Translation and psychometric testing of the Family Collaboration Scale
The instrument measures the collaboration between healthcare personnel and the relatives of frail elderly patients in acute hospital wards. Having a Norwegian version of the instrument will mean it can be used in our clinical practice and research.
Background: The Family Collaboration Scale (FCS) instrument has been developed to assess relatives’ experiences of the collaboration with healthcare personnel when a frail elderly person is admitted to an acute hospital ward.
Objective: The purpose of the study was to translate the FCS from Danish to Norwegian. We also wanted to test the psychometric properties of the translated version on a sample of the relatives of frail elderly patients who had been admitted to an acute hospital ward for medical treatment.
Method: The instrument was translated according to international criteria. The Norwegian version has been tested in a cross-sectional study with 147 relatives of patients over the age of 65. Reliability is tested through analyses of internal consistency and test-retest reliability. Validity is assessed through the evaluation of content and construct validity.
Results: Reliability analysed using Cronbach’s alpha and intraclass correlation coefficient (ICC) showed values above 0.7 for the five original dimensions. A panel of experts and relatives of patients rated the content validity as satisfactory. Evaluating construct validity using exploratory factor analysis showed that the original dimension structure was recreated to some extent, but three new factors emerged.
Conclusion: The Norwegian version of the FCS is essentially a reliable and valid instrument for measuring relatives’ experiences of the collaboration with healthcare personnel after a frail elderly person is admitted to an acute hospital ward. Before using the instrument in research and practice, we recommend further testing on a larger sample for further assessment of construct validity.
Most admissions of elderly patients in general hospitals are acute (1). Healthcare personnel have an obligation to involve the patient in their treatment and care, and the patient role entails statutory rights, such as the right to information and involvement (2). User involvement requires active and involved patients (3), but many older people are unprepared for taking part in such processes (4).
Research shows that some patients do not get involved in their treatment and care due to a lack of resources during their hospital stay (5). Among other things, illness and impairment can make it difficult to comprehend and process the content of the information provided (6). The results of a study on the discharge procedures for elderly patients show that patients wanted to participate, but this wish was largely ignored by the healthcare personnel. More than half of the participants had little or no opportunity to explain what they considered to be important for managing on their own after being discharged (5, 7). More than a third wanted to receive information together with their family, and almost half stated that they had not been offered such information (5).
Relatives as a resource or challenger
In the report to the Storting ‘Good quality – safe services – Quality and patient safety in the health and care services’ (3), patients’ relatives are characterised as an invaluable resource. They often have valuable knowledge about the patient’s background, medical history, resources and experiences from earlier treatment. They can take on the role of the patient’s spokesperson, contribute to the coordination between the various health services and help the patient to deal with information where the patient consents to this (3).
The relative’s role during hospitalisation is also the subject of research. The relatives consider themselves to be a support for the patient, and want to ensure that the patient’s interests and needs are safeguarded. If they have been involved in assisting and caring for the patient before admission to hospital, they can still feel responsible after this role is taken over by the healthcare personnel (8, 9).
Interacting and collaborating with relatives is regarded as good nursing practice (10-12), and can safeguard the patient’s right to user involvement (3). Despite the theoretical and political ideals, studies show that the collaboration between nurses and patients’ relatives is marked by challenges (12-14). Initially, nurses are positive to collaboration, but this can prove to be both challenging and time consuming (12, 13). Collaboration can be hampered by inadequate communication (13) or conflicts if relatives get involved in the patient’s care, thereby representing a challenge for the nurses (8, 12).
Charting the relatives’ perspective
Research shows significant correlations between relatives’ opportunities to participate in collaborative processes and their assessment of the quality of care in nursing homes (15). Correlations have also been found between the relatives’ degree of satisfaction with the hospital stay and the collaboration with nurses (16). It is therefore reasonable to assume that the relatives’ experiences with collaboration can be linked to their satisfaction and assessment of quality (17).
Based on a review of earlier research and contact with international research communities, Lindhardt et al. (17) found that there were no instruments available that charted the relatives’ perspective of the collaboration with healthcare personnel after frail elderly patients were admitted to general hospitals. They therefore developed the Family Collaboration Scale (FCS) instrument through a process of selecting relevant variables, developing questions and response options as well as designing a logical structure. This work is partly based on two qualitative studies where patients’ relatives and nurses were interviewed (11, 12). The FCS contains five dimensions, each of which measures different aspects of collaboration:
- Influence on decisions
- Quality of contact with healthcare personnel
- Trust and its prerequisites
- Achieved information level
- Influence on discharge
Lindhardt and her colleagues tested the instrument on a Danish sample and considered the psychometric properties to be satisfactory (17).
The purpose of translating the FCS to Norwegian is to make the instrument available in clinical practice and research. The instrument identifies barriers to collaboration and results of the collaboration in the form of relatives’ satisfaction, information level and quality of the hospital stay. It also identifies whether collaboration exists between patients’ relatives and healthcare personnel (16, 17).
Using the instrument can help to increase awareness of collaboration with relatives and their inclusion when desired by patients, which in turn can foster user involvement and improve the quality of care and treatment of elderly hospital patients.
Objective of the study
The objective of this study was to translate the FCS from Danish to Norwegian and to test the psychometric properties of the translated version in a sample of relatives of frail elderly patients following admission to an acute hospital ward for medical treatment.
Method
Translation and pre-testing of the FCS
We translated and adapted the Norwegian version of the FCS in accordance with a sequential translation procedure (18-20) (Figure 1). Two separate translators translated the instrument from Danish to Norwegian. The first translator was bilingual and a government-authorised translator, and the other translator was a nurse with extensive experience from clinical practice and a high level of proficiency in Danish. The differing backgrounds were in accordance with theoretical recommendations, which require one translator to be a linguistic expert and the other to have specialist competence in the subject to be studied (20-22).
