Diabetes specialist nurses’ experiences when training patients in the use of insulin pump therapy
Diabetes specialist nurses have a strong feeling of responsibility for the patient and find it challenging to keep up to date with all the functions of some of the insulin pumps.
Background: Research shows that the prevalence of type 1 diabetes is increasing, while the number of people who use technical medical equipment such as an insulin pump is also rising. Consequently, diabetes specialist nurses in both the primary and specialist health services will more frequently encounter people who use an insulin pump. Patients have now better access to information on technical medical equipment, which poses a challenge to the expertise of diabetes specialist nurses. Providing training and guidance are key tasks for diabetes specialist nurses in the specialist health service.
Objective: The objective of the study was to gain more knowledge about the experiences of diabetes specialist nurses when providing training and guidance in the use of insulin pump therapy.
Method: This is a qualitative study with a sample of ten diabetes specialist nurses from various diabetes outpatient clinics in the specialist health service. Four different counties in Norway are represented. The informants are registered nurses who have taken specialised courses comprising at least 30 ECTS in diabetes treatment and care, and who have an average of 18 years of work experience in the field. We undertook semi-structured individual interviews and analysed the data material using content analysis.
Results: The diabetes specialist nurses felt considerable responsibility for individual training and guidance in insulin pump therapy, both during the actual training and afterwards. At the same time, they said that it was challenging to keep up to date with all the functions of some of the pumps.
Conclusion: The study shows that even though diabetes specialist nurses have long experience of diabetes treatment and care for this patient group, they want and need to be regularly updated on technical medical equipment such as insulin pumps. Patient follow-up is resource-intensive, and the diabetes specialist nurses feel a responsibility to remain accessible to patients at the commencement of insulin pump therapy. In order to maintain their training and guidance skills, they need to exchange experiences regularly with other diabetes specialist nurses as well as with others involved.
Diabetes treatment for people with type 1 diabetes (DM1) changed during the 20th century from the time of the discovery of insulin around 1920 to the introduction of the insulin pump at the end of the 1970s (1, 2). Some insulin pumps have integrated continuous glucose monitoring (CGM), which measures tissue glucose (3).
The number of people with type 1 diabetes using insulin pump therapy is increasing, and it is believed that numbers will continue to increase (4). There is a wide variation in the use of the insulin pump in European countries (5, 6). The Norwegian Diabetes Register for Adults shows that 26–34 per cent of those with DM1 use insulin pump therapy, depending on gender and age group (6).
Safe use of an insulin pump requires rigorous training by specialised healthcare personnel as well as the active participation of the patient (1, 2, 7). The insulin pump is a technical aid in the treatment, and the person’s own mastery of their life situation is decisive for the outcome of the disease (7, 8).
Todres et al. demonstrate that the use of an insulin pump may pose a challenge for patients to begin with, but in due course the technology can contribute to a higher quality of life, a greater feeling of responsibility and better mastery of their own situation (9).
Patients vary in terms of their ability to learn and remember the information they have been given. Continual evaluation of knowledge, technical skills and behaviour are vital for patient safety and the optimalisation of insulin pump use (10).
Support from healthcare personnel, structured training and guidance, whether provided to individuals or groups, are recommended for all those with diabetes in order to improve the outcome of type 1 diabetes (10, 11). While the individual medical treatment is prescribed by a doctor, the task of the specialist diabetes nurse (DSN) is to train and guide those with diabetes in the treatment measures prescribed (12).
Studies show that nurses need knowledge about both the benefits of insulin pump therapy and the acute complications that may arise when using the pump. They also need training in the technical aspects of using the insulin pump (6, 13). A trained specialist team must follow up those using an insulin pump (9).
Both insulin pumps and CGM are in a continuous process of development and are more precise and more user-friendly than earlier. Moreover, they can be linked to platforms that can be used to download data. In their everyday lives, those with DM1 need the assistance of healthcare personnel to interpret the data and make necessary adjustments (2).
Schaffer found that routines varied regarding how often data was downloaded from insulin pumps with CGM. A total of 56 per cent of healthcare personnel responsible for diabetes care downloaded data from insulin pumps (with CGM) at least once after the commencement of therapy while 27 per cent regularly downloaded data from individual patients’ insulin pump (2).
