord-Trøndelag Health Study, HUNT 3. All residents in the 24 municipalities were invited to participate. The study lasted from October 2006 to June 2008 (8). Some 93 860 persons qualified for participation and 54.1 per cent participated in HUNT 3.
The sample in this study consists of 1190 persons who have had a stroke or brain haemorrhage. Socio-demographic variables: Gender, age, marital status, living alone, and work activity.
To survey self-assessed health we asked: “How is your health at the moment?” The question had four alternative responses: “poor”, “not so good”, “good” and “very good”. The question is taken from the well-validated instrument SF-36, and is frequently used in self-assessment of health (29).
Functional disability
HUNT’s version of the modified Rankin scale (mRS) is used to assess functioning after a stroke (30). The first question is: “Have you completely recuperated after your last stroke?” with response alternatives yes or no. To the question: “If you have had a stroke, how does it affect your functioning level and your ability to do normal, daily tasks? Normal, daily tasks mean, for example, eating, dressing and going to the bathroom. ” There were six response alternatives, ranging from:0) No symptoms at all, 1) No significant disability despite symptoms,, with the explanation “have some symptoms, but am able to perform all tasks and activities as before the stroke”, 2) Slight disability, 3) Moderate disability, 4) Moderately severe disability and 5) Very severe disability. A mRS score of 0-2 corresponds to none to slight disability and is defined as independence (14,19). Moderate to very severe disability (mRS 3-5) is defined as dependence. mRS has been found to be valid and reliable in Norway and internationally (4,31). As few respondents scored 4 and 5, these categories were combined. Persons aged 70 or above were asked questions on what normal, daily tasks they could manage without help from others.
Use of health services
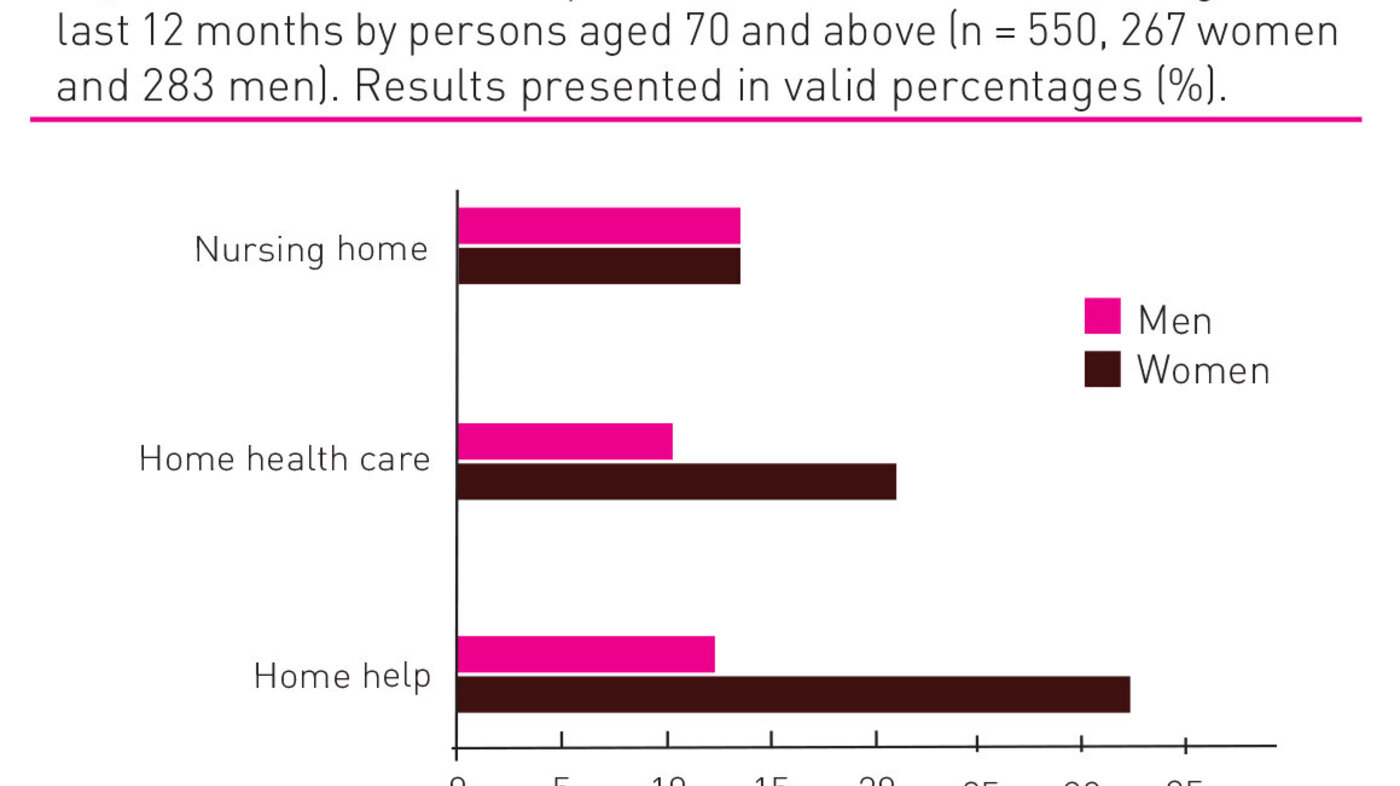
The questions address whether the participants had been admitted to hospital in the last 12 months, consulted a general practitioner, a specialist outside the hospital, a doctor without being admitted to the psychiatric out-patient department, consulted a doctor without being admitted to a hospital out-patient department (other than psychiatric department), consulted complementary and alternative medicine, chiropractor etc[LK1] . The participants were also asked whether they were admitted to hospital in connection with the last stroke they had suffered. Women and men aged 70 or above were asked if they had used home care help, home nursing care, or been admitted to a nursing home in the last 12 months. The variable “Do you have friends that can help you when you need them?” is also included. The response alternatives to all questions above were yes or no.