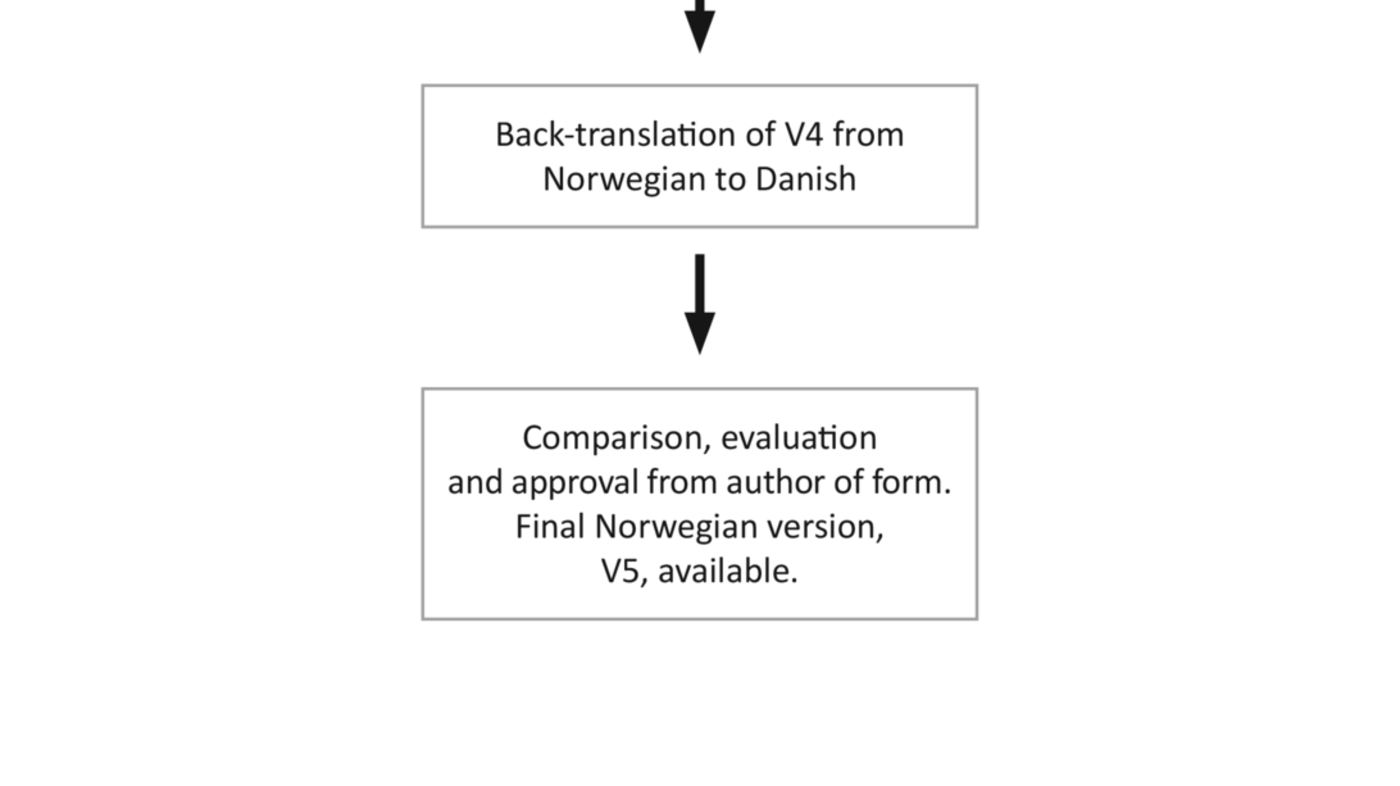
We performed a synthesis of the translated versions. This synthesis was reviewed by a consensus group consisting of a Danish senior consultant and two nurses with research expertise and clinical competence from the field of geriatrics. The group’s mandate was to discuss similarities and differences between the original and the translated version, as well as propose suggestions for adaptations.
Furthermore, we presented the Norwegian version to a panel of experts consisting of four nurses with extensive clinical experience from care of the elderly. They were asked to evaluate the wording, the relevance of the questions and the form as a whole. We then pre-tested the instrument on five relatives of sick, elderly patients who had recently been admitted to a general hospital with an acute illness. We conducted a personal interview after completion of the questionnaire, and asked the relatives whether they considered the questions to be comprehensible and meaningful. We also asked them to propose suggestions for changes.
In the original version, the Danish term ‘ sygeplejepersonale’ (nursing staff) was used in several of the questions. According to the Danish author, the term referred to all occupational groups that are involved in patient care in the hospital. We discussed the term with both the panel of experts and the patients’ relatives, and most related the term to staff who were qualified nurses. Several of the relatives thought it was difficult to distinguish between nurses and other nursing staff when reporting their experiences, and therefore preferred the term ‘ pleiepersonalet’ (healthcare personnel) in the Norwegian version of the instrument.
During the translation process, we made minor changes and adaptations to terms in order to make them more compatible with general Norwegian language usage. A different, independent, professional bilingual translator back-translated the edited version from Norwegian to Danish. We submitted the different versions as well as documentation from the translation procedure to the author of the questionnaire. The Danish author has worked in Norway for several years and has a good level of proficiency in Norwegian and terminology usage. She recommended only minor changes to individual words in order to ensure equivalence between the Norwegian and the original version.
Testing the FCS
The psychometric properties of an instrument refer to testing performed on a specific target group under given circumstances. It is therefore important to test psychometric properties when using the instrument in a different culture or in another target group (18, 20, 22). We tested the Norwegian version of the FCS using a cross-sectional survey.
Sample and data collection
We conducted the study at eight medical wards in a university hospital. A close collaboration was needed with healthcare personnel in order to recruit participants. Approved student assistants had responsibility for recruitment in three of the wards.
The inclusion criteria for the patients were that they were over the age of 65 and admitted with an acute illness or due to the worsening of a chronic illness. They had to have been staying at home before admission to hospital, have impaired health related to one or more conditions, and be in need of assistance and support in everyday life. They had to be competent to give consent, i.e. speak Norwegian sufficiently and not have a conjunctive impairment. The patients received written and oral information. Those who wanted to participate gave written informed consent so that we could contact the relative who, according to the patient, were most involved in providing assistance and support and who had been present during their hospital stay.