James et al. found that DSNs wanted to be in a position to offer patients insulin pumps with CGM, use digital platforms and provide video consultations. However, the reported use of the technology was lower than the stated intentions of the DSNs. Their own training in the use of insulin pumps and their level of confidence and competence were factors that significantly impacted on the training received by the patient group (14).
In another study, James et al. showed that DSNs found it difficult to keep up to date on advanced functions in relation to insulin pumps, CGM and available apps (10).
The objective of the study
There are currently few Nordic studies dealing with the nursing perspective on the training of insulin pump therapy users. The objective of the study was, therefore, to acquire more knowledge about diabetes specialist nurses’ experiences when training patients in the use of insulin pump therapy.
Method
We used a qualitative design since we wanted to document the experiences of DSNs. Data collection was based on semi-structured individual interviews. Qualitative methods are characterised by small samples and a close relationship with the informants (15).
The first author is a DSN with experience of the specialist health service. The second author, who has joint responsibility for the study, has comprehensive knowledge of qualitative research methods and has provided input throughout the entire research process.
The first author sent a request and written information to hospitals in four different Norwegian counties. Heads of department in the specialist health service recruited DSNs who were interested in participating in the study. The inclusion of different hospitals provides more nuanced and richer data material based on systemic differences in the hospitals (16).
Informants
The inclusion criteria for the study were: nurses with specialised training in diabetes therapy and working in the specialist health service. A total of ten informants from six different hospital trusts contacted the first author. The diabetes teams in the different health trusts varied in size, but a minimum requirement was that they included a doctor responsible for diabetes patients, a DSN and a nutritionist.
Most DSNs estimated that 40–60 per cent of those with DM1 who were monitored by the diabetes outpatient clinics had an insulin pump. Some informants believed that the percentage was as low as 20 per cent, while a few did not know the percentage.
The average age of the informants was 52 years, and they had on average 18 years of work experience in the field. The informants' DSN positions ranged from 50 to 100% full-time equivalent hours (FTEs). None of the informants withdrew from the study.
Interviews
We conducted individual, semi-structured interviews (16) from November 2017 until February 2018. Some of the interviews took place at the informant’s workplace while others were carried out at a conference on diabetes. All the interviews were agreed beforehand, and the participants took part in person. We used suitable rooms and a dictaphone to record the interviews.
The interview guide contained introductory questions about nursing position, work experience and the percentage of patients with DM1 using insulin pump therapy. It included one open-ended question in which the DSNs were asked to describe what it was like being able to offer insulin pumps as a treatment method.
We also devised supplementary questions covering the experiences of the informants in relation to their own training in the use of different insulin pumps, downloading data from the insulin pump/CGM and documentation.
Data analysis
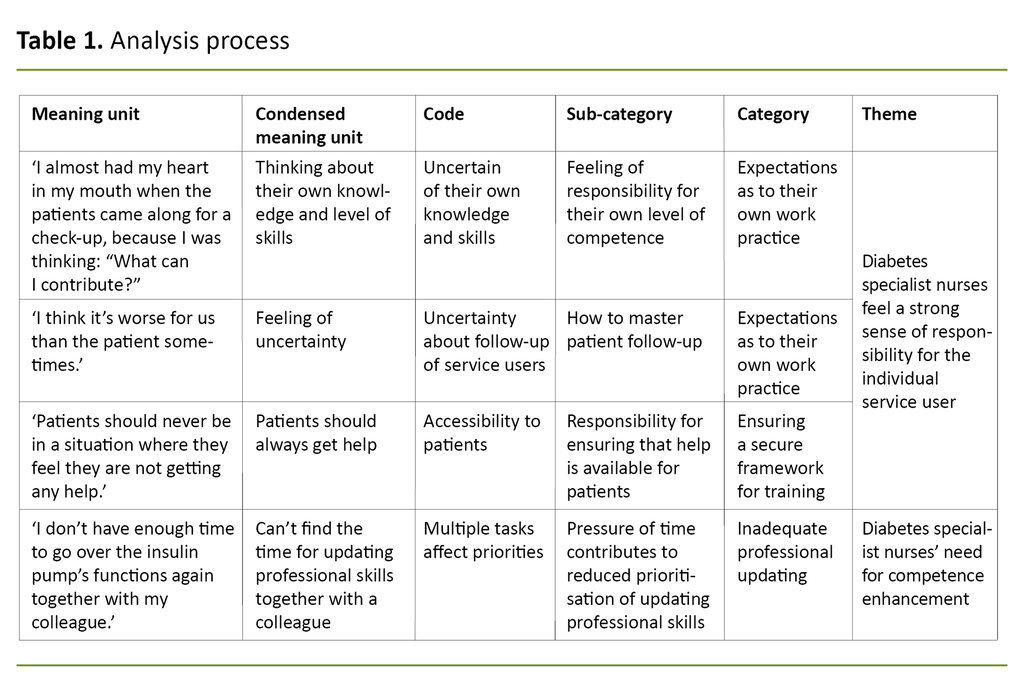
We used Graneheim and Lundman’s qualitative content analysis (17), and read the text of the interview to form an overall impression of the content. Then the meaning units were derived from the transcribed text based on their relevance in relation to the research question. This was noted in a self-composed table.
