Co-ordinated collaborative meetings as patients transition from the psychogeriatric health service
Collaborative interdisciplinary meetings may increase the mutual respect between health professionals and provide more knowledge about the patient.
Background: For many years, co-ordinated collaboration has been a challenging issue for the health and social services, nationally and internationally. In the mental health sector it has been particularly difficult to identify initiatives that might ensure continuity of care as patients transition from the specialised health service and into the primary health service.
Purpose: The purpose of this study was to examine the experiences of health care professionals across the disciplines when attending collaborative interdisciplinary meetings held two weeks after the patient had been discharged from the specialised psychogeriatric health service and into nursing homes.
Method: This sub-study forms part of a larger participation-based research project, PASSUS, which looks into quality development and actions. This project focuses on patient-oriented interaction at the point of discharge into nursing home care and involves one psychogeriatric hospital department and four nursing homes. It looks specifically at one of the improvement measures: co-ordinated collaborative meetings. The study has a descriptive qualitative design and is based on written notes from twelve such collaborative meetings.
Results: Our analysis of the material suggests that the participants’ descriptions can be grouped in four summary categories: 1) information about individualised care and treatment, 2) knowledge exchange, 3) mutual recognition and affirmation, and 4) improvement measures.
Conclusion: The study involved meetings between the health care personnel who had been responsible for the follow-up of patients in the psychogeriatric department, and those who took over this responsibility for the patient in the nursing home. Our analysis showed that the collaborative meetings contributed to interdisciplinary knowledge exchange, as well as increased understanding and insight into the patient’s situation. The collaborative meetings show how co-ordinated systematic interaction can boost competence levels and ensure continuity of care between service sectors.
In recent years, co-ordination issues have received increased attention in Norwegian health policy (1) and research (2, 3). The national health and care plan for 2011–2015 revealed that many patients still experience discontinuity of treatment. Inadequate continuity of care may give rise to insecurity, provision of incorrect treatment and care, inefficient services and a reduced quality of life for patients and their relatives (4).
In 2013 the Norwegian Directorate of Health issued a circular concerning national objectives and priorities within the health and care services (5). It was pointed out that discontinuity of care and disrupted service provision, as well as inadequate communication, often occurs at the point of transition between hospital and nursing home. Regional health trusts were asked to follow up collaboration agreements and to “facilitate co-operation and dialogue meetings involving the primary health service, the specialised health service and other service providers” (author’s italics) (5, p. 21).
Health care personnel across all disciplines and service sectors must give due attention to information transfer in order to ensure that good and health-promoting relationships are sustained between patients and health professionals throughout the course of the patient’s treatment (4). The exchange of knowledge, information and experiences in connection with the hospital discharge process is of great importance to the continued development of services, the continuity of care and a medically acceptable patient progression.
Co-ordinated collaboration in the mental health services
Serious mental disorders in the elderly are often complex in nature (6). When patients are in the vulnerable phase of being transferred from a psychogeriatric hospital ward to a nursing home, the challenge is to ensure that health care personnel work in partnership in order to avoid discontinuity of interventions, relationships, objectives and treatments (5). Earlier research shows that successful interaction between the different parts of the mental health service can be brought about by influences from the system level, organisational level and interpersonal level (3).
Individual service providers can deliver collaborative interaction if the premise for interdisciplinary collaboration has been established at the organisational level. There are reciprocal influences at work between the education system, the organisation of the healthcare system, government policies, ideologies, structures, resources, shared objectives, and the willingness to co-operate and communicate (7–10).
Co-ordinated collaboration involves more specific commitment than co-operation. The concept involves a commitment to do something together in order to ensure that the work processes are streamlined and that services and measures are co-ordinated (11–13). This requires colleagues to make mutual adjustments to their respective jobs. Collaboration amongst individuals requires “trust, reciprocity and equality” and a shared understanding of the situation (11, p. 257).
Description of the study
This is a qualitative study which forms part of a larger participation-based research project entitled PASSUS (patient-oriented collaboration at the point of discharge into nursing homes) (14), set up to study quality development and actions. The objective of PASSUS is to develop and test a new collaborative model that might improve the discharge process, the continuity of care and the exchange of information between psychogeriatric hospital departments and sheltered or long-stay nursing home units at personal and system levels (14, 15).