Fourteen days after the patient was discharged from hospital, the relative was sent an information letter with a request to participate, along with a questionnaire ( Appendix 1) and a stamped addressed envelope for returning the questionnaire. We conducted a selective reminder procedure by telephone three weeks after the first communication. Returning the questionnaire was regarded as consent to participate.
The FCS questionnaire
The FCS is composed of 27 questions, which contain a total of 45 Likert scales and make up the various dimensions of the instrument. In addition, nine categorical variables are included in the instrument ( Appendix 1, questions 20-56). The response options on the Likert scales are rated from 1-4 or from 1-6, where a low score indicates a high degree of collaboration.
The questionnaire also contains nine socio-demographic questions about patients’ relative (questions 1-9) and five categorical variables that chart the scope of help that the relative provided (questions 10-14). Five questions about relatives’ experiences (questions 15-19) and the open-ended question at the end of the form were not part of the FCS instrument, and were not therefore analysed in this study.
We added three questions for this study, which can be found in the questionnaire ( Appendix 1). These questions identify which department the elderly patient was admitted to as well as the reason for the admission. In addition, one question asks whether the relative of the patient wanted to fill out the questionnaire again after two to three weeks in order to test the instrument’s stability by repeat monitoring.
Analyses
We scanned data from completed questionnaires into a database. We then encoded, scored and summarised the data in dimensions based on the score description devised by the author of the questionnaire (17). We summarised and transformed questions in each dimension to values from 0-100, where higher scores indicated that relatives were less satisfied or experienced less collaboration with healthcare personnel. In questions with more than one possible answer, the number of answers was summarised.
We performed the analyses using the statistics program SPSS version 21.0. Descriptive statistics were used to analyse socio-demographic variables and the type of assistance that relatives provided, and to obtain an overview of the dimensions of the form. We assessed reliability through internal consistency analyses (Cronbach’s alpha and the correlation of individual questions with each sub-scale) and stability (test-retest reliability).
Stability was analysed using the intraclass correlation coefficient (ICC) through the variance measurement of average scores and repeated average scores from the participants who responded to the FCS twice. The panel of experts and pre-test participants evaluated the content validity of the instrument in the translation process and assessed the form as a whole, the suitability of the individual questions, and whether they were adequate to measure the collaboration with the healthcare personnel. We analysed construct validity using exploratory factor analysis (EFA), with Principal Component Analyses (PCA) as an extraction method and Varimax rotation.