The meaning units were then condensed and sorted into codes according to their content. This systematic and continuous analysis process elicited three categories and two themes (Table 1).
Ethics
We submitted an application to the Norwegian Centre for Research Data prior to the start of the project (project number 56455). After being given oral and written information about the study, the informants signed the consent form. The data was stored on a password-protected computer, and the audio recordings were deleted following transcription (16).
Results
The DSNs felt a considerable degree of responsibility for people with DM1, both during the training and in the ensuing period. They also wanted to discuss various issues regarding training and the follow-up of insulin pump therapy with other partners.
Diabetes specialist nurses feel a strong sense of responsibility for the individual service user
Providing training and guidance in the use of the insulin pump is a complex task. The DSNs were interested in ensuring that each individual patient received individual adaptation. It varied how often they carried out training in the use of the insulin pump.
Several of the DSNs spoke of demanding workdays when they felt alone with the responsibility because they often worked on their own when training patients to use the insulin pump: ‘I often feel exhausted after the insulin pump start’ (informant 1).
The type of training the DSNs gave patients varied. Some provided training in the basic functions when the insulin pump was introduced while others described all the pump’s different functions. They also reviewed the essential pump accessories.
Some of those with DM1 lived at a considerable distance from the diabetes outpatient clinic and the DSNs provided follow-up either by telephone or email.
The DSNs found that the patients should actively use as many of the pump’s functions as possible during the first year. If not, there was little likelihood of the patients’ learning to use the insulin pump’s full range of options; ‘The options offered by the insulin pump must be highlighted’ (informant 10).
The DSNs felt considerable responsibility for offering support and being easy to contact in order to give guidance to the patient after insulin pump start, since they wanted all patients to master insulin pump therapy in their everyday lives.
Most of the DSNs gave the patients their private telephone number.
After the insulin pump start, it was vital to be accessible to patients, both during and after working hours. Being accessible meant either being present in person at the diabetes outpatient clinic or being available on the telephone. The DSNs found that patients dared to experiment more with the insulin pump when they were assured of back-up, and were of the opinion that the patients then learned more quickly.
Most of the DSNs gave the patients their private telephone number: ‘I want to be available for the patients, because that gives them a sense of security, and I want to be part of the learning process. You get better insight into their everyday lives,’ (informant 2) and ‘The patients must know that we’re there for them,’ (informant 5).
The commencement of insulin pump therapy and following up patients during the consultations required extra nursing resources. It was important to go over the various functions of the insulin pump again in later consultations.
The DSNs said that it took time to download the data from the pumps and that the data could be difficult to interpret: ‘It’s time-consuming to get a full overview of all the data downloaded from the insulin pump,’ (informant 6).
The patients themselves were also meant to acquire an understanding of the downloaded data during the time they spent with the DSN. Meanwhile, this should not be the main focus of the consultation. The DSNs wanted to view patients and their situation as a whole. They also wanted to encourage patients to identify any trends in the data material themselves.
Since blood sugar is affected differently in different patients, the patients themselves could suggest appropriate adjustments of insulin in a specific time period. Patient participation could also help to increase awareness of the association between blood sugar level and any events that took place during the period in question.
Diabetes specialist nurses’ need for competence enhancement
Diabetes specialist nurses said that it took several years for them to feel confident about the use of the insulin pump. Several of them said that they took it home with them in order to go over the procedure and the pump’s different functions prior to pump start. They wanted to be well prepared and updated with regard to the pump that they were to train patients to use.
