Master’s degree in anaesthesia and intensive care nursing: a survey of attitudes and expectations in academia and in the field
Sykepleiere med master i anestesi- og intensivsykepleie vil styrke helseteamets samlede kompetanse og bidra til økt pasientsikkerhet.
Background: The Ministry of Education and Research has implemented a new framework, which is based on a degree structure. Credits have not previously been awarded for specialist nursing courses within the degree system, and these courses are now being converted into master’s degree programmes. In parallel with this development, new requirements are being introduced for specialist nurses due to the rapidly changing health service.
Objective: The purpose of the study was to survey attitudes and expectations in relation to a master’s degree programme in anaesthesia and intensive care nursing.
Method: The study was a cross-sectional study in which we invited anaesthesia and intensive care nurses and their first-line managers, clinical nurse educators and teaching staff associated with education in anaesthesia and intensive care nationally to answer an online questionnaire. The questionnaire was based on statements from a qualitative study exploring attitudes and expectations in relation to master’s degrees. We divided the statements into the following areas: ‘Knowledge-based practice’, ‘Critical thinking and interaction competence’, ‘Skill level and theoretical competence’, ‘Recruit and retain’ and ‘The need for a master’s degree’.
Results: A total of 1661 people were asked to participate, and 475 responded to the questionnaire. This corresponds to a response rate of 29 per cent. The participants were most positive about the possibility of a master’s degree impacting on the areas of ‘Knowledge-based practice’ and ‘Critical thinking and interaction competence’. There was somewhat more scepticism as to whether it would contribute to ‘Skill level and theoretical competence’ and ‘The need for a master’s degree’. Within the area ‘Recruit and retain’, the participants expressed some concern about problems related to recruitment. Men were somewhat more critical of a master’s education than women. The respondents from local hospitals were significantly more concerned than the respondents from university hospitals about being able to recruit and retain specialist nurses with a master’s degree. The respondents from the Northern Norway Regional Health Authority were also significantly more concerned about recruiting and retaining specialist nurses with a master’s degree than the respondents from the South-Eastern Norway Regional Health Authority.
Conclusion: Attitudes and expectations in relation to a potential master’s degree in anaesthesia and intensive care nursing were generally positive. The majority agreed that converting the existing specialist nursing courses into master’s degree programmes is a natural development. Few expressed concern that a master’s degree would reduce practical skills. Some expressed potential problems with recruiting and retaining nurses with a master’s degree in clinical practice.
The specialist health service is characterised by complexity, time pressure, organisational changes, new technology, new treatment options and a requirement for knowledge-based practice. Knowledge-based practice entails treatment and care that is informed by research, practitioners’ experience and the service user’s wishes (1). One of the major challenges is planning for sufficient and appropriate competence (2).
In 2005, the EU developed the overarching European Qualifications Framework (EQF) (3, 4). The requirements for the degree structure were laid down in the Norwegian Act relating to Universities and University Colleges from 2011 (5).
The framework covers education at bachelor, master and doctorate levels and describes the qualifications at the different levels (5). At present, specialist nurses are increasingly having to relate to new knowledge, and they must be able to drive change processes and participate in and lead the development of the clinical field.
In Report no. 44 to the Storting (2008–2009) (6), the Ministry of Education and Research pointed out the following: ‘There will be a growing demand in the labour market for people who understand and can take a critical approach to applying research results, and not least who are able to conduct research or use the research methods themselves’ (6).
Report no. 4 to the Storting (2018–2019) emphasises the educational institutions’ responsibility for the quality of education (7), which includes offering attractive, good-quality study programmes that provide competence for a long working life.
It is not sufficient to prepare students for a profession. Higher education must prepare students for tasks that do not yet exist, technologies that have not yet been invented, and problems we do not yet know will arise.
This means that students must understand complex contexts, have the skills needed to acquire new knowledge, and develop creativity and problem-solving skills. They must also be able to exercise professional judgement and work across disciplines (8–10).
Research in professional studies has traditionally had two main aims: to strengthen education and to strengthen the field of practice. These are still important objectives. Research shows that attaining a master’s degree provides a basis for changing the professional dialogue in relation to patients, patients’ families, colleagues and other healthcare personnel (11–13).
The Stjernø Commission, which was appointed by the Minister of Education, Øystein Djupedal, and whose mandate was to recommend new structures in higher education and research, welcomed the master’s degree in clinical nursing. The Commission was of the opinion that the study programme, which grew from a robust professional education, provided a good basis for developing knowledge related to the profession and the field of practice (14).