We focused on performing the analyses in the same way as the author of the questionnaire described in the test of the Danish version (17) in order to compare the results. A total of 44 questions were included in the EFA. The Kaiser-Meyer-Olkin (KMO) test of 0.81 indicated that the sample size was sufficient (23). Bartlett’s test for all correlations was significant (p <0.001), and the analysis was therefore justified (23).
Spearman’s rank order correlation (Spearman’s rho) was used to analyse the correlation between the questions in each dimension and between the different dimensions. Significance level was set to p ≤0.05.
Ethical aspects
The study was approved by clinic managers, and in addition we informed ward administrators, charge nurses and healthcare personnel in writing and orally before recruitment started. According to the Regional Committees for Medical and Health Research Ethics (REC), the study did not require approval. The university hospital’s own Data Protection Official (DPO) approved the study and provided directives for anonymising and storing the data. A list of names and corresponding ID numbers were kept locked away and unavailable to unauthorised parties during the recruitment period, and we deleted the list at the end of the study.
Results
We contacted a total of 243 patients, and of these, 230 consented to us contacting their relative. A total of seven participants were excluded owing to death of the patient after consent was given (n = 3), a lack of contact details for the relative (n = 2), age (n = 1) or exercising of the patient’s right to withdraw consent (n = 1). We sent out 223 questionnaires, and a total of 147 relatives returned a completed form (66 per cent). All relatives were asked if they were willing to fill out the questionnaire again after three weeks in order to perform a stability analysis, and 22 relatives did this.
We present an overview of the socio-demographic variables in Table 1. The typical participant was a married or cohabiting woman aged 58.5 with a higher education and in employment. She was the daughter of the elderly patient, and they did not live together.
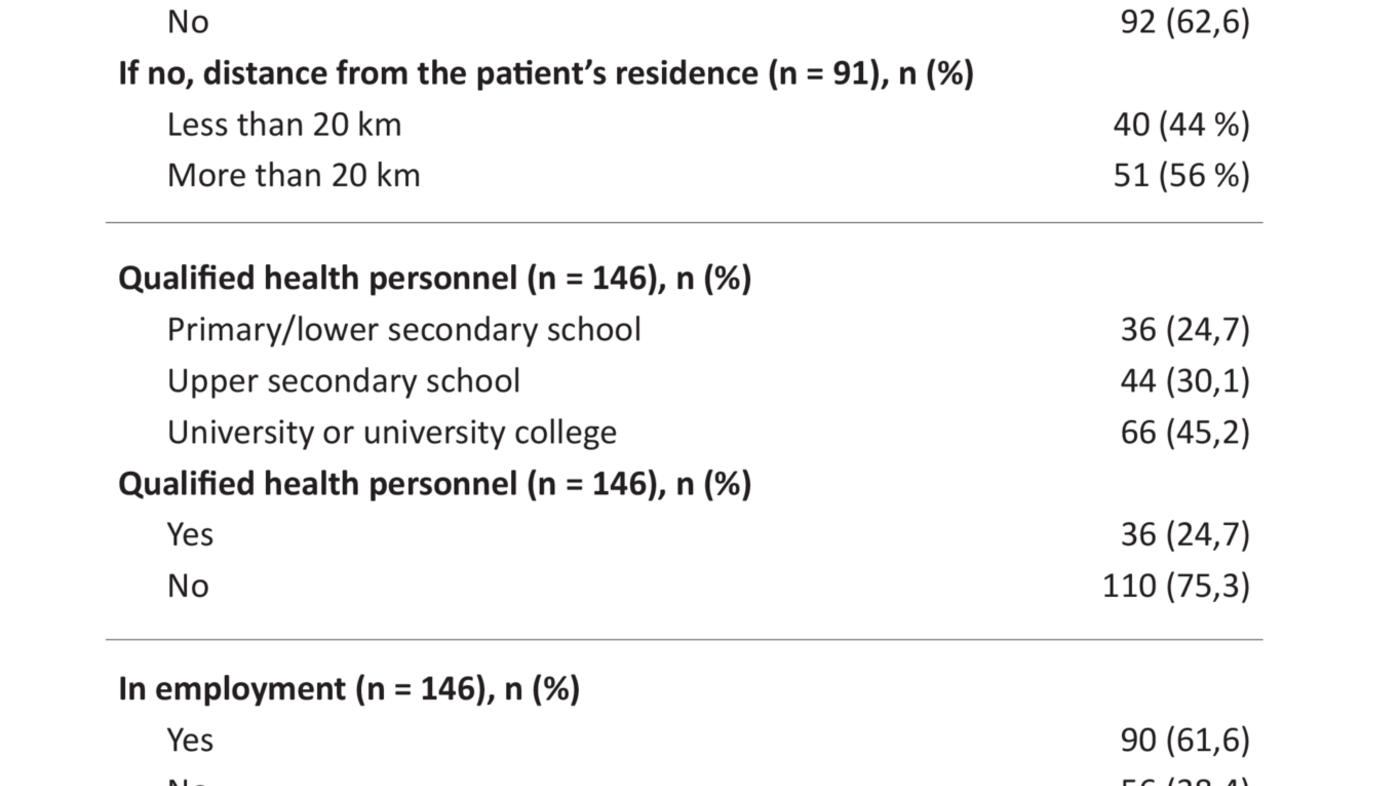
Table 2 presents a frequency overview of the variables that characterise the assistance provided by the relative to the elderly in need for support. In addition, analyses showed that relatives were mainly involved in assistance such as psychological support and encouragement (58 per cent), practical help in the home (57 per cent), accompanying the patient on outings (57 per cent) and shopping (57 per cent). Fewer provided personal assistance such as help with personal hygiene, toilet visits, washing hair and help to eat (22 per cent) or physical training (3 per cent).
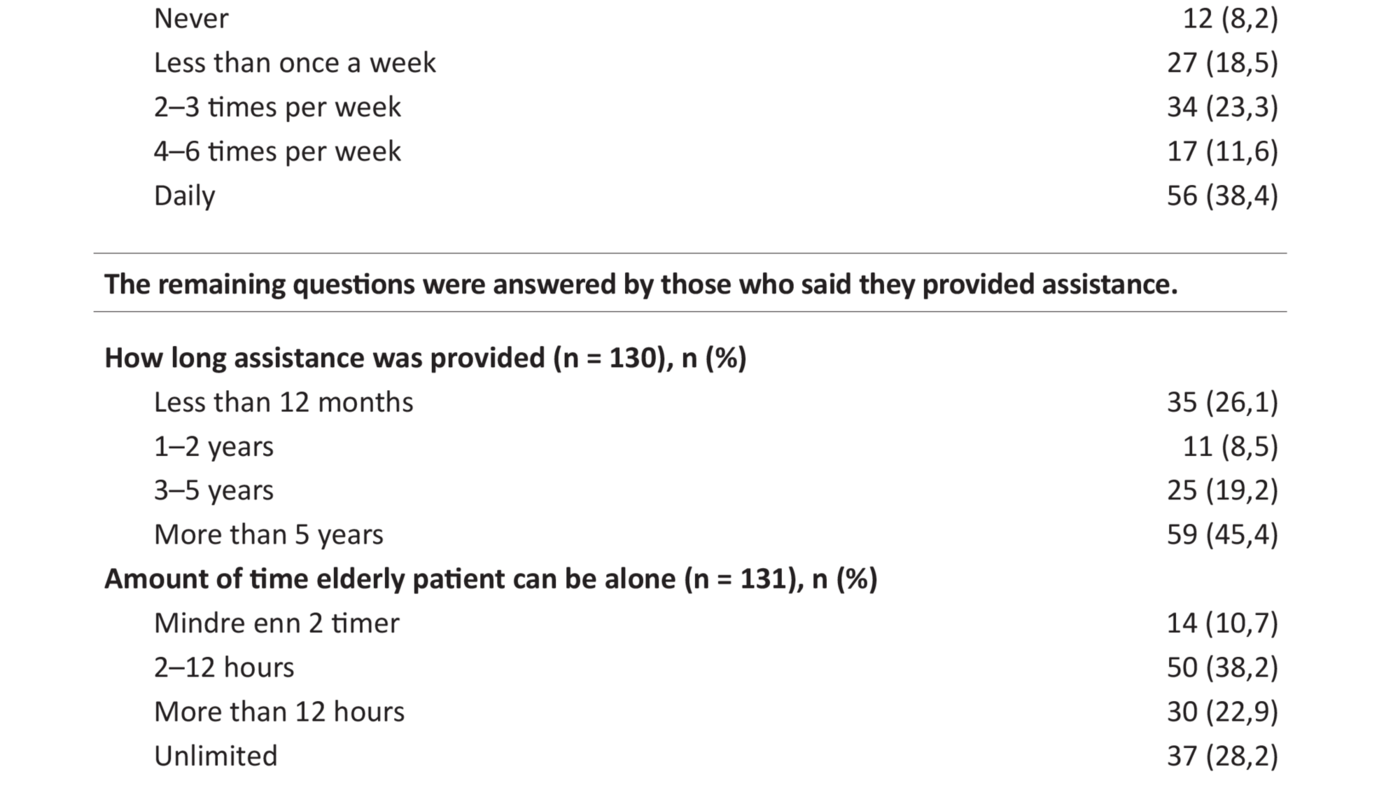
In Table 3 we present the results for the summary measurements for the five original dimensions of the FCS. The dimension ‘influence on decisions’ had the highest average score of 62.6. The dimension ‘trust and its prerequisites’ had the lowest average score. The significant left-skewed distribution of the results, i.e. a prominence of low scores, indicates that relatives experienced a high level of trust. ‘Influence on discharge’ had the highest non-response rate. This may be due to the fact that one question should have been answered by respondents who had answered ‘no’ to a preceding question, which resulted in a 29 per cent non-response rate for the follow-up question.