Insulin pumps can have different menus even though the functions are the same: ‘You ought to have worked as a diabetes specialist nurse for some years before you start giving guidance on insulin pumps,’ (informant 8), and ‘So if you’re going to train a patient to use an insulin pump, you should know it from A to Z,’ (informant 8).
They took the insulin pump home with them in order to go over the procedure and the pump’s different functions prior to pump start.
The DSNs had a need for regular updates on all the types of insulin pumps available and to go over their use again. They stated that only a small number of healthcare personnel otherwise in both the specialist and the primary health services were able to handle an insulin pump.
The time available for DSNs to update their knowledge of the different insulin pumps and the treatment of the individual patient depended on several factors, for example FTE percentage, diabetes team size and workload: ‘It’s a lonely job, I work on my own a lot of the time,’ (informant 1).
The majority of the DSNs had a part-time position. They believed that it was an advantage to have positions with a larger FTE percentage to ensure continuity in the work: ‘One example of the benefits of having positions with more working hours could be that you have a better overview at all times of which service users need guidance, and what individuals need guidance on,’ (informant 7).
DSNs believed that it was an advantage to have positions with a larger FTE percentage.
There was a variation in how much time DSNs allocated to each individual consultation. Some were able to determine the length of the consultation themselves, whilst others had limited time available to them.
The DSNs collaborated to different degrees with the various specialist companies that delivered the insulin pumps. Some of them invited the product specialist to take part in the training if they were unsure about the pump’s technical functions.
They also said that they would have felt more confident during their first solo patient training session if they could have telephone support available throughout: ‘I know some of the insulin pumps better than others,’ (informant 5).
‘If the information I give the patient could have been confirmed by someone who is familiar with the technical aspects of the pump, maybe I would grow more confident every time I help a patient with the start-up,’ (informant 3).
‘We depend on the companies to keep us updated,’ (informant 9).
One DSN in a large diabetes team remarked as follows: ‘Everyone must have a genuine interest in diabetes and the technical equipment, and everyone must contribute equally to keeping the team updated at all times,’ (informant 10).
The DSNs mentioned the advantages of being in a team with several members and being able to advise each other. It also meant that more people could take part in the consultation with each patient, and that they could discuss the data downloaded from the pumps.
They wanted more opportunities to exchange experiences, saying that this could help the individual DSN to feel a sense of mastery and confidence.
Discussion
It is clear that the DSNs adapt insulin pump training to suit the individual patient and focus on making them feel safe and well looked after, particularly after the patient has begun to use the insulin pump.
Diabetes specialist nurses’ own expectations of service user training and follow-up during insulin pump therapy
DSNs’ expectations of their own role and their level of competence vary, impacting on the individual patient’s learning situation.
An earlier study shows the importance of focusing on how patients can feel secure regarding their own treatment, stating that this must be adapted to the needs and preferences of the individual. The findings in the study show that the DSNs emphasise the creation of good relationships with the patient and a secure care framework as a vital component of the training and guidance (7).
Earlier research demonstrates that good routines and habits in everyday life are important for patients (18). Healthcare personnel’s support is absolutely essential in improving the outcome of type 1 diabetes (8). The fact that the DSN creates a secure setting by being easily accessible and being there for the patient may be crucial for the patients’ actions and the choices they make in their everyday lives.
The dialogue between the DSN and the patient in terms of individual goals may make the patient more aware of treatment results and can be positive for the patient psychologically (19, 20).
A number felt exhausted and alone in their professional lives.
The DSNs in our study described a strong sense of responsibility for their patients and high expectations of themselves. A number felt exhausted and alone in their professional lives. Often they gave important advice without back-up, even though they did this in agreement with the patient.
According to the nursing theorist Patricia Benner, DSNs can be regarded as being at different stages of clinical competence – from novice to expert (21). If we compare Benner’s theory (21) with the statements of the DSNs in this study, none of them regarded themselves as experts. However, they did see themselves as competent to carry out their tasks, but it was difficult to achieve a higher level of competence.
A study by Sweeney et al. found that nurses in the specialist health service needed to increase their knowledge of insulin pump use (22), and this is also underlined by the DSNs in this study. The specialist literature indicates that if DSNs feel unsure about the training they give or if they find that they do not have enough time to give the patient guidance, this may impact on the patient’s perceptions of the quality of insulin pump training (21).