One of the improvement measures put forward in the collaborative model was to conduct collaborative meeting across disciplines and service sectors at the nursing home two weeks after discharge (14). The purpose of this sub-study was to examine the experiences of the health care professionals who attended these collaborative meetings. The sub-study was restricted to descriptions submitted by participating health care personnel of their own role and professional contribution to an interactive process.
Method
The study has a descriptive qualitative design and is based on written notes from twelve collaborative meetings. The meetings were held at the nursing homes approximately two weeks after the patient had been discharged from the psychogeriatric hospital ward. Every collaborative meeting was attended by at least one specialist nurse and one psychiatrist from the hospital, as well as at least one nursing home doctor, primary contact or manager.
The collaborative meetings accommodated a mutual exchange of information concerning the patients’ symptoms and functioning in their new surroundings. The forum was used to discuss how the transfer of information had worked, and whether the measures proposed by the psychogeriatric service had proved effective. After each meeting, all participants would complete a self-reporting form by answering the following open-ended questions:
- What were your contributions to the collaborative meeting?
- What are your thoughts about the collaborative meeting?
- What have you learnt?
The questions had been drawn up in liaison with representatives of the nursing homes involved and the work group that had been set up at the psychogeriatric department as part of the preparations for PASSUS (14).
Sample
We recruited the responsible doctor or psychiatrist from the psychogeriatric department as well as a specialist nurse who was familiar with the relevant patient, and who had been involved with discharging the patient into the nursing home. We further recruited a nursing home doctor, primary contact or manager who had come to know the patient after the transfer to the nursing home. All participants were required to be proficient in writing in Norwegian.
We included 10 participants from the psychogeriatric hospital department and 26 participants from nursing homes. There were 27 females and 9 males, all of them health professionals from a wide range of backgrounds (table 1).
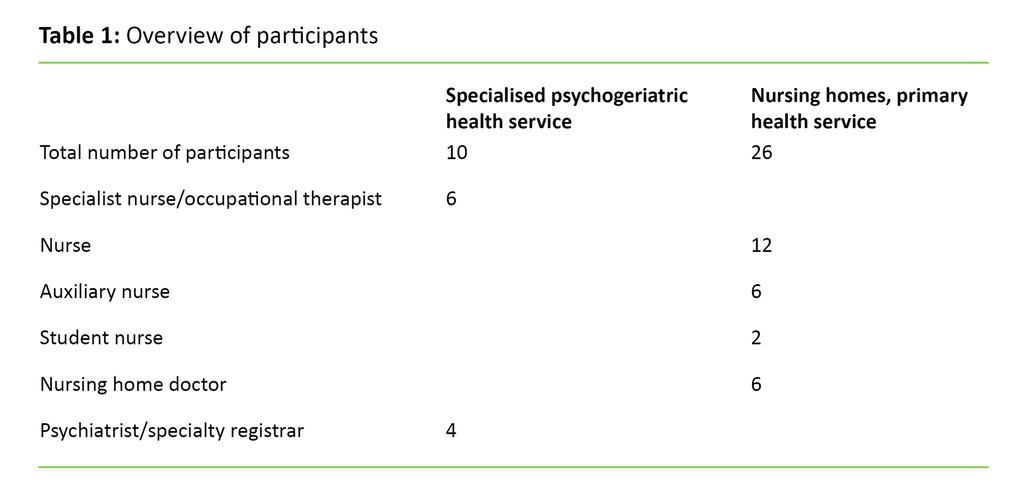
Data collection
We set aside a full hour for each of the collaborative meetings. Data were collected through self-reporting forms that were handed in immediately after each meeting. The full body of data consists of 80 such forms. The participants responded in handwriting on paper, formulating short sentences and keywords. These handwritten responses were transcribed verbatim and transferred to electronic media. The resulting electronic text makes up the study’s 36 pages of data.
Ethical considerations
The study was approved by the health trust’s data protection officer and by senior management at the nursing homes. We obtained written consent from all participants prior to the collaborative meeting. They were informed that participation was voluntary. No-one dropped out before completion. All information that emerged was securely treated in accordance with Norwegian Personal Data Act and the Data Protection Authority’s guidelines (18, 19). This meant that all self-reporting forms containing names were de-identified. There is no code list of names and contact details.