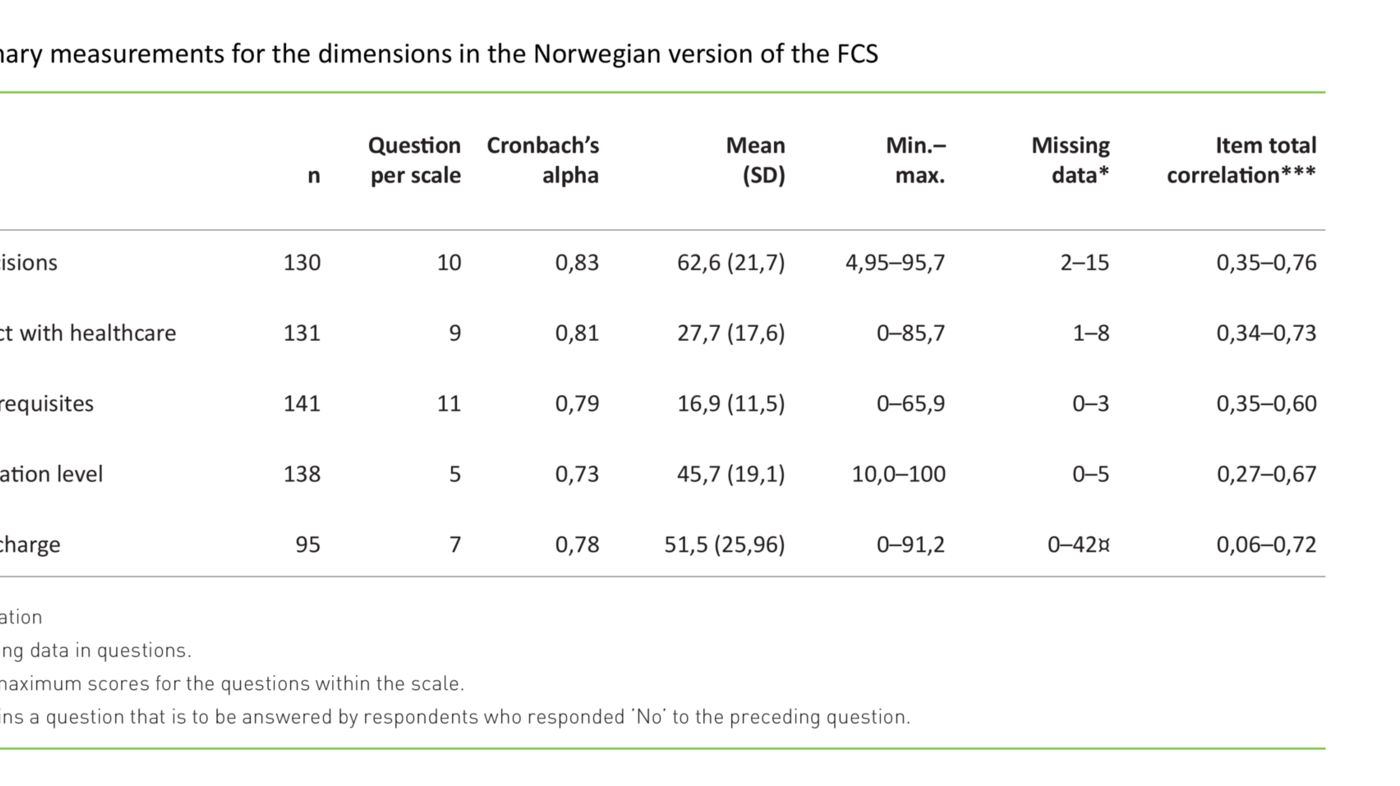
Reliability analyses
Internal consistency, analysed by Cronbach’s alpha, showed a score in excess of 0.7 for all five original dimensions. The correlations between individual questions and each scale showed varying correlations as an expression of varying overlap between individual questions and the corresponding scale (Table 3). Test-retest reliability was analysed using the intraclass correlation coefficient (ICC), and all five dimensions held values in excess of 0.7.
Validity
Experts and the patients’ relatives assessed content validity in the pre-test of the questionnaire. Both groups considered the form to have good direct validity, and the first impression was that the content referred to various aspects of the collaboration between families and health personnel. All relatives pointed out that the content was easy to understand, relevant and recognisable. Several relatives thought that the questionnaire was useful as they had had varying experiences in the collaboration with healthcare personnel.
Question 32 (Appendix 1) referred to whether the problem that led to the hospital admission had been resolved. This question was the only one that was removed from the factor analysis due to the low correlation with the other questions.
A total of 44 questions were included in the factor analysis. According to Kaiser’s criterion (eigenvalue > 1) and interpretation of the scree plot, eight factors could be included, and these accounted for 61.5 per cent of the total variance. Two of the five original dimensions were split, and three new factors emerged. Table 4 presents an overview of factors and includes the questions’ factor loading (≥ 0.3).