Students need both academic and specialist clinical competence to be able to fulfil their role of specialist nurse. Study programmes must help ensure that the students can integrate knowledge, handle complex events and situations and develop an ability to participate in clinical research and development (15–18).
Most educational institutions currently offer a master’s degree in specialist nursing. Some institutions only offer studies at the master level, while others offer both specialist nursing courses and master’s degrees. The requirement for a universal knowledge-based approach brings with it a need for better understanding of methodology than has previously been taught in specialisation courses.
A Swedish study showed that the methodology must be adapted to the relevant discipline in order for students to recognise the value of specialising in the subject and the need for a more academic approach to the complexities of their profession (15).
The process of converting specialist nursing courses to master’s degrees programmes has led both to concerns about the consequences and enthusiasm among academics and professionals. They have used terms such as ‘master’s disease’, ‘overqualification’, ‘a way through a dead-end street’ and ‘function-oriented masters’ (19, 20).
A recent Norwegian qualitative study (21) explored 25 anaesthesia and intensive care nurses’ perceptions and expectations in relation to a master’s degree programme. The respondents believed that the value of a master’s degree will be reflected in the nurse’s language and increased ability to think critically. This in turn will be reflected in their behaviour and how they interact.
The respondents also reported an expectation of competence enhancement and the capability to exercise knowledge-based practice. Furthermore, they expressed concern about whether students could learn the same skill level and theoretical competence in a master’s degree in specialist nursing as in specialisation courses (21).
When changing the content and level of the education, it is important to understand how it could impact on patients, colleagues and society as a whole. Educating anaesthesia and intensive care nurses is especially important in this regard because they work in a high-tech environment where the requirement to stay abreast of developments in their field is vital to good and safe patient care.
Those who are best placed to describe the consequences of such changes are the future practitioners, managers, professional development personnel in health trusts and teaching staff.
Objective of the study
- To collect data on attitudes and expectations in relation to a master’s degree in anaesthesia and intensive care nursing.
- To investigate whether individual and work-related characteristics (gender, age, years of experience as a specialist nurse, job category, type of hospital and health region) have a bearing on attitudes and expectations in relation to a master’s degree.
Method
We conducted this cross-sectional study in the autumn of 2017. We sent information about the study and a link to the questionnaire to first-line managers of anaesthesia and intensive care nurses at 78 hospitals, both public and private. Responses were received from 34 hospitals.
The email addresses of the managers at the various hospitals were obtained from the nursing union’s moderated forum for anaesthesia and intensive care nurses. The managers forwarded the request to their staff by email. We collected data via the University of Oslo’s digital platform Nettskjema, where the responses were anonymised in order to obscure email and IP addresses.
Teaching staff in the anaesthesia and intensive care nursing programmes were directly invited to participate through email lists that were collected in the respective lecturer networks. We sent a reminder via the first-line managers who forwarded the requests. Approval of the study was ensured since the managers passed on the invitation to their employees.
Submission of the online questionnaire was considered to represent informed consent from the respondents. The study was approved by the Norwegian Centre for Research Data, ref. no. 54679, and the management at Oslo Metropolitan University.