Other variables
Questions on whether the participants had used blood pressure medication, had a heart attack, angina pectoris, heart failure, other heart disease, atrial fibrillation or diabetes, and one question on whether they had pain that had lasted more than 6 months were included. The response alternatives were yes or no. Obesity as a variable is created from reported Body Mass Index (BMI). BMI is a continuous variable recoded as a dichotomous variable. BMI under 29.9 was given the value 0, and BMI > 30 is considered obese, and given the value 1. The question “How often do you exercise?” had the response alternatives “never”, “less than once a week”, “once a week”, “2-3 times a week”, and “nearly every day”.
Statistical analyses
Descriptive data analyses were performed. Continuous variables were analysed with t-test and presented with mean and standard deviation. Ordinal and categorical data were analysed with Chi-square test and the level of significance set to p<0.05. Where the questions had more than one value and the Chi-square test indicated statistical significance, we did a post hoc Bonferroni test. This entails that if, say, there are six possible hypotheses (i.e. 0.05/6), the p value must be <0.008 for the individual hypothesis to be considered statistically significant. Descriptive statistics are presented in frequency tables, figures, and described in the text. Data were analysed using the statistics programme SPSS version 22.
Ethics
This study has been evaluated and approved by the Regional Committee for Medical and Health Research Ethics (REC east C, no. 2012/2261), by the Norwegian Centre for Research Data in 2013, and was given permission to use data material from HUNT Research Centre in 2013.
Results
Table 1 shows the sample of 1190 respondents, with 572 (48.1 per cent) women and 618 (51.9 per cent) men. The average age was 68 years, and post hoc tests showed that there were no significant differences in age between women and men. The oldest woman was 95 years and the oldest man 88 years. More men were married or cohabited (80.9 per cent, p<0.001), whereas more women were widows (p<=0.001) or lived alone (p<0.001).
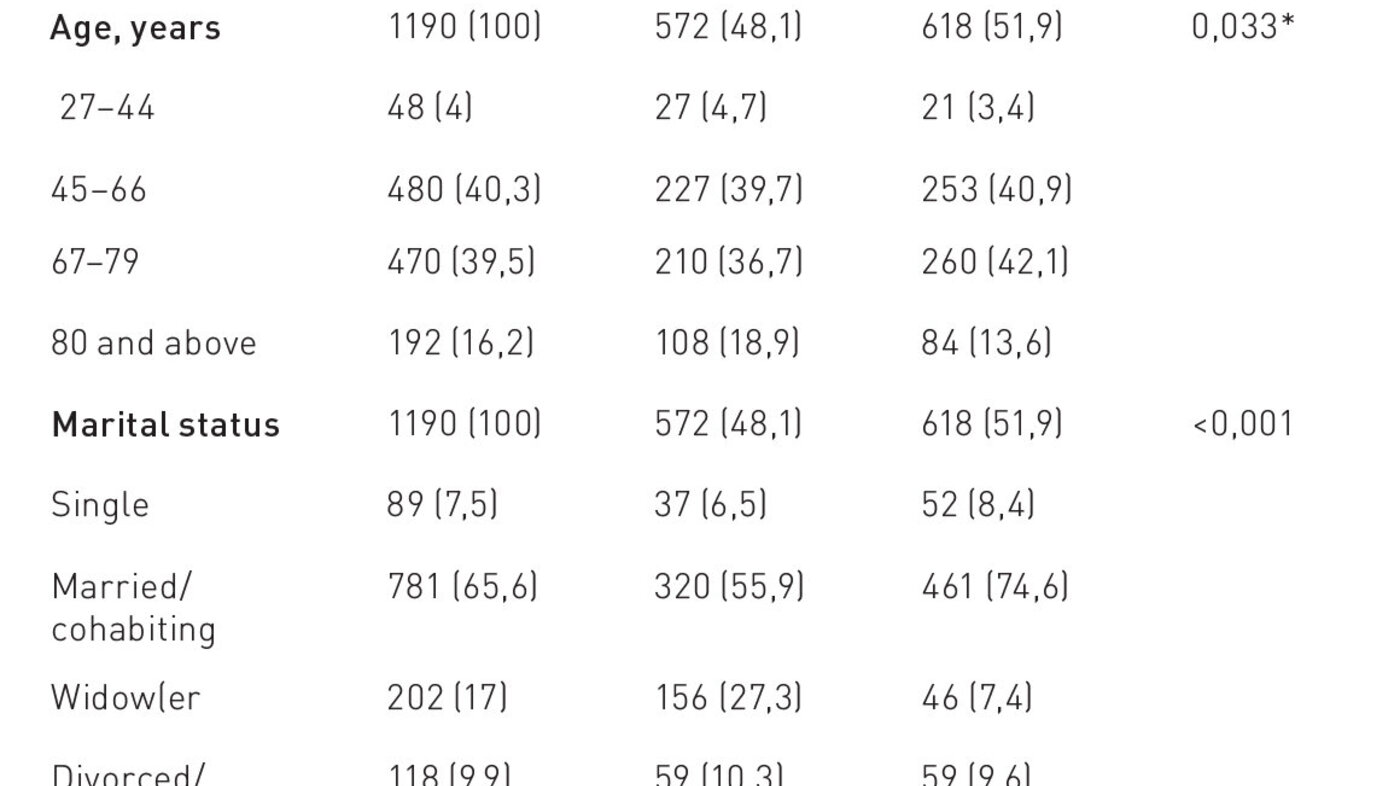
The average age at first stroke was 58 years (SD 14.4), and the median age was 60 years. Earliest reported stroke for both women and men in the sample happened before turning 1 year. There were no significant differences between women and men in number of strokes (p=0.682), as many as 79.9 per cent had suffered just one stroke. The majority were admitted to hospital when suffering their most recent stroke, but women were admitted less frequently than men: 77.8 per cent of the women and 85.9 