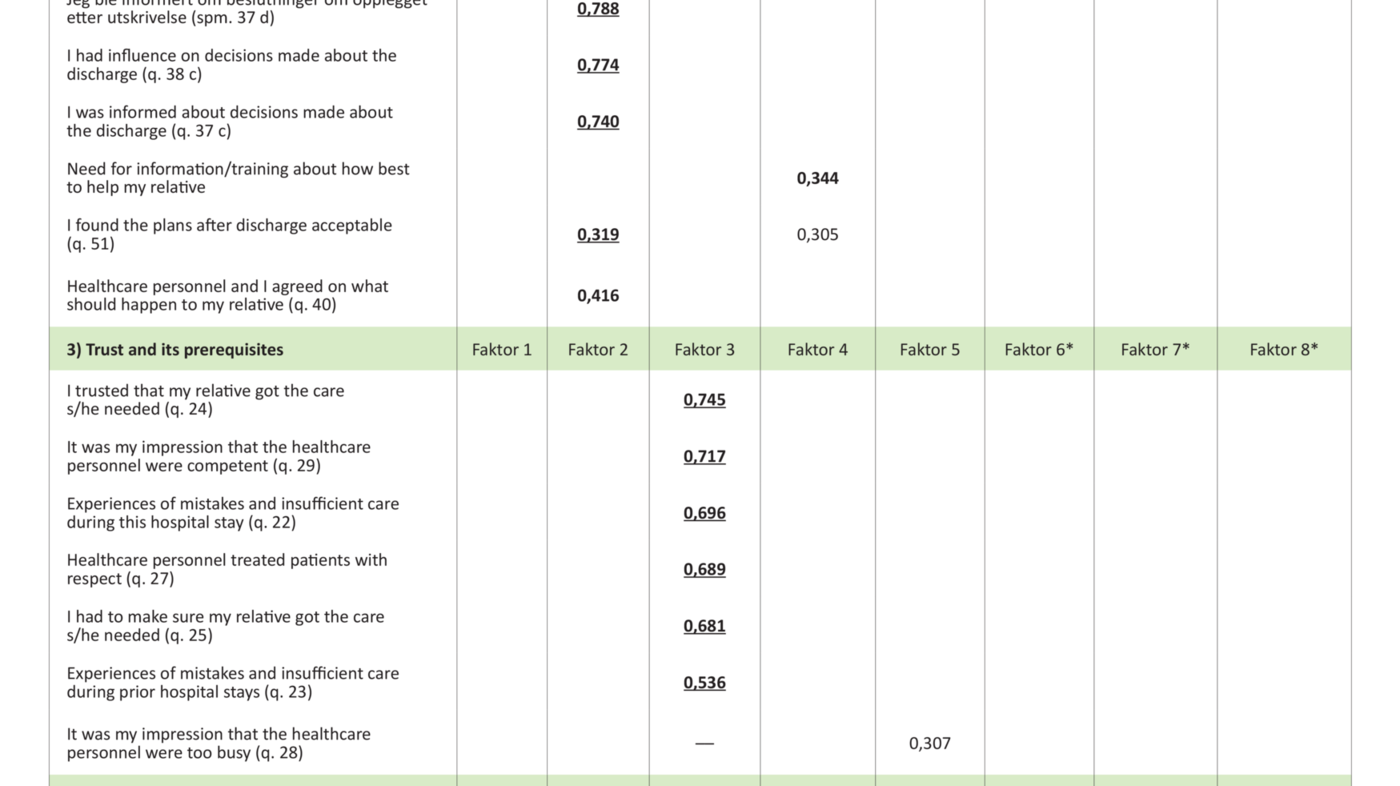
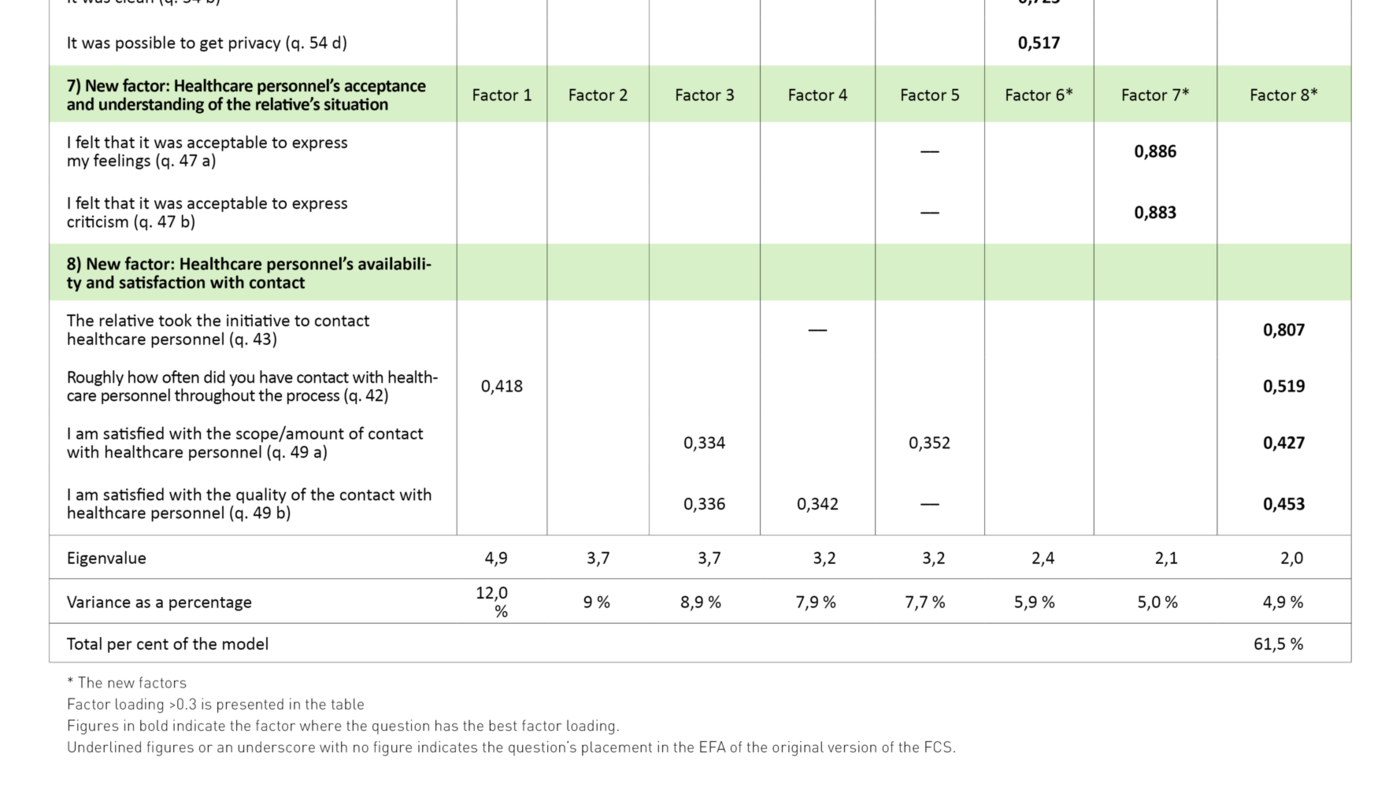
The first factor reflected the dimension ‘influence on decisions’, and a total of eight out of ten questions had the strongest loading here. The second factor in the analysis was in accordance with the ‘influence on discharge’ dimension. The factor contained five of the original seven questions, but one question (question 51) had a low loading. Factor three formed part of the dimension ‘trust and its prerequisites’, but four of the original questions formed a new factor (factor six). Factor four is compatible with the dimension ‘achieved information level’, but question 43 fell under factor eight. Factor five to some extent corresponds to the dimension ‘quality of contact with healthcare personnel’ and contains five of the original nine questions. Two of the questions fell under factor seven (questions 47 a and b), and two had the highest loading in factor eight (questions 49 a and b).