Analysis
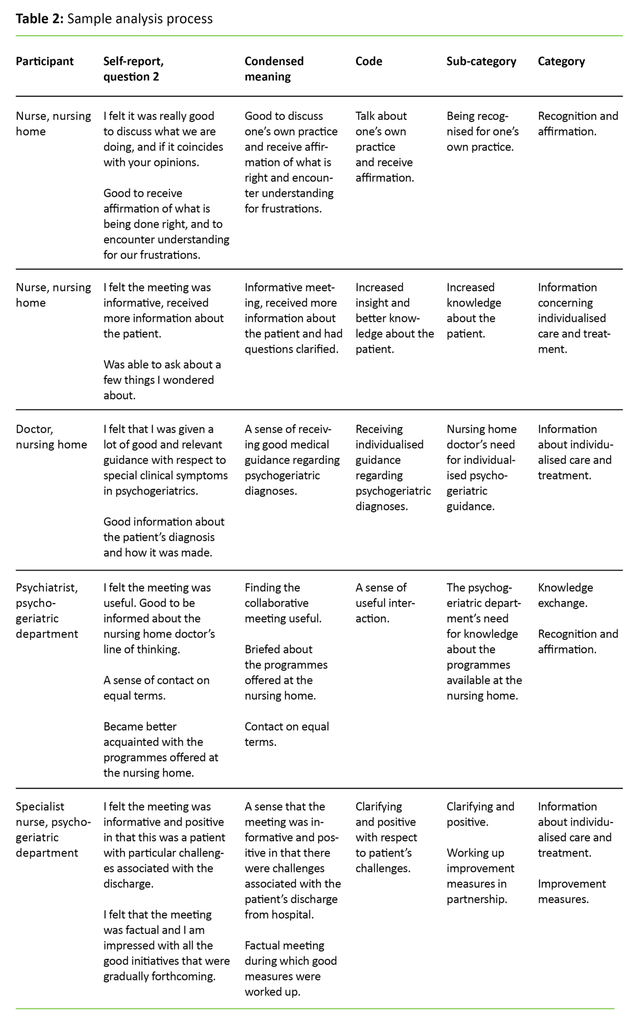
We conducted a qualitative content analysis of our material, inspired by Graneheim and Lundman (16, 17). The hallmark of a qualitative content analysis is a process that moves back and forth between the whole material and its parts. The text may be interpreted at a variety of levels; we chose the manifest level of analysis (16). This means that our interpretations were closely linked to that which is explicitly expressed in the material. Each self-reporting form was therefore identified as a unit of analysis.
We conducted the analysis in multiple stages, the first involving a read-through of the electronic data generated by each participant. We also read the whole material for each of the self-reporting questions in order to gain an understanding of the complete body of data. At the next stage we condensed the text. Examples of this process are set out in Table 2. Similar meanings were grouped in sub-categories before being allocated to four main categories. We conducted the analysis several times in order to ensure a uniform process. The sub-categories represent different aspects of a category (16, 17).
Results
From our analysis of the material four categories emerged that summarised the participants’ descriptions: 1) information about individualised care and treatment, 2) knowledge exchange, 3) mutual recognition and affirmation, and 4) improvement measures.
Information about individualised care and treatment
The psychogeriatric nurses reported that they chaired the collaborative meetings and that they provided patient information that complemented the written transfer report: “I have provided more specific details about interventions that had been inadequately described in the nursing summary – such as the administration of medication, the patient’s behaviour and moods.”
Health care personnel from the specialised health service highlighted the exchange of information concerning their experience of working with the patient’s relatives, and activity programmes that had been implemented to good effect. Nurses and occupational therapists alike reported that complex needs made it difficult to summarise the care provided in writing: “This is a patient with many needs which are difficult to describe” (psychogeriatric nurse).
The nursing home staff on the other hand, reported that the transfer information provided by the psychogeriatric department at the time of discharge was good and comprehensive: “I have received good descriptive information about the patient’s condition as well as an action plan that was ready for immediate implementation when the patient arrived here” (nursing home nurse). The health care personnel at the nursing homes also reported that they had followed up on the proposed measures: “I have followed up with specific measures at meal times and when providing personal care, and by creating a sense of calm around the patient. This has worked very well” (auxiliary nurse at nursing home).