Instrument
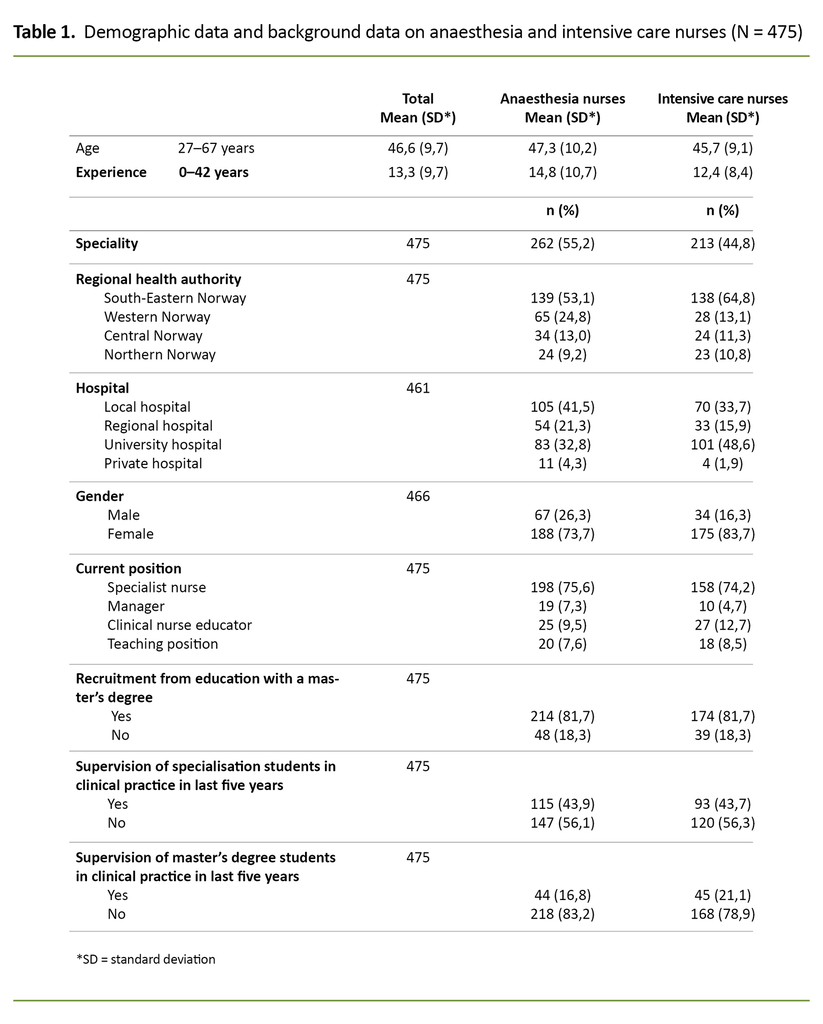
The questionnaire consists of 36 questions in total. The background information we collected was specialty (anaesthesia or intensive care nursing), age, gender and years of experience as a specialist nurse.
We also obtained data on the respondents’ current position, type of hospital, health region and whether relevant colleges and universities offer a master’s degree in anaesthesia and intensive care nursing.
We based questions about attitudes and expectations on results from an earlier qualitative study (21), which explored expectations of how master’s degree competence can contribute to clinical practice. When preparing the questionnaire, we used statements from the focus group interviews, both positive and negative.
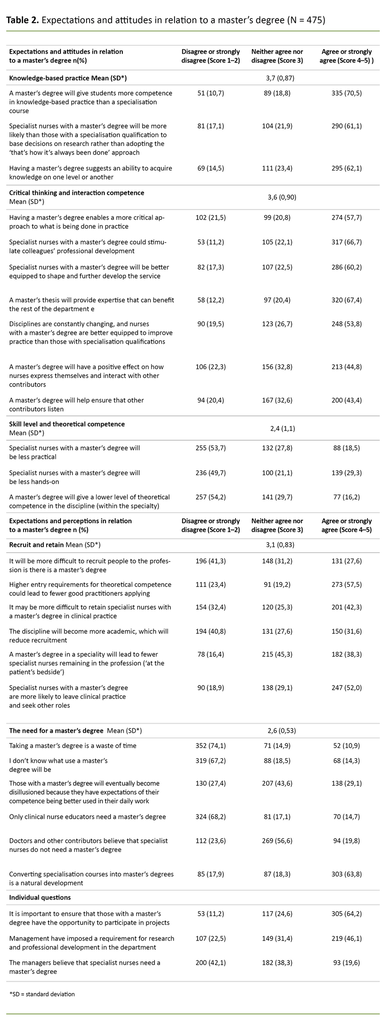
We divided the individual statements (28) into the following areas: ‘Knowledge-based practice’ (3 statements), ‘Critical thinking and interaction competence’ (7 statements), ‘Skill level and theoretical competence’ (3 statements), ‘Recruit and retain’ (6 statements), ‘The need for a master’s degree’ (6 statements) and 3 other individual statements.
We asked participants to score the statements on a Likert scale from 1–5 (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree and 5 = strongly agree). In some analyses, the response alternatives ‘strongly disagree’ and ‘disagree’ were merged, as were ‘agree’ and ‘strongly agree’.
Because the various statements were both positively and negatively charged, a high value will not necessarily be an indication that the answers are veering towards a positive direction or vice versa.
To test the reliability of the questionnaire, we calculated Cronbach’s alpha for the different areas: ‘Knowledge-based practice’ (α = 0.71), ‘Critical thinking and interaction competence’ (α = 0.92), ‘Skill level and theoretical competence’ (α = 0.92), ‘Recruit and retain’ (α = 0.83) and ‘The need for a master’s degree’ (α = 0.78). Cronbach’s alpha above 0.70 is considered acceptable (22).