The values for correlation between the five original dimensions of the FCS ranged from 0.18 to 0.61. Correlation between the questions in each dimension confirmed that the questions with a low loading in the factor analysis or that had fallen outside the original dimensions had a low correlation with the other questions in the respective dimensions.
Discussion
The response rate after the reminder procedure (66 per cent) is considered to be acceptable for a questionnaire survey (18). We did not carry out a non-response analysis, but frequency analyses indicated that some groups were underrepresented. Only 17 per cent of the participants were over the age of 70, and just under 25 per cent reported primary/lower secondary school as the highest completed level of education. These are groups that historically have high non-response rates in questionnaire surveys (24, 25).
Descriptions and testing of the original Danish version of the FCS showed a good correlation between theory and practice, and the instrument was considered to be reliable and valid within the test population (17). The Norwegian version of the FCS is considered to have satisfactory internal consistency (18, 21) for the five original dimensions. High scores for ICC indicate that the Norwegian version of the FCS has stable properties, which is important for overall reliability (26).
Different cultures can come into play
The hypothetical correlations of a construct should be tested using a confirmatory factor analysis (CFA) (18). In our study, this method was not justified since the sample size did not meet the criteria for the analysis (27). We therefore assessed the construct validity of the instrument by analysing its structure using EFA, which is suited to assessing differences between the original and translated instrument (21).
Where questions did not load into their original factors after translation, this may be an indication that they are not perceived in the same way in the different cultures (21). Although it is assumed that there are few cultural differences between Denmark and Norway, disparities may be attributed to the organisation of nursing and care. It may also be that relatives have different expectations of collaboration and user involvement, but this is not certain.
Questions should have factor loading ≥0.4 within the corresponding dimension (23, 25). A total of 13 of the questions have a low loading and cannot therefore be related to the original dimensions (Table 4). In this study, this means that they cannot be linked to the properties they were originally set to measure. In addition, the analysis shows that four individual questions have a high factor load of >0.4 in several dimensions, which complicates the interpretation of which factor they belong to (21).
Different result when using other populations
The first of the new factors (factor six) consists of four questions that relate to the physical conditions of the ward (Table 4, questions 54a-d), and originally belonged to the dimension ‘trust and its prerequisites’. Theoretically, the questions are related to the fact that contextual relationships in a hospital environment can be barriers to collaboration, which in turn may affect the relatives’ experience of trust (16, 17). In this study, the analyses showed that the questions had a low correlation to other questions about trust, and thus they do not reflect the same property (21). Differences in the results can be attributed to the composition of the samples, but it cannot be ruled out that Danish and Norwegian relatives had different perceptions of the impact of the physical environment in relation to the experience of trust and collaboration.
Factors seven and eight emanate from the dimension ‘quality of contact with healthcare personnel’, and interpretation suggests that the new factors measure ‘healthcare personnel’s acceptance and understanding of the relatives’ situation’ and ‘healthcare personnel’s availability and satisfaction with contact’. Theoretically, they are linked to collaboration, since being available and accommodating are prerequisites for contact and communication (17). The analyses showed that several of the questions in these dimensions had low average scores. Such a floor effect arises when the response options are not adequate for what is being measured or when the instrument is used in a population that is different to the one for which it was developed (21).
In structural analyses, such skewed distributions tend to have a lower correlation with other questions and to stand out (28). These factors must therefore be interpreted with caution, and this analysis cannot confirm whether they reflect separate dimensions of the concept of collaboration, or whether the dimensions are the result of highly correlated questions that measure other properties. A factor should also consist of at least three questions (21), and factor seven does not meet this criterion.
Norwegian relatives had lower scores
On average, Norwegian relatives scored lower than the Danish relatives in all dimensions (17), indicating that they collaborated more with the healthcare personnel. The disparities can also be attributed to differences in the way interaction and collaboration with relatives is organised, but we do not know this for certain.
Disparities in results between an original and a translated instrument can be attributed to the translation procedure, where terms and definitions used can change the meaning of the questions. Disparities can also emerge due to cultural differences (21). We took these factors into account in the translation process, and the objective was that the instrument should be equivalent to the original version. Similarity in expression and meaning means semantic equivalence (18, 20), and comparison of the original and the back-translated version of the form showed a satisfactory degree of such equivalence. The original factor solution that constitutes the five dimensions of the instrument was partly reflected in the subsequent results.
The sample size of 147 participants may affect the results of the instrument’s construct validity. According to Field (23), a stable factor solution is found in samples with more than 300 participants, and factors with a low factor loading should be interpreted with caution in small samples (23). Other recommendations indicate that there should be at least three participants per variable, where ten respondents per variable is considered to be a good basis for analysis (18).
In our study, the ratio was 3.3 participants per variable, which is within the lowest recommended limit. In addition, the KMO test showed that the sample had an above average degree of sufficiency, and the analysis was therefore justified (23). The size of the sample should nevertheless be taken into consideration when assessing the factor structure and stability thereof. Lindhardt et al. conducted the factor analysis of the original version in a sample of 158 participants (17), and we cannot therefore rule out that the disparities in the factor solutions may be attributed to the sample size in both studies.