The nursing home doctors reported that during the collaborative meetings they had a different focus than other professional groups. They sought supplementary information from the psychiatrist about the background to the diagnosis, the assessment, case history and medical treatment: “I raised questions concerning the medication.” The psychiatrist from the psychogeriatric department reported having provided in-depth information and having given her reasons for her choice of medical treatment: “I have explained the history, the medication and MR findings.” The nursing home doctors described the information provided in the medical discharge summary as good. A number of nursing home doctors reported that they contributed with supplementary information concerning the patient’s case history prior to hospitalisation at the psychogeriatric ward, and that they planned the continued treatment in partnership with the doctor or psychiatrist from the psychogeriatric department.
Knowledge exchange
A number of participants described receiving useful information about the patient through the interdisciplinary knowledge exchange at the collaborative meetings, and that they gained new insight into how it might be possible to interact with the patient in a good way. Particularly the nursing home doctors reported that they acquired more knowledge about psychogeriatric assessment methods and treatments: “I learnt more about the assessment methods.” Another nursing home doctor reported: “I have acquired insight into the treatment of Lewy body dementia: advice about what should be at the back of my mind in special cases. Have received an update.” The psychiatrist from the psychogeriatric department reported that she had acquired new knowledge about available support of significance to the transition into sheltered nursing home accommodation. This individual had also gained greater respect for the working practices at the nursing home.
Recognition and affirmation
The participants described their discussions during the collaborative meetings as frank exchanges conducted on equal terms: “I felt that the discussion was good and frank. Nursing staff were given a good opportunity to describe their observations of the patient. Everyone listens to one another” (nursing home doctor). Both the nurses and the nursing auxiliaries felt it was very useful to review the measures that work, and to give each other credit. They reported as follows: “it feels good to receive recognition for what is being done the right way [in the nursing home], and whether this coincides with your views [in the psychogeriatric department]”.
The psychogeriatric nurses reported that openness surrounding challenges was seen as particularly important. This was confirmed by the nursing homes. One person reported that: “I felt we received affirmation that what we are doing is not wrong, and that our frustrations were met with understanding” (nursing home nurse). A number of participants from both the psychogeriatric department and the nursing homes reported a good atmosphere at the collaborative meetings, and a sense that the participants were engaged. One participant gave a different account of one particular meeting where few people had been in attendance: “I felt it was not particularly motivating because few people contributed to the discussion and we appeared to run out of things to say” (psychogeriatric nurse).
Some described the discussions about challenging situations as being useful and informative, and based on a wish to do their very best for the patient: “The meeting was clarifying and very positive in that this was a patient with great challenges. I felt that the meeting was factual and I am impressed with all the good initiatives that were gradually forthcoming” (psychogeriatric nurse).
Health care personnel from the psychogeriatric department reported that it was good to receive feedback and confirmation that the patient’s needs were being met, and that the measures suggested by their department were being followed up. A number of doctors from the specialised health service reported that they had gained an insight into the work of nursing homes: “[G]ood to learn how the nursing home doctors are thinking with respect to medication and the patient’s condition. Am now better informed with regard to the programmes offered at the nursing home.” Health care personnel working for either service provider reported that they received mutual acknowledgement, irrespective of their occupation.
Improvement measures
The supplementary descriptions of the patient’s situation and the dialogue with health professionals with different experiences, helped to solve problems: “I started getting ideas about how to improve the things we do . It was a real boost for me” (nursing home nurse). It was emphasised that interdisciplinary dialogue can contribute to raising the participants’ competence levels, which might influence the patient’s future care: “[T]his kind of meeting will raise our level of competence, so that we jointly can come up with initiatives designed to maintain the patient’s identity and dignity” (student nurse at nursing home).
Several participants reported that the collaborative meetings constituted an important improvement measure in terms of ensuring the continuity and quality of care for elderly people suffering from mental disorders, and they wanted the practice to continue. Health care personnel from the psychogeriatric department reported that the collaborative meetings had brought to their attention that some of the nursing homes were struggling for too long before patients were admitted to hospital for assessment. They asked whether this could possibly be changed: “In the future I feel it would be wise for nursing home doctors to have an open line of communication to the specialised health service” (psychiatrist at the psychogeriatric department).