Two researchers quality-assured the language and content of the questionnaire. One of them has a background as an anaesthesia nurse, and the other has extensive experience in preparing questionnaires.
Statistical analyses
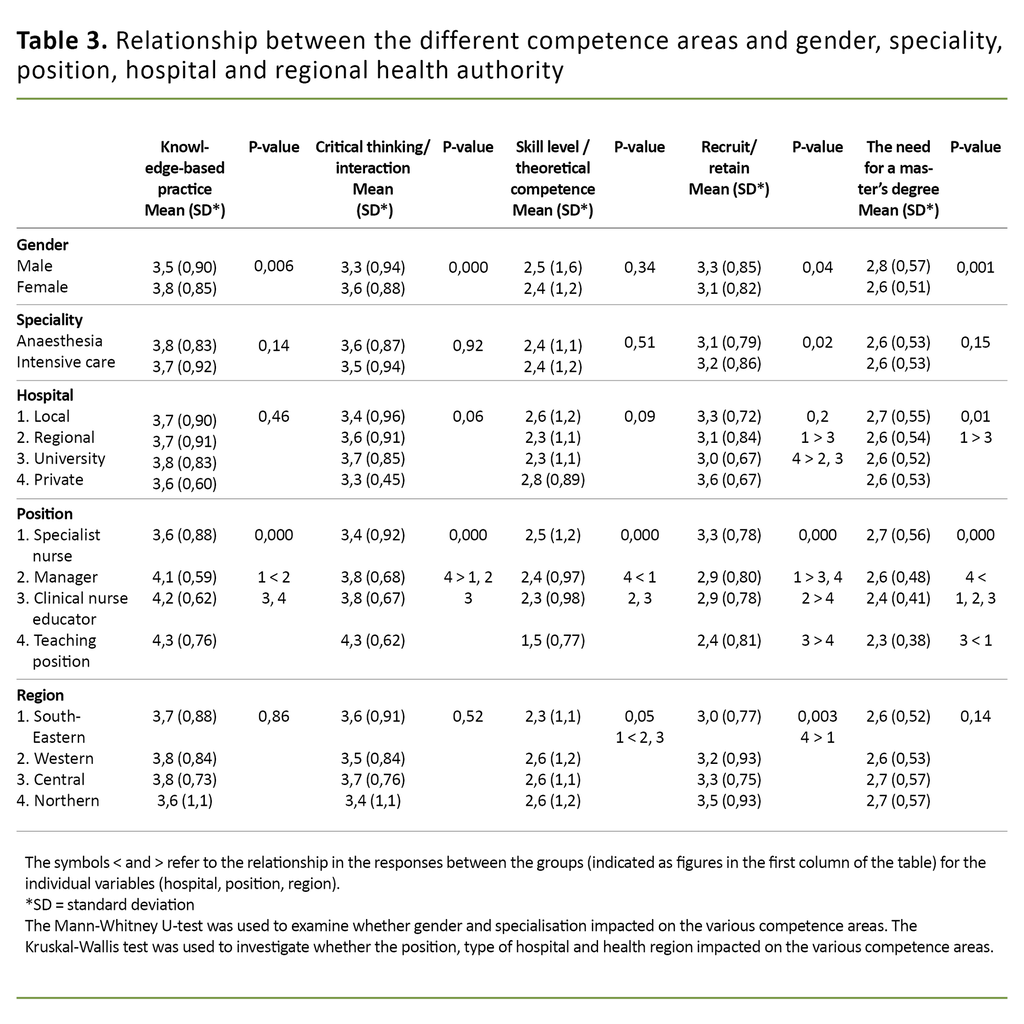
We used the Mann-Whitney U-test to investigate whether gender and specialisation impacted on the different areas. We used the Kruskal-Wallis test to investigate whether position, type of hospital and health region impacted on the different areas (Table 3). We used Pearson’s correlation test to investigate the relationship between the competence areas, age and experience.
Results
A total of 1661 people were asked to participate; 824 anaesthesia nurses and 837 intensive care nurses. Of these, 475 responded to the questionnaire, which corresponds to a response rate of 29 per cent. For the intensive care nurses, we emailed 56 hospitals, 15 of which responded. For the anaesthesia nurses, 64 hospitals were contacted and 29 responded.