per cent of the men (p=0.001). There was no difference between women and men in the use of blood pressure medication (p=0.450), incidence of atrial fibrillation (p=0.757), diabetes (p=0.135) or BMI (p=0.890). Around 30 per cent reported a BMI of more than 30. One fifth (20.5 per cent) reported exercising more or less daily, and 10 per cent reported that they never exercised. There was no significant difference between women and men in this. More men had had a heart attack, heart failure, and angina pectoris (p<0.001). More women had had long-term pain of more than six months’ duration compared to men, 60.1 per cent and 42.7 per cent respectively (p<0.001).
Table 2 shows how women and men assessed their own health, and the post hoc test showed that a significantly larger proportion of the men reported being in good health compared to the women.
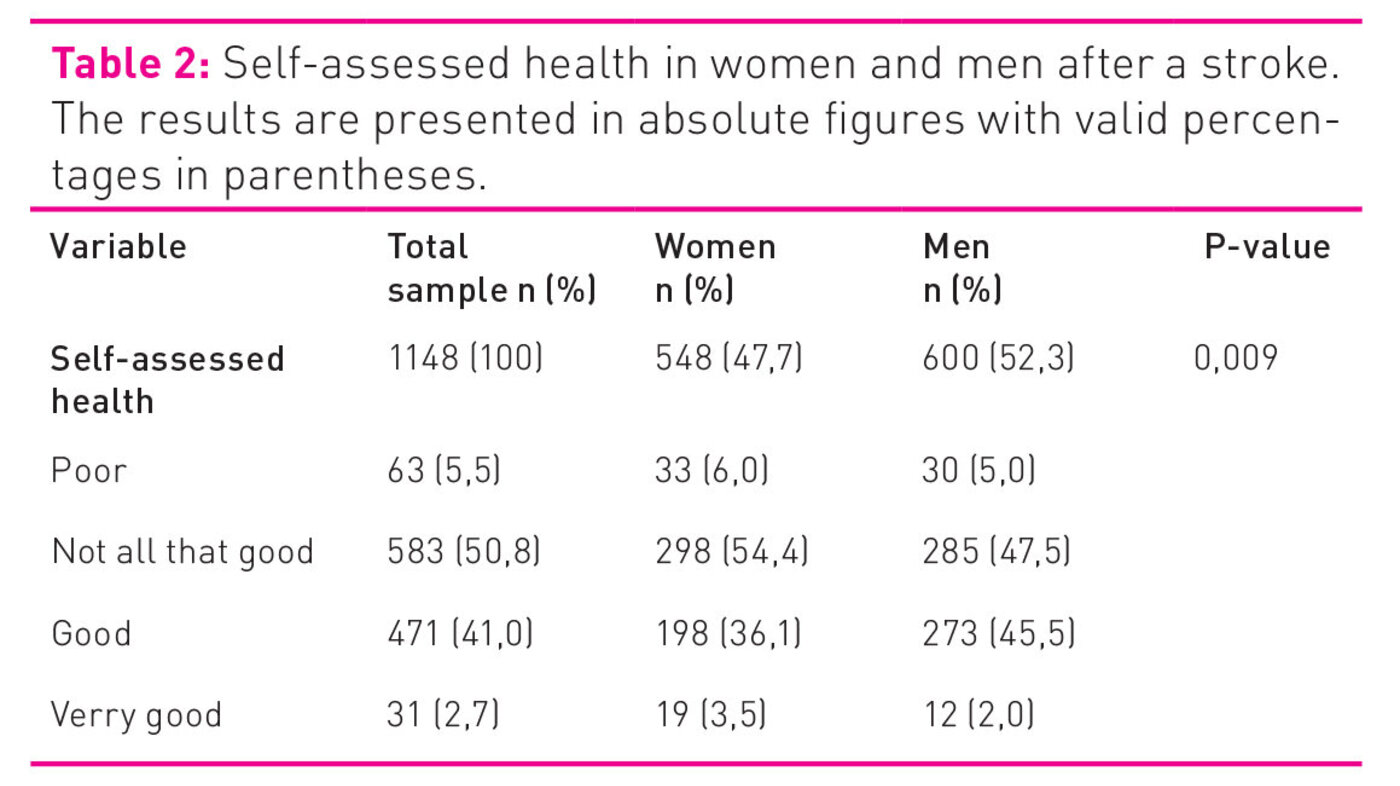
Table 3 shows that nearly ¾ of the total sample had completely recuperated after the most recent stroke (72.3 per cent), with no significant difference between women and men (p=0.595). Only 6.2 per cent reported moderate to very severe disability, with no significant difference between women and men.
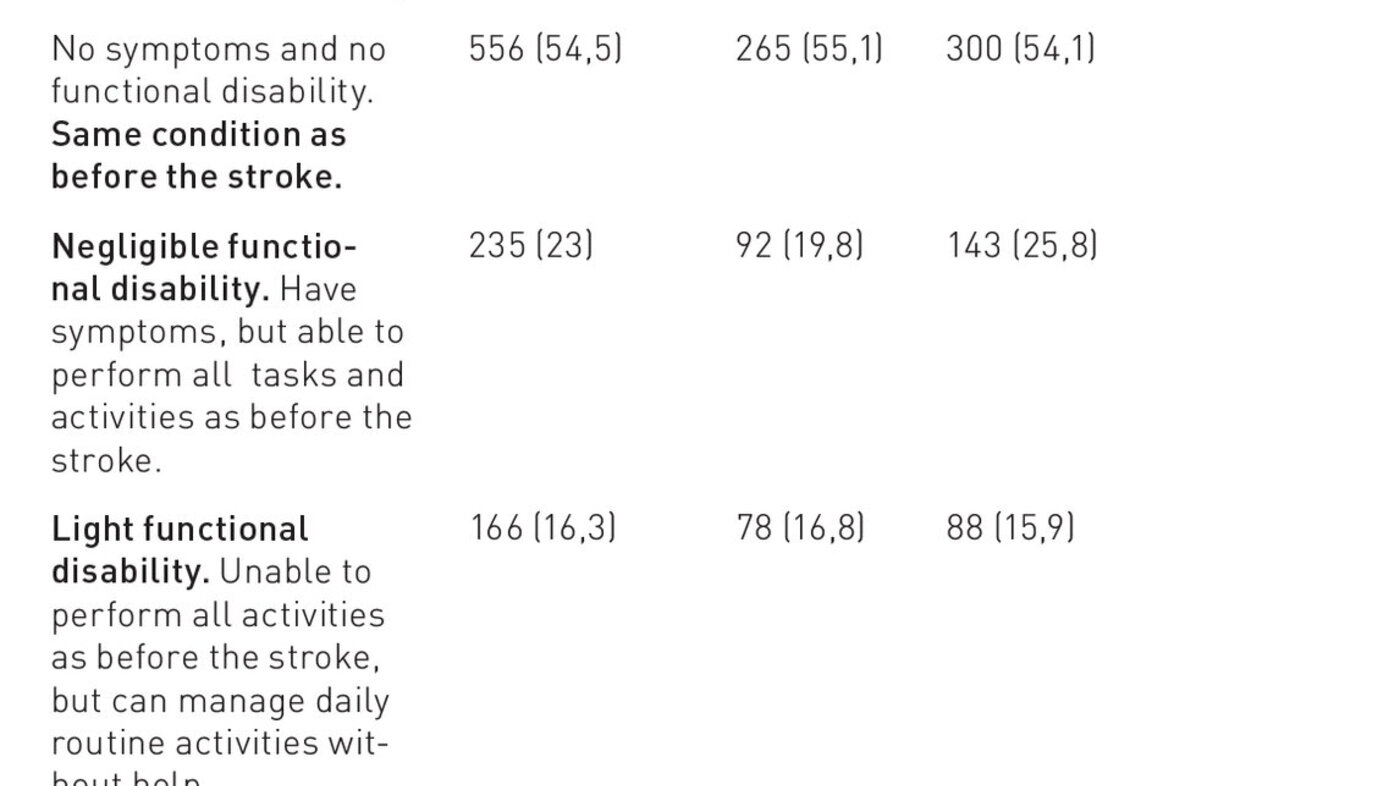
Figure 1 shows significant differences in the ability to manage normal, daily tasks between women and men > 70 years.