The DSNs said that they wanted to be accessible, giving their private telephone numbers to many of their patients after the start-up of insulin pump therapy. Although this practice undoubtedly gives the patient a greater sense of security, the nurses’ strong sense of responsibility and their desire to help by advising patients both during and after working hours are surprising.
Diabetes specialist nurses need to be professionally updated
The diabetes specialist nurses in this study described the percentage of people with DM1 who received follow-up in the diabetes outpatient clinic. Several of the nurses said that they took the insulin pumps home with them to go over various functions, so that they themselves became more confident about the options and menus offered by the individual pumps.
Patients must ‘find their own way’ to independence and mastery when using an insulin pump. Using technical aids is complex, and if the patient does not receive adequate training, this may result in adverse events.
Organisational factors such as time pressure, lack of nursing resources, part-time positions in the field and inadequate updating in the use of the insulin pumps resulted in DSNs taking the devices home with them. These organisational factors can be compared with the results of a training programme that was initiated at a hospital in Boston in the United States. Here it was found that the nurses had better knowledge and skills with regard to the use of insulin pumps after they had worn them at home themselves for a few days (23).
Everett and Kerr pointed out that downloading data either in the patient’s home or together with the healthcare personnel had led to greater understanding and insight as well as better control of the patient’s diabetes. One of the challenges was to structure the working day in such a way that this did not take up more time or require more staff (24).
The findings in our study show that DSNs got in touch with other colleagues or product specialists if they felt uncertain about their own competence regarding the pumps. They feel more confident of their ability to train patients and give them guidance in the use of the insulin pump in diabetes outpatient clinics with a large diabetes team.
Hilsted et al. confirm the need for cooperation between the companies delivering insulin pumps and the specialist health service (3). The Health Personnel Act prescribes cooperation with other healthcare personnel if this is indicated by the needs of the patient (25). This is also mentioned in the ethical guidelines for RNs and in the DSN role description (12, 26).
Benner distinguished between ‘competent’ and the next level up, ‘proficient’, by including active teaching (21). This is something that the DSNs lack in their everyday work. Receiving tuition and exchanging experiences are important for them, since this can make them feel more confident about the training they give patients in the use of the insulin pump.
The strengths and weaknesses of the study
The interviews conducted with experienced DSNs from different diabetes outpatient clinics in several Norwegian counties are a strength of the study. Individual interviews enabled us to understand the experiences of the individual informant and indirectly provided information about how they handled the technical medical equipment (27).
Another strength of the study is the fact that the first author has worked as a DSN even though this may have led to biased attitudes that may have affected the results (28). In order to avoid influencing the informants, the first author was mindful of her own level of knowledge and experiences as a diabetes specialist nurse.
In order to safeguard the informants’ perspectives and self-understanding, the first author made every effort to remain neutral before and during the interviews. The first and second author had different backgrounds, which we regard as a strength of the study when it comes to identifying different nuances in the data material.
Conclusion
According to the National Action Plan for Diabetes 2017–2021, there is a need to establish what competence, resources and staffing will be required in diabetes outpatient clinics in the years ahead (29). This study shows that Norwegian DSNs in the specialist health service have a strong sense of responsibility for ensuring that all patients receive the help they need in relation to insulin pump therapy.
The study supports earlier research showing that DSNs in charge of training patients need to receive regular updates in the use of the insulin pump. RNs who meet these patients in other settings also need to increase their level of knowledge in this respect.
Implications for practice
DSNs need resources to work on training and guidance for this patient group. They need psychosocial support and to be able to exchange experiences with other DSNs. Not all diabetes outpatient clinics have a full-fledged diabetes team where they can discuss different issues.
References
1. Chatteriee S, Davies MJ. Current management of diabetes mellitus and future directions in care. Postgraduate Medical Journal. 2015;91(1081):612–21.
2. Schaffer R. New diabetes devices improve connectivity, but patient, provider education needed. Endocrine Today. 2016;14(2):1–14.
3. Hilsted J, Christiansen JS, Borch-Johnsen K, red. Diabetes – sygdom, behandling og organisation. Copenhagen: Munksgaard; 2016.