Responses were received from all health regions, and the majority were specialist nurses working at local hospitals or university hospitals. The mean age was 47 years. The age range was from 27 to 67 years for the group as a whole, and there was a slightly higher mean age for the anaesthesia nurses. Over 70 per cent had more than six years of experience.
The participants were most positive to the idea that a master’s degree could impact on the area of ‘Knowledge-based practice’. Most (70 per cent) believed that a master’s degree would increase competence in knowledge-based practices.
A total of 61 per cent either agreed or strongly agreed that specialist nurses with a master’s degree were more likely than those with a specialisation qualification to base decisions on research rather than adopting the ‘that’s how it’s always been done’ approach (Table 2).
A master’s degree can stimulate professional development
Within the area ‘Critical thinking and interaction competence’, the strongest agreement was found in the notion that a master’s degree could stimulate colleagues’ professional development, and that the master’s thesis would represent an in-depth study that could benefit the rest of the department (Table 2).
Under the area ‘Skill level and theoretical competence’, between 16 and 29 per cent agreed or strongly agreed that specialist nurses with a master’s degree will become less practical and less hands-on, or that nurses with a master’s degree will have a lower level of theoretical competence within the specialty (Table 2).
There was slightly more variance within the area ‘Recruit and retain’. Approximately 30 per cent of the respondents believed it could be more difficult to recruit people with a master’s degree into the profession. Many (42 per cent) believed that it may be more difficult to retain specialist nurses with a master’s degree in clinical practice (Table 2).
Under the area ‘The need for a master’s degree’, a minority (11 per cent) thought that taking a master’s degree was a waste of time. The majority (64 per cent) believed that converting specialisation courses into master’s degree programmes was a natural development (Table 2).
The responses differed somewhat by gender. The women were significantly more positive to the statements under the areas ‘Knowledge-based practice’ (p = 0.006) and ‘Critical thinking and interaction competence’ (p = 0.00) than the men.
The men were also significantly more negative to the area ‘Recruit and retain’ (p = 0.04) and ‘The need for a master’s degree’ (p = 0.00) than the women (Table 3).
There was considerable agreement in all areas between the anaesthesia and intensive care nurses, however the intensive care nurses expressed somewhat more concern about the ‘recruit and retain’ aspect (p = 0.02) (Table 3).
The local hospitals were more concerned
The respondents’ answers differed somewhat depending on the type of hospital they worked at. The greatest disparity was between university hospitals and local hospitals.
The respondents at the local hospitals were significantly more concerned about the consequences of a master’s degree in the areas ‘Recruit and retain’ and ‘The need for a master’s degree’ compared with the university hospital staff (Table 3).
Respondents from the South-Eastern Norway Regional Health Authority were less concerned than those in the other health regions within the area ‘Skill level and theoretical competence’ (p = 0.05), while Northern Norway Regional Health Authority was more concerned than the South-Eastern Norway Regional Health Authority within the area ‘Recruit and retain’ (p = 0.003).
The teaching staff were generally more positive towards a master’s degree than clinical nurse educators, managers and specialist nurses (Table 3).
Discussion
Overall, the majority of the respondents in the study agreed that specialist nurses with a master’s degree will be better equipped to adopt knowledge-based practices.
Nevertheless, we found that the managers, clinical nurse educators and teaching staff were more positive than the specialist nurses to the idea that a master’s degree provides a better basis for knowledge-based practice. This may partly be due to the fact that more people in these groups have a master’s degree and are aware of the competence it can give them.
Specialist nurses without a master’s degree have less knowledge of what a master’s degree entails, and are less aware of the competence attained from the different forms of learning at master’s degree level.
Senior managers in health trusts and the employers’ association Spekter, on the other hand, are sceptical to a master’s degree being the only approved specialist education (23).
The majority believed that specialist nurses with a master’s degree will stimulate professional development and provide expertise that can benefit the rest of the department.
In the area ‘Critical thinking and interaction competence’, the respondents were mostly positive about the consequences of a master’s degree. The majority believed that specialist nurses with a master’s degree will stimulate professional development and provide expertise that can benefit the rest of the department.
The specialist nurses were nevertheless less positive compared with those in other positions. This may be because fewer of the specialist nurses have a master’s degree compared to those in other positions.
This could impact on the ability to assess the extent to which a master’s degree increases competence in critical thinking and interaction. There was also a significant difference in the responses in this area depending on the type of hospital the respondents worked at.