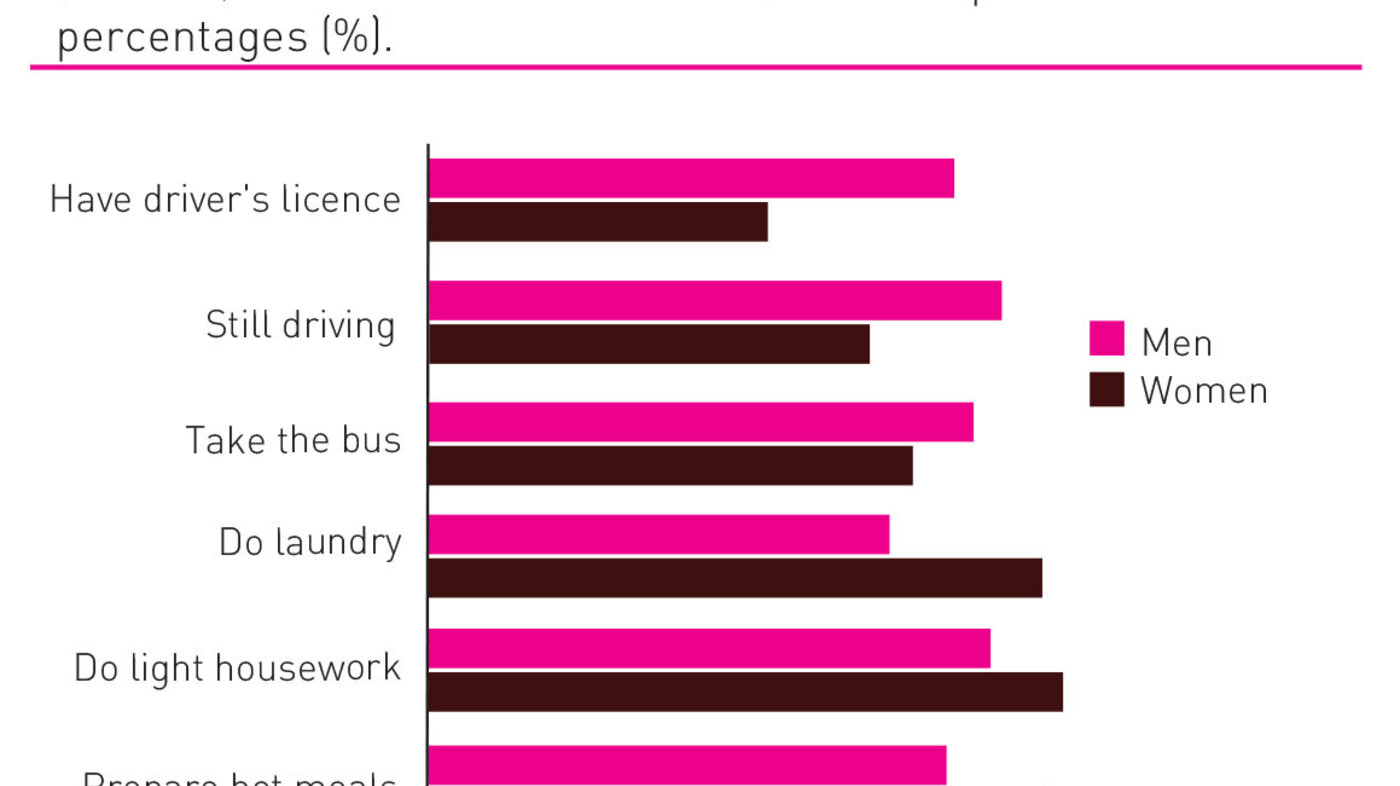
More than 90 per cent of both women and men answered that they were able, without help, to walk indoors on one floor, go to the bathroom, wash themselves, bathe or shower, dress, go to bed and get up, and eat. There were no significant differences.
There were no significant differences between women and men in the use of health services during the last twelve months, with the exception that women more often sought alternative treatment (p<0.001) and other medical specialist services (p<0.014). Figure 2 shows that significantly more women aged 70 and above used home care help (31.2 per cent women and 12.4 per cent men, p<0.001) and home nursing care (20.8 per cent women and 10 per cent men, p<0.001) during the past twelve months.