Conclusion
We translated the Family Collaboration Scale (FCS) instrument from Danish to Norwegian according to international criteria. The Norwegian version is considered to have satisfactory reliability, and experts and pre-test participants judged its content validity to be good. Our analyses of construct validity showed that the factor structure partly corresponds to the five original dimensions.
Certain questions differed by not being included in their original dimension, by creating new factors or by emanating from the analysis. The instrument should therefore be tested in a larger heterogeneous sample, and a confirmatory factor analysis should be performed in order to test the hypothetical relationships between the questionnaire’s original dimensions before further use.
According to the recommendation from the author of the questionnaire, a short version should be devised for the oldest family members (17). In order to expand the area of application of the instrument, consideration should be given to adapting and testing the FCS on different relative groups to those included in this study, such as relatives of patients who have been admitted to hospital for surgical treatment or intensive treatment.
References
1. Meld. St. 47 (2008–2009). Samhandlingsreformen: Rett behandling – på rett sted – til rett tid. Oslo: Helse- og omsorgsdepartementet; 2009.
2. Lov 2. juli 1999 nr. 63 om pasient- og brukerrettigheter (pasient og brukerrettighetsloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-63(downloaded 25.08.2017).
3. Meld. St. 10 (2012–2013). God kvalitet – trygge tjenester: Kvalitet og pasientsikkerhet i helse- og omsorgstjenesten. Oslo: Helse- og omsorgsdepartementet; 2012.
4. Bentley J. Older people as health service consumers 4: disempowered or disinterested? British Journal of Community Nursing. 2003;8(4):181–7.
5. Foss C, Hofoss D, Romøren TI, Bragstad LK, Kirkevold M. Eldres erfaringer med utskrivning fra sykehus. Sykepleien Forskning. 2012(4):324–33. Available at: https://sykepleien.no/forskning/2012/11/eldres-erfaringer-med-utskrivning-fra-sykehus(downloaded 25.08.2017).
6. Hellesø R, Eines J, Fagermoen MS. The significance of informal caregivers in information management from the perspective of heart failure patients. Journal of clinical nursing. 2012;21(3–4):495–503.
7. Foss C, Hofoss D. Elderly persons’ experiences of participation in hospital discharge process. Patient Education and Counseling. 2011;85(1):68–73.
8. Allen D. Negotiating the role of expert carers on an adult hospital ward. Sociology of Health & Illness. 2000;22(2):149–71.
9. Li H, Stewart BJ, Imle MA, Archbold PG, Felver L. Families and hospitalized elders: A typology of family care actions. Research in Nursing & Health. 2000;23(1):3–16.
10. Norsk Sykepleierforbund. Yrkesetiske retningslinjer for sykepleiere. Available at: https://www.nsf.no/vis-artikkel/2193841/17102/Yrkesetiske-retningslinjer(downloaded 04.11.2016).
11. Lindhardt T, Bolmsjö IA, Hallberg IR. Standing guard – being a relative to a hospitalised, elderly person. Journal of Aging Studies. 2006;20(2):133–49.
12. Lindhardt T, Hallberg IR, Poulsen I. Nurses’ experience of collaboration with relatives of frail elderly patients in acute hospital wards: A qualitative study. International Journal of Nursing Studies. 2008;45(5):668–81.
13. Hertzberg A, Ekman SL, Axelsson K. ʻRelatives are a resource, but…ʼ: Registered Nurses' views and experiences of relatives of residents in nursing homes. Journal of Clinical Nursing. 2003;12(3):431–41.
14. Ward-Griffin C, McKeever P. Relationships between nurses and family caregivers: Partners in care? Advances in Nursing Science. 2000;22(3):89–103.
15. Voutilainen P, Backman K, Isola A, Laukkala H. Family members' perceptions of the quality of long-term care. Clinical Nursing Research. 2006;15(2):135–49.
16. Lindhardt T, Nyberg P, Hallberg IR. Collaboration between relatives of elderly patients and nurses and its relation to satisfaction with the hospital care trajectory. Scandinavian Journal of Caring Sciences. 2008;22(4):507–19.
17. Lindhardt T, Nyberg P, Hallberg IR. Relatives’ view on collaboration with nurses in acute wards: Development and testing of a new measure. International Journal of Nursing Studies. 2008;45(9):1329–43.
18. Polit DF, Beck CT. Nursing research: Generating and assessing evidence for nursing practice (9th edition). Philadelphia: Wolters Kluwer Health; 2012.
19. Beyer N, Magnusson P, Thorborg K. Målemetoder i forebyggelse, behandling og rehabilitering: Teori og anvendelse. (2nd edition). København: Munksgaard; 2012.
20. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–91.
21. de Vet HCW, Terwee CB, Mokkink LB, Knol DL. Measurement in medicine : A practical guide. Cambridge: Cambridge University Press; 2011.
22. Wahl AK, Hanestad BR. Måling av livskvalitet i klinisk praksis: En innføring. Bergen: Fagbokforlaget; 2004.
23. Field A. Discovering statistics using IBM SPSS statistics (4th edition). Los Angeles: SAGE; 2013.
24. Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L et al. The measurement of satisfaction with healthcare: Implications for practice from a systematic review of the literature. Health Technology Assessment. 2002;6(32):1–244.
25. Eikemo TA, Clausen TH. Kvantitativ analyse med SPSS : En praktisk innføring i kvantitative analyseteknikker (2nd edition). Trondheim: Tapir akademisk forlag; 2012.
26. Walters SJ. Quality of life outcomes in clinical trials and health-care evaluation: A practical guide to analysis and interpretation. Hoboken: Wiley; 2009.
27. Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research. 2006;99(6):323–38.
28. Clark LA, Watson D, Butcher JN. Constructing validity: Basic issues in objective scale development. Psychological Assessment. 1995;7(3):309–19.










Comments