The university hospitals were most positive
The respondents from the university hospitals were significantly more positive about the consequences of a master’s degree compared with the respondents at the local hospitals, but there was no regional difference.
This may be partly due to the fact that the university hospitals have a greater responsibility than the local hospitals for educating different groups of healthcare personnel over and above treating patients. They therefore have more experience with the positive consequences of education.
Few believed that a master’s degree will lead to less practical specialist nurses.
Few believed that a master’s degree will lead to less practical specialist nurses, that they will be less hands-on, or that nurses with a master’s degree will have a lower level of theoretical competence within the specialty. Teaching staff were significantly less concerned than the other groups that the master’s degree programme would take nurses away from the field of practice.
We assume that the teaching staff have more insight into and influence on the content of the master’s degree than the other groups. They work directly with preparing plans and content in education, while the other groups have less influence and insight into this work.
The most senior hospital managers and the employers’ association Spekter, on the other hand, expressed concern that academicisation will be at the expense of necessary practical competence (24).
Within the area ‘Recruit and retain’, more than half (57.5 per cent) stated that higher entry requirements for theoretical competence could lead to fewer good practitioners applying, but only 30 per cent thought that it would be more difficult to recruit nurses into the profession. The entry requirements for master’s degree programmes vary.
Entry requirements for master’s degrees are the same as for specialisation courses at most educational institutions (e.g. the University of Agder and the University of Stavanger). The aforementioned concern is therefore unfounded for most educational institutions.
A master’s degree is needed in clinical practice
The question is, what is a ‘good practitioner’? One of the characteristics of a good practitioner is a high level of theoretical competence that is applied directly in practice and can be used to justify choices and decisions that are made in practical patient care (25).
The respondents believe that it may be difficult to keep specialist nurses with a master’s degree ‘at the patient’s bedside’, and that they will seek other positions after completing their education. This view is likely based on the fact that there are not currently many specialist nurses with a master’s degree.
Experiences to date show that those who have a master’s degree have tended to seek positions in management, clinical nurse education or teaching. A master’s degree is either an advantage or a requirement in these positions. Compared to the anaesthesia nurses, the intensive care nurses believed that it could be more difficult to recruit and retain specialist nurses.
Once again, it was the teaching staff who expressed the least concern, and the specialist nurses who expressed the most concern. One explanation may be that it is the specialist nurses who have direct patient contact, and who notice when there are recruitment problems or if staff turnover in the department is increasing.
Northern Norway Regional Health Authority was more concerned than the South-Eastern Norway Regional Health Authority within the area ‘Recruit and retain’.
The difference between South-Eastern Norway Regional Health Authority and Northern Norway Regional Health Authority was that respondents from the latter were more concerned that it might be more difficult to recruit and retain specialist nurses. This can possibly be explained by this health authority’s generally smaller supply of specialist nurses.
Within the area ‘The need for a master’s degree’, a generally positive attitude to a master’s degree emerged. This was supported by the majority agreeing that converting the existing specialisation courses to master’s degree programmes is a natural development.
It is already decided that Norway will have three degree structures: bachelor, master and doctorate (5), and it should go without saying that education pathways for specialist nurses follow this framework. Academic credits should be awarded in specialist nursing education.
The respondents believed that education at master’s level is just as important for specialist nurses with close patient contact.
The majority believed that a master’s degree should not be reserved for clinical nurse educators, and this may be an indication that the respondents believed that education at master’s level is just as important for specialist nurses with close patient contact.
There were different views on the need for a master’s degree, and once again it was the most senior managers of the health trusts that expressed scepticism, partly due to the additional costs (24).
Significant gender disparity
In several areas, men were more critical of the need for a master’s degree than women, particularly in the competence areas of knowledge-based practice, critical thinking and interaction competence.
One explanation may be that, among those with a specialisation qualification, men are more likely than women to believe that they have sufficient knowledge to adopt knowledge-based methods in their work and to take a critical and analytical approach to their discipline and the interaction with colleagues.
There was a significant gender disparity in all individual questions in the area ‘Critical thinking’. The greatest agreement was in relation to the statements that a master’s thesis provides expertise that can benefit the rest of the department, and that a master’s degree better equips nurses for improving practice compared with specialisation courses.
These questions were more general and did not have a strong focus on personal competence, which supports the higher tendency among men to feel less of a need for the competence that a master’s degree can give.