Discussion
This is one of few Norwegian studies to survey whether women and men assess their health and functional ability differently after a stroke, and whether there is any difference in the use of health services. An important finding is that as many as 72 per cent report having completely recuperated after their last stroke, which is good. Women and men both report a low level of disability; 92 per cent of the women and 96 per cent of the men report no significant disability to slight disability. This finding is unexpected as prior research from Norway and other countries has found that about every third person who has a stroke suffers varying degrees of disability (4,6,32). New figures from The Norwegian Stroke Registry show that in 2013 two out of five had completely recuperated three months after the stroke (5); this may suggest support for the present study’s figures. One explanation for so many participants reporting a low degree of reduction in functional ability may be that the Nord-Trøndelag Health Study consists mainly of people living at home. Earlier studies have often been based on patients admitted to hospital after a stroke, or nursing home residents. There are also other possible ways of interpreting these findings. In HUNT 3 the average age at the first stroke was 58 years, while the average age at participation in the survey was 68 years. Research shows that the effect on functional outcome may be mild (33), and some of this may disappear over time (34,35). Many respondents may also have adapted to any consequences of the stroke (36), and may thus not notice any small effects still remaining. Underreporting is also a possibility. One may also speculate whether the HUNT version of mRS does not catch “hidden and invisible outcomes” from the stroke, such as for instance depression, anxiety, light concentration difficulties, and sleep disorders. HUNT has changed the original instrument by excluding a concretisation of the response alternatives with examples.
The difference in disability between women and men in this study is negligible. This is in opposition to findings of earlier research that show that women suffer a greater degree of disability than men (19,21,37,38), also when adjusting for the seriousness of the stroke (37). Gender alone is, however, not a decisive factor for the degree of disability following a stroke.
In line with earlier research on women’s health in general and following stroke in particular, the women in this study report poorer health than the men (17,18,39-43). It is reasonable to assume that some factors are direct consequences of the outcome of the disease. Such consequences may be pain issues (4) as reported by the majority of women in this study. We have no basis for saying that there is a connection between the pain and the stroke, but it is important that health personnel address such issues in the encounter with the individual patient. A majority of the women in this study live alone, are single, and fewer women than men have friends that can help when needed. These are psychosocial factors that may contribute to explaining why women and men assess their health differently. Earlier studies have assumed that these are factors that affect women’s and men’s health differently (3,43).
Another important finding is that more women than men over 70 years of age depend on assistance for normal, daily tasks after a stroke, and use more home care help and home nursing care. There are several possible explanations for this. Fewer women than men have friends that can help them when needed and more women were widows and lived alone. This may help explain a greater use of home services by women.
In a gender role perspective it is not particularly surprising that more women than men reported being able to do laundry, light domestic chores, and prepare hot meals, and that more men had a driver’s licence, drove a car, and took the bus on their own. This is in line with findings that sociocultural factors such as gender roles and social support may explain the women’s poorer health and functional ability after a stroke (27). One may speculate whether different gender roles alone, and expectations of such different gender roles, may affect women’s and men’s assessment of their health after a stroke. It is nevertheless important to emphasise that in questions on independence in daily activities and tasks, such as washing themselves, dressing, food shopping and getting out, there is no difference between women and men in this study.
Strengths and limitations
One strength of this study is that the HUNT 3 has population data that include a large number of persons who have suffered a stroke. Valid questionnaires have been used and the data have been quality assured. The analyses build on these strengths, and pose research questions of clinical significance and implications. Some limitations of the study need discussing. In this cross-sectional study there is great variation in the time that has passed from a person’s most recent stroke. Information that is based on someone remembering across varying time spans is tainted by a great deal of uncertainty. This is why analyses to describe consequences after, say, one, two or ten years have not been performed. This would require a longitudinal design. Even if HUNT 3 has a relatively high response rate (54 per cent) (44), an analysis of the non-respondents indicates that these generally have weaker personal economy, higher mortality, and more chronic diseases, including stroke (44). Further, several non-respondents assessed their health as poorer and they had more frequently been admitted to hospital during the past twelve months (44). This entails that the most seriously ill stroke patients and those with the lowest socioeconomic status are not included in our study. The findings cannot therefore be considered representative for all people who have suffered a stroke. We assume that the findings may, with some caution, be generalised to healthier, home-residing persons with a fair personal economy, who have had a stroke. Nord-Trøndelag has a demography presumed to be fairly similar to the rest of the Norwegian population (8). Another limitation, however, is that these are self-report results, and it is possible that a lower outcome would have been the result in the case of medical testing of the patients.