Discussion
This study looks at a group of health professionals who attend co-ordinated collaborative meetings. The meetings involved a level of commitment and focused on an exchange of knowledge that may contribute to better continuity of care between psychogeriatric hospital departments and nursing homes. Co-ordinated collaboration between health care personnel in the specialised health service and the primary health service is often taken for granted, and the responsibility for ensuring continuity of care has received growing attention after the introduction of the Coordination Reform (1, 3). A number of studies have also pointed to the need for new approaches (2, 3).
Previously, elderly patients suffering from complex mental disorders and dementia used to be assessed and treated during lengthy periods of hospitalisation in psychogeriatric departments. These days, the requirement is for outpatient services, nursing home adaptations and as few inpatient nights as possible. In compliance with the Coordination Reform, the psychogeriatric hospital services have become more specialised and focused on assessment. This is why there are complex interactions and decision-making processes involved with the transfer of patients from psychogeriatric hospital departments to nursing homes. Furthermore, there is a risk of discontinuity of care (3). Demands for knowledge-based practice ensure that care and treatment are provided on the basis of research-based knowledge and adjusted to the individual patient’s resources and wishes (1).
The study shows that interdisciplinary health care personnel at nursing homes felt they were receiving useful information from the medical discharge summaries and nursing summaries when patients were transferred from the psychogeriatric service. The nursing home doctors nevertheless often asked for assessment details and the reasoning that formed the basis for drug treatment choices. The attention of the nursing staff was to a greater extent directed towards the patient’s basic needs. All professions were able to contribute to the exchange and put forward suggestions from their own viewpoint, and it was useful to exchange knowledge.
Recognition and affirmation are important
Health care personnel from both service sectors reported that the collaborative meetings provided affirmation of their own work. Affirmation arises in the moment and is all about the way we listen, our attitude to other people and how an individual’s overall behaviour appears as they encounter other people. Affirmation relates to our appreciation of another person as an individual and the acceptance and validation of this other person’s experiences (22, 26).
An earlier psychogeriatric study conducted by Brattrud and Granerud (10) shows that it may be challenging for personnel within the primary health service and the specialised health service to see each other as equal partners (10). In our study, the health professionals from the specialised hospital department were described as “experts” by the nursing home staff, which may suggest that there is an informal hierarchy in place. Nevertheless, it appears that the health care personnel saw each other as equal participants. We interpret this to mean that each participant attending the collaborative meetings felt confident about their own background, which matches the findings of earlier research on individual factors that are essential to good co-operation (12, 26).
Another interpretation may be that those who attended the collaborative meetings focused their attention on the patient’s health and treatment. In other words, equality is linked to equality of experience, as all participants had some knowledge of the patient. They felt it was really useful to listen to each other and to meet up face-to-face as interdisciplinary partners. Earlier studies have also shown that meetings are conducive to co-operation and to ensuring a good flow of information (2, 25). It is therefore useful to highlight various aspects of the interactions that may serve to enhance the level of continuity and collaboration, and encourage learning from the experiences.
Exchanging experiences
The interdisciplinary nature of the interaction between health care personnel was an important factor. The collaborative meetings in our study were characterised by exchanges of relevant medical information and in-depth descriptions of the care provided for the individual patients. Our findings show that the exchange of experiences gave participants new knowledge about the patient and an insight into each other’s service areas. Other studies point out that the specialised health service and the primary health service represent different approaches in terms of ideology, culture, resources and competence, and that this may prove to be an obstacle to collaboration (3). Nevertheless, our study showed that the participants included each other on equal terms.
Earlier studies have demonstrated that collaboration is greatly enhanced by regarding each other as “we” rather than “us and them” (9). In their study from the Swedish mental health service, Magnusson and Lützén (9) found that different views and focus in the approach to people with mental health problems may be obstructive to co-operation and interaction. The same applies if the health care personnel involved make use of different concepts, expressions and terminology within the field (9).
The health care personnel who took part in the study reported that one particular collaborative meeting was not considered useful. This may have been caused by disrupted dialogue and misunderstandings (22). Dialogue disruptions may be attributed to attitudes or insufficient engagement, or a poor sense of belonging or community (22). According to Goffman (21) the emotional response among participants is a third significant factor in focused social meetings. Meeting each other in person allows the participants access to a number of social clues in the form of words, facial expressions, gestures and actions. In the light of Goffman (21), our findings may suggest that the participants tried to “build bridges” to one another in the interest of doing their utmost for the patient.