Weaknesses of the study
The study has several weaknesses. The intention was to gain an insight into what anaesthesia and intensive care nurses throughout Norway thought about master’s degrees. The response rate was low.
This may be because many were not given the opportunity to participate, either because the email addresses we were given for their managers were incorrect, or because the managers did not forward the invitation to their employees. We sent a reminder, which increased participation somewhat.
It could be questioned whether the result is representative. It may be that those who responded were particularly interested in educational issues. The results concerning the various health authorities must also be interpreted with caution because some of the regions had few respondents. Despite the low response rate, it is nevertheless a strength of the study that respondents from all regions and different hospitals participated.
We based the questionnaire on statements that emerged in the qualitative interviews, and some statements were of a colloquial nature. This means that several of the formulations could perhaps be misunderstood or interpreted in different ways.
One example is the concept of ‘not hands-on’, which can be understood in several ways; it could mean that they are more interested in a theoretical approach to their discipline, or that they wish to have less direct contact with the patient.
In the statement that more stringent entry requirements for theoretical competence could potentially result in fewer good practitioners applying, there is an assumption that the entry requirements will be higher for a master’s degree. This is not necessarily the case, since many master’s degree programmes have the same entry requirements as specialistion courses.
Conclusion
Both the anaesthesia nurses and the intensive care nurses had generally positive attitudes and perceptions in relation to a master’s degree in anaesthesia and intensive care nursing. The majority believed that converting specialisation courses into a master’s degree programme was a natural development.
Few expressed concern that a master’s degree would mean less practical specialist nurses, but several believed that it may be more difficult to recruit nurses to the profession and retain those with a master’s degree in clinical practice.
A master’s degree will help to boost the clinical perspective through a more critical assessment of current practice and personal actions and mindsets. It will also improve the understanding for viewing the organisation as a whole.
Patients are living longer nowadays. Many have complex comorbidities, treatments are becoming steadily more advanced, and there is reduced interaction between patients and healthcare personnel. This makes it even more important to safeguard the right competence. Nurses with a master’s degree will strengthen the health team’s overall competence and improve patient safety.
Research in the health service is important for raising standards in patient care and in the nursing provided. Specialist nurses with a master’s degree will be vital contributors in the development of knowledge and research in the years ahead.
To oppose the education of specialist nurses at master’s level is not only at odds with internationally approved degree structures, but is also a backwards approach to the future.
References
1. Grønvik CKU, Ulvind I, Bjørkly S. Videreutdanning gjør sykepleiere bedre rustet til å arbeide kunnskapsbasert. Sykepleien Forskning. 2018;13(69520):e-69520. DOI: 10.4220/sykepleienf.2018.69520.
2. Meld. St. 7 (2019–2020). Nasjonal helse- og sykehusplan 2020–2023. Oslo: Helse- og omsorgsdepartementet; 2020. Available at: https://www.regjeringen.no/no/dokumenter/meld.-st.-7-20192020/id2678667/ (downloaded 10.01.2020).
3. Joen Y, Lathinen P, Meretoja R, Leino-Kilpi H. Anaesthesia nursing education in the Nordic countries: literature review. Nurse Educ Today. 2015;35(5):680–8. DOI: 10.1016/j.nedt.2015.01.015.
4. Collins S, Hewer I. The impact of the Bologna process on nursing higher education in Europe: a review. Int J Nurs Stud. 2014;51(1):150–6. DOI: 10.1016/j.ijnurstu.2013.07.005.
5. Forskrift 8. november 2017 nr. 1846 om Nasjonalt kvalifikasjonsrammeverk for livslang læring og om henvisningen til Det europeiske kvalifikasjonsrammeverket for livslang læring 2017. Available at: https://lovdata.no/dokument/SF/forskrift/2017-11-08-1846 (downloaded 10.01.2020).
6. St.meld. nr. 44 (2008–2009). Utdanningslinja. Oslo: Kunnskapsdepartementet; 2009. Available at: https://www.regjeringen.no/no/dokumenter/stmeld-nr-44-2008-2009-/id565231/ (downloaded 10.01.2020).
7. Meld. St. 4 (2018–2019). Langtidsplan for forskning og høyere utdanning 2019–2028. Oslo: Kunnskapsdepartementet; 2018. Available at: https://www.regjeringen.no/no/dokumenter/meld.-st.-4-20182019/id2614131/ (downloaded 10.01.2020).