Conclusion
This study shows no difference in disability between women and men after a stroke. It may, however, seem as if a stroke has a more negative effect on women’s health. It is worth noting that although the majority of the participants were admitted to hospital in connection with their most recent stroke, women were less frequently admitted to hospital than men. More women than men received home nursing care and home care help. Further research should investigate possible gender, psychosocial, or biological causes for such differences. Personal economy and number of chronic diseases are most likely significant, and should be included in future studies. Qualitative studies will be able to contribute to deeper insight into this issue. Health personnel need to be aware that women and men live somewhat different lives, and that this may affect how they assess their own health, and the rehabilitation and help they need after a stroke. An important implication for nursing practice is to facilitate individually adapted treatment and rehabilitation. Special attention should be paid to women, who more often live longer and alone, so that they more easily learn to manage daily activities and tasks after a stroke.
Acknowledgement
Data are taken from The Nord-Trøndelag Health Study (HUNT) – a collaboration between HUNT Research Centre (Faculty of Medicine, Norwegian University of Science and Technology (NTNU)), Nord-Trøndelag County Council, Central Norway Health Authority and Norwegian Institute of Public Health.
References
1. Duerr A, Ellingsen CL, Egeland G, Tell G, Seliussen I, Igland J, et al. Hjerte- og karregisteret. Rapport for 2012. Oslo: Nasjonalt folkehelseinstitutt; 2014. 42 s.
2. Norgeshelsa.no. Statistikkbanken. Dødsårsaker nøkkeltall hjerneslag kvinner, alle aldre 2012, per 100 000. (Nedlastet 20150826). Tilgjengelig fra: http://norgeshelsa.no./norgeshelsa/
3. Ellekjær H, Selmer R. Hjerneslag – like mange rammes, men prognosen er bedre. Tidsskr Nor Laegeforen. 2007;127:740-3.
4. Helsedirektoratet. Nasjonal retningslinje for behandling og rehabilitering ved hjerneslag. Oslo: Helsedirektoratet; 2010. 196 s.
5. Indravik B. En kort presentasjon og utdrag fra årsrapporten 2013: Kvalitetsregistre.no; 2014 (Nedlastet 20150825). Tilgjengelig fra:http://www.kvalitetsregistre.no/getfile.php/Norsk/Bilder/Offentliggj%C3…
6. World Health Organization. Global burden of stoke. Genève: World Health Organization; 2004. (Nedlastet 20150825). Tilgjengelig fra: http://www.who.int/cardiovascular_diseases/en/cvd_atlas_15_burden_strok…
7. Folkehelseinstituttet. Hjerneslag – årsaker og forebygging. Folkehelseinstituttet; 2012 (Nedlastet 20151030). Tilgjengelig fra http://www.fhi.no/artikler/?id=42974
8. Krokstad S, Knudsen MS. Folkehelse i endring. Helseundersøkelsen Nord – Trøndelag. HUNT 1 (1984-86), HUNT 2 (1995-97), HUNT 3 (2006-08). Levanger: HUNT forskningssenter; 2011. 213 s.
9. Kirkevold M. Hjerneslag. I: Kirkevold M, Brodtkorb K, Randoff AH, red. Geriatrisk sykepleie. God omsorg til den gamle pasienten. Oslo: Gyldendal Norsk Forlag AS; 2010 (s.407-17).
10. Engstad TT, Viitanen M, Ellekjær H. Epidemiology of stroke in the elderly in the Nordic countries. Incidence, survival, prevalence and risk factors. Nor Epidemiol. 2012;22:121-6.
11. Kvalitetsregistre.no. Hjerneslag (Nedlastet 20150825). Tilgjengelig fra:
http://www.kvalitetsregistre.no/resultater/hjerte-og-kar/norsk-hjernesl…
12. Bakken LN, Kim H, Finset A, Lerdal A. Stroke patients functions in personal activities of daily living in relation to sleep and socio-demograghic and clinical variables in the acute phase after first-time stroke and at six months of follow-up. J Clin Nurs. 2012;21:1886-95.
13. Kouwenhoven S, Kirkevold M. Å leve med depresjon etter hjerneslag. Sykepleien Forskning. 2013;4:334-42.
14. Tveiten A, Ljostad U, Mygland A, Naess H. Functioning of long term survivors of first-ever intracerebral hemorrhage. Acta Neurol Scand. 2014;129:269-75.
15. Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7915-26.
16. Di Carlo A, Lamassa M, Baldereschi M, Pracucci G, Basile AM, Wolfe CD, et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke. 2003;34:1114-9.
17. Eriksson M, Glader EL, Norrving B, Terént A, Stegmayr B. Sex differences in stroke care and outcome in the Swedish national quality register for stroke care. Stroke. 2009;40:909-14.
18. Glader EL, Stegmayr B, Norrving B, Terent A, Hulter-Asberg K, Wester PO, et al. Sex differences in management and outcome after stroke: a Swedish national perspective. Stroke. 2003;34::1970-5.
19. Kim J, Lee K, Roh H, Ahn M, Hwang H. Gender differences in the functional recovery after acute stroke. J Clin Neurol. 2010;6:183-8.