Different resources and different requirements
Earlier studies have pointed out that specialised health services and nursing homes have different resources and different competencies available to them (24). Within the context of a hectic working day at a nursing home, it may be challenging to follow up the residents’ developing needs to ensure that the appropriate measures are put in place (24). Participating health care personnel from either service sector described it as challenging to identify suitable measures for individual patients. During the meetings they exchanged knowledge and provided mutual affirmation of each other as resource persons.
The detailed descriptions provided by participants through the questionnaires, told us that the participants became better acquainted with the physical circumstances, resources and competencies provided at the various nursing homes and in the specialised health service. This type of mutual knowledge exchange helps the health professionals realise when there is reason to seek or provide advice and guidance (10).
In order to be able to provide health care which is medically sound, health care personnel must be able to interact with members of other health care professions (11). Equally, knowing each other’s competence and services will enable mutual understanding and recognition of one another’s differences. Willumsen (12) points out that recognition of differences is a factor that may encourage dynamic collaboration. This requires health care personnel to be flexible and capable of taking advantage of each other’s contributions. Willumsen (12) argues that good interdisciplinary co-operation requires members of different professions to work in partnership on a joint task, with everyone contributing on equal terms. Our study demonstrated that a shared understanding of the patient’s situation helped the health professionals jointly draw up detailed interventions for the patient’s future nursing care.
The study’s limitations and strengths
There are some limitations to the study. It was based on a limited number of written feedback reports from a specific geographic area. The body of data consists of written responses to three questions and the participants’ ability to express themselves clearly in writing differs. The researchers have not had the opportunity to follow up with further questions.
The timing and location of the collaborative meetings may have influenced the results. They were all held after the patient’s discharge from hospital to ensure that both parties would be familiar with the patient and had made their own observations. The meetings were held at the nursing homes in order to boost participation levels. We presumed that it would be difficult for nursing home staff to travel to the hospital, as few staff are assigned to a shift.
It is one of the study’s strengths that six different healthcare professions are represented, and that the questions were drafted in liaison with the target group. The study raises important points, corroborates the need for co-ordinated collaborative meetings and highlights themes of universal significance. A relatively low number of participants, and the data collection method, represent limitations to the study’s transfer value.
Our study does not discuss co-ordinated organisational collaboration, but we have communicated our sub-project findings to the main PASSUS project. This resulted in written guidelines being issued with respect to the collaboration between nursing homes and the psychogeriatric service. Neither patients nor their relatives were included as study participants. In future research, it will be important to include interaction with these key groups.
Conclusion
This study involved meetings between health care personnel who had been responsible for the care of patients in the psychogeriatric department, and those who took over responsibility for the patient in the nursing home. Our analysis of the participants’ self-reported experiences showed that the collaborative meetings contributed to interdisciplinary knowledge exchange, as well as increased understanding and insight into the patient’s situation. It was important for health care personnel at the nursing homes to receive detailed information about the psychogeriatric assessment and the reasoning behind treatment choices, while also receiving affirmation of their work.
The health care personnel in the psychogeriatric department reported that the feedback received from health care personnel at the nursing homes was significant to their practice. The collaborative meetings contributed to mutual respect and the exchange of detailed, patient-oriented knowledge. They are examples of how systematic collaboration can improve the individual’s competence and ensure continuity of care between service sectors.
References
1. Helse- og omsorgsdepartementet. St.meld.nr. 47 (2008–2009). Samhandlingsreformen. Rett behandling – på rett sted – til rett tid. Oslo.
2. Elstad TA, Steen TK, Larsen GE. Samhandling mellom et distriktspsykiatrisk senter og kommunalt psykisk helsearbeid: Ansattes erfaringer. Tidsskrift for psykisk helsearbeid 2013;10(4):296–305.
3. Olsen BM, Vatne S, Buus N. Kontinuitet og samhandlingsutfordringer i psykiske helsetjenester – en fokusgruppestudie. Klinisk Sygepleje 2015;29(4):55–68.
4. Helse- og omsorgsdepartementet. Nasjonal helse- og omsorgsplan for 2011–2015. Oslo. 2011.
5. Helsedirektoratet. Nasjonale mål og prioriterte områder for 2013. Rundskriv til kommunene, fylkeskommunene, de regionale helseforetak og fylkesmennene fra Helsedirektoratet, Oslo. 2013.