4. Renard E. Insulin pump use in Europe. Diabetes Technol Ther. 2010;suppl. 1(S1):29–32.
5. Kampmann U, Madsen LR, Bjerg L, Witte DR, Hasselstrøm K, Østergård T, et al. Prevalence and geographical distribution of insulin pump therapy in the Central Denmark Region and its association with metabolic parameters. Diabetes Research and Clinical Practice. 2018;141:148–55.
6. McKnight JA, Wild SH, Lamb MJE, Cooper MN, Jones TW, Davis EA, et al. Glycaemic control of type 1 diabetes in clinical practice early in the 21st century: an international comparison. Diabetic Medicine. 2015;32(8):1036–50.
7. Reidy C, Bracher M, Foster C, Vassilev I, Rogers A. The process of incorporating insulin pumps into the everyday lives of people with type 1 diabetes: a critical interpretive synthesis. Health Expectations. 2018;21(4):714–29.
8. Bode BW, Tamborlane WV, Davidson PC. Insulin pump therapy in the 21st century. Strategies for successful use in adults, adolescents, and children with diabetes. Postgraduate Medicine. 2002;111(5):69–77.
9. Todres L, Keen S, Kerr D. Continuous subcutaneous insulin infusion in type 1 diabetes: patient experiences of ‘living with a machine’. Diabetic Medicine. 2010;27(10):1201–4.
10. James S, Pery L, Gallagher R, Lowe J. Diabetes educators: perceived experiences, supports and barriers to use of common diabetes-related technologies. Journal of Diabetes Science and Technology. 2016;10(5):1115–21.
11. Poole R. Type 1 diabetes in adults: new NICE guidance on diagnosis and management. Practical Diabetes International. 2015;32(8):279–80.
12. NSFs faggruppe for diabetessykepleiere. Funksjonsbeskrivelse for diabetessykepleiere. Oslo: Norsk Sykepleierforbund; 2006. Available at: https://www.nsf.no/sites/default/files/groups/subject_group/2019-11/funksjonsbeskrivelse-for-diabetessykepleiere.pdf (downloaded 01.06.2018).
13. Leonhardi BJ, Boyle ME, Beer KA, Seifert KM, Bailey M, Miller-Cage V, et al. Use of continuous subcutaneous insulin infusion (insulin pump) therapy in the hospital: a review of one institution's experience. Journal of Diabetes Science and Technology. 2008;2(6):948–62.
14. James S PL, Perry L, Gallagher R, Lowe J. Diabetes educator's intended and reported use of common diabetes-related technologies. Journal of Diabetes Science and Technology. 2016;10(6):1277–86. DOI: 10.1177/1932296816646798
15. Malterud K. Kvalitative forskningsmetoder for medisin og helsefag. 4th ed. Oslo: Universitetsforlaget; 2017.
16. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 3rd ed. Oslo: Gyldendal Akademisk; 2015.
17. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–12.
18. Mæland JG. Forebyggende helsearbeid. Folkehelsearbeid i teori og praksis. Oslo: Universitetsforlaget; 2016.
19. Vaaler S, Møinichen T, eds. Diabeteshåndboken. Oslo: Gyldendal Akademisk; 2014.
20. Haug J. Diabetespsykologi: samspillet mellom kropp og sinn. Oslo: Gyldendal Akademisk; 2017.
21. Benner P. Fra novise til ekspert: dyktighet og styrke i klinisk sykepleiepraksis. Oslo: Tano Aschehoug; 1995.
22. Sweeney TJ, Kenny DJ, Schubert CC. Inpatient insulin pump therapy. Journal for Nurses in Professional Development. 2013;29(2):84–9.
23. Einis S B, Mednis GN, Rogers J E, Walton DA. A program to train inpatient pediatric nurses in insulin pump use. American Journal of Nursing. 2011;111(7):51–5.
24. Everett J, Kerr D. Telehealth as adjunctive therapy in insulin pump treated patients: a pilot study. Practical Diabetes International. 2010;27(1):12.
25. Lov 2. juli 1999 nr. 64 om helsepersonell (helsepersonelloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-64?q=helsepersonellov (downloaded 01.06.2018).
26. Norsk Sykepleierforbund (NSF). Yrkesetiske retningslinjer. Oslo: NSF; u.å. Available at: https://www.nsf.no/vis-artikkel/2193841/17102/Yrkesetiske-retningslinjer (downloaded 01