20. Petrea RE, Beiser AS, Seshadri S, Kelly-Heyes M, Kase CS, Wolf PA. Gender differences in stroke incidence and poststroke disability in the Framingham heart study. Stroke. 2009;40:1032-7.
21. Feigin VL, Barker-Collo S, Parag V, Senior H, Lawes CMM, Ratnasabapathy Y, et al. Auckland Stroke Outcomes Study. Part 1: Gender, stroke types, ethnicity, and functional outcomes 5 years poststroke. Neurology. 2010;75:1597-607
22. Naess H, Nyland HI, Thomassen L, Aarseth J, Myhr KM. Etiology of and risk factors for cerebral infarction in young adults in western Norway: a population-based case-control study. Eur J Neurol. 2004;11:25-30.
23. Eilertsen G. Forståelse av pasientens livsprosjekt – en nøkkel i slagrehabilitering? Tidsskrift for omsorgsforskning. 2015;1:27-37.
24. Eilertsen G. «Alt er som før, men ingenting er som det var»: gamle kvinners opplevelse av livet etter hjerneslag. (Doktoravhandling). Universitetet i Oslo. Oslo. 2005.
25. Kvigne K, Kirkevold M, Gjengedal E. Fighting back-struggling to continue life and preserve the self following a stroke. Health Care Women Int. 2004;25;370-87.
26. Kvigne K, Kirkevold M. Living with bodily strangeness: Women´s experiences and their changing and unpredictable body following a stroke. Qual Health Res. 2003; 18:1291-310.
27. Turtzo LC, McCullough LD. Sex differences in stroke. Cerebrovasc Dis 2008;26:462-74.
28. Wyller T, Sødring K, Sveen U, Ljunggren A, Bautz-Holter E. Are there gender differences in functional outcome after stroke? Clin Rehabil. 1997;11:171-9.
29. Bowling A. Just one question: If one question works, why ask several? J Epidemiol Community Health. 2005;59:342-5.
30. HUNT 3. MRS Modified Rankin Scale 2015 (Nedlastet 20150825). Tilgjengelig fra: https://hunt-db.medisin.ntnu.no/hunt-db/#variab3611.
31. Goldstein LB. Use and utility of stroke scales and grading systems. UpToDate. (Oppdatert 20150305; nedlastet 20150825). Tilgjengelig fra: http://www.uptodate.com/contents/use-and-utility-of-stroke-scales-and-g… – H20964997.
32. Fjærtoft H, Indredavik B. Kostnadsvurderinger ved hjerneslag. Tidsskr Nor Laegeforen. 2007;127:744-7.
33. Kristensen H, Post A, Poulsen T, Jones D, Rosenbek Minet L. Subjective experiences of occupational performance of activities of daily living in patients with mild stroke. Int J Ther Rehabil. 2014;21:118-25.
34. Tveiten A. Intracerebral Hemorrhage In Southern Norway. A study of incidence and outcome. (Doktoravhandling). Universitetet i Bergen, Bergen. 2013.
35. Kjork E, Blomstrand C, Carlsson G, Lundgren-Nilsson A, GC. Daily life consequences, cognitive impairment, and fatigue after transient ischemic attack. Acta Neurol Scand 2015.
36. Brunborg B, Ytrehus S. Sense of well-being 10 years after stroke. J Clin Nurs. 2014;23:1055-63.
37. Lisabeth L, Reeves M, Baek J, Skolarus L, Brown DL, Zahuranec D, et al. Factors infuencing sex differences in poststroke functional outcome. Stroke. 2015;46:860-3.
38. Gall SL, Tran PL, Martin K, Blizzard L, Srikanth V. Sex differences in long-term outcomes after stroke: functional outcomes, handicap, and quality of life. Stroke. 2012;43:1982-7.
39. Kuhlmann E, Annandale E. The palgrave handbook of Gender and healthcare. Hampshire UK: Palgrave Macmillan;2010.
40. Sosial- og helsedepartementet. Kvinners helse i Norge. Oslo. Statens forvaltningstjeneste. NOU 1999:13.
41. Schei B, Sundby J. Kjønn og helse – begreper og modeller. I: Bakketeig LS, Schei B, red. Kvinner lider – menn dør: Folkehelse i et kjønnsperspektiv. Oslo: Gyldendal Norsk Forlag AS; 2007 (s. 33-49).
42. World Health Organization. Women and Health. Today´s Evidence, Tomorrow´s Agendas (Internett). Geneva: World Health Organization; 2009. 7s.
43. Appelros P, Stegmayr B, Terent A. A review on sex differences in stroke treatment and outcome. Acta Nevrol Scand. 2010;121:359-69.
44. Langhammer A, Krokstad S, Romundstad P, Heggland J, Holmen J. The HUNT study: participation is associated with survival and depends on socioeconomic status, disease and symptoms. BMC Med Res Methodol. 2012;12:1-14.









Comments