6. Engedal K, Haugen PK et al. Demens: Fakta og utfordringer. Forlaget Aldring og helse, Tønsberg. 2009.
7. San Martin-Rodriguez L, Beaulieu M-D, D'Amour D, Ferrada-Videla M. The determinants of successful collaboration: A review of theoretical and empirical studies. Journal of Interprofessional Care 2005;1:132–47.
8. Bramesfeld A, Ungewitter C, Bottger D, El Jurdi J, Losert C, Killian R. What promotes and inhibits cooperation in mental health care across disciplines, services and service sectors? A qualitative study. Epidemiology and Psychiatric Sciences 2012;21:63–72.
9. Magnusson A, Lützén K. Factors that influence collaboration between psychiatric care and CSSs: experiences of working together in the interest of persons with long-term mental illness living in the community. Scand J Caring Sci 2009;23:140–5.
10. Brattrud TL, Granerud A. Sammen om gode overganger. Samarbeid mellom kommunene og spesialisthelsetjenesten i psykisk helsevern. Tidsskrift for psykisk helsearbeid 2011;3:206–16.
11. Orvik A. Organisatorisk kompetanse i sykepleie og helsefaglig samarbeid. Cappelen Akademisk Oslo. 2004.
12. Willumsen E (ed.). Tverrprofesjonelt samarbeid i praksis og utdanning. Universitetsforlaget, Oslo. 2009.
13. Hagen R, Johnsen E. Styring gjennom samhandling: Samhandlingsreformen som kasus. I A Tjora og L Melby (red.). Samhandling for helse. Kunnskap, kommunikasjon og teknologi i helsetjenesten. Gyldendal Akademisk, Oslo. 2013 (p. 32–53).
14. Jensen LH, Rekve KH (red.). PASSUS: Pasientorientert samhandling ved utskrivning til sykehjem. Skriftserie nr. 5 / Høgskolen i Buskerud og Vestfold. Drammen. 2014.
15. Kristoffersen K. Helsepersonells erfaringer fra samarbeid med pårørende til personer med demens i utskrivelsesprosessen fra alderspsykiatris avdeling til sykehjem: En kvalitativ studie. [Master's thesis]. Fakultet for helsevitenskap, Høgskolen i Buskerud, Drammen. 2013.
16. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today 2004;24:105–12.
17. Graneheim UH, Lundman B. Kvalitativ innhållsanalys. In: MG Granskär og B Höglund-Nielsen (eds.). Tillämpad kvalitativ forskning inom hälso- och sjukvård. Studentlitteratur, Lund. 2008 (p. 187–201).
18. Lovdata. Lov om behandling av personopplysninger. 14. april 2001; nr. 31 [personopplysningsloven]. Available at: https://lovdata.no/dokument/NL/lov/2000-04-14-31. (Downloaded 03.03.2017).
19. NEM, Den nasjonale forskningsetiske komité for medisin og helsefag. Veiledning for forskningsetisk og vitenskapelig vurdering av kvalitative forskningsprosjekt innen medisin og helsefag. Oslo. 2010.
20. Røkenes OH, Hanssen P-H. Bære eller briste. Kommunikasjon og relasjon i arbeid med mennesker. Fagbokforlaget, Oslo. 2002.
21. Goffman E. Interaction ritual: essays in face-to-face behavior. Aldine Transaction, New Brunswick. 1967/2005.
22. Schibbye, A-LL. Relasjoner: Et dialektisk perspektiv på eksistensiell og psykodynamisk psykoterapi. Universitetsforlaget, Oslo. 2009.
23. Repstad P. Sosiologiske perspektiver for helse- og sosialarbeidere. 3. ed. Universitetsforlaget, Oslo. 2014.
24. Gautun H, Bratt C. Bemanning og kompetanse i hjemmesykepleien og sykehjem. NOVA-rapport 14/14. Velferdsforskningsinstituttet NOVA, Oslo. 2014.
25. Danbolt LJ, Kjønsberg K, Lien L. Hjelp når du trenger det. En kvalitativ studie av samhandling og gjensidighetskunnskap i den psykiske helsetjenesten. Tidsskrift for psykisk helsearbeid 2010;3:238–45.
26. Molyneux J. Interprofessional teamworking: What makes teams work well? Journal of interprofessional care 2001;15:29–35.





Comments