8. NOU 2018: 2. Fremtidige kompetansebehov I – Kunnskapsgrunnlaget. Oslo: Kunnskapsdepartementet; 2018.
9. NOU 2019: 2. Fremtidige kompetansebehov II – Utfordringer for kompetansepolitikken. Oslo: Kunnskapsdepartementet; 2019. Available at: https://www.regjeringen.no/no/dokumenter/nou-2019-2/id2627309/ (downloaded 10.01.2020).
10. LeGrow K, Espin S. Critical reflection on practice development, beginning explorations of the connectedness between patient – centered care, practice development and advanced nursing competencies to promote professional development. IPDJ. 2017;7(2). Available at: https://www.fons.org/Resources/Documents/Journal/Vol7No2/IPDJ_0702_08.pdf (downloaded 10.01.2020).
11. Universitets- og høgskolerådet. Merverdi av master i sykepleie. Rapport fra nasjonal fagstrategisk enhet for utdanning og forskning innen helse- og sosialfag. Oslo: Universitets- og høgskolerådet; 2016.
12. Cotterill-Walker SM. Where is the evidence that master's level nursing education makes a difference to patient care? A literature review. Nurse Educ Today. 2013;32(1);57–64. DOI: 10.1016/j.nedt.2011.02.001.
13. Norsk Sykepleierforbund. Fremtidens spesialsykepleiere. Krav til spesialiststruktur, utdanningskvalitet og dimensjonering 2016. Available at: https://www.nsf.no/Content/2976737/cache=1465980149000/Fremtidens_spesialsykepleier_pdf.pdf (downloaded 10.01.2020).
14. NOU 2008: 3. Sett under ett – Ny struktur i høyere utdanning. Oslo: Kunnskapsdepartementet; 2008. Available at: https://www.regjeringen.no/no/dokumenter/NOU-2008-3/id497182/?ch=1 (downloaded 10.01.2020).
15. Millberg LG. Akademisering av specialistsjuksköterskans utbildning i Sverige. Karlstad: Fakulteten for samhälls- och livsvetenskaper. Karlstads Universitet; 2012. Available at: https://www.diva-portal.org/smash/get/diva2:570330/FULLTEXT01.pdf (downloaded 10.01.2020).
16. Millberg LG, Berg L, Brämberg EB, Nordström G, Öhlén J. Academic learning for specialist nurses: a grounded theory. Nurse Educ Pract. 2014;14(6):714–21. DOI: 10.1016/j.nepr.2014.08.008.
17. Song G, Xing X, Gui-fang G. A systematic review of the impact of master’s educated nurses on inpatient care. Intern J Nurs Scienc. 2015;2(4):414–21. DOI: 10.1016/j.ijnss.2015.10.003.
18. Clark L, Casey D, Morris M. The value of Master's degree for registered nurses. BJN. 2015;24(6). DOI: 10.12968/bjon.2015.24.6.328.
19 Lerdal A. Vi trenger funksjonsorienterte mastergrader. Sykepleien Forskning. 2014;9(2):103. DOI: 10.4220/sykepleienf.2014.0103.
20. Skogsaas B. Praksisveilederes refleksjoner om akademisering av AIOK videreutdanningene. Sykepleien Forskning. 2016;(1);54–64. DOI: 10.4220/sykepleienf.2016.56818.
21. Skogsaas B, Valeberg BT. Hva mastergradskompetanse kan bidra med i klinisk praksis: en kvalitativ studie. Sykepleien Forskning. 2017;12(63495):e-63495. DOI: 10.4220/sykepleienf.2017.63495.
22. Kline P. Handbook of Psychological Testing. 2nd ed. New York, NY: Routledge; 2000.
23. Ulvestad AK. Mastergraden – ikke nødvendigvis kvalitet. Oslo: Fontene Forskning; 2019. Available at: https://fontene.no/fagartikler/mastergraden--ikke-nodvendigvis-kvalitet-6.47.664922.b82b5df383 (downloaded 24.05.2020).
24. Innpasning av videreutdanning i mastergrad. Rapport fra arbeidsgruppe nedsatt av Universitets- og høgskolerådet 14.12.2014. Available at: https://www.napha.no/attachment.ap?id=3052 (downloaded 26.05.2020).
25. Furåker C, Nilsson A. Kompetens, kunskap och lärande. In: Leksell J, Lepp M, eds. Sjuksköterskans kärnkompetanser. Stockholm: Liber AB; 2013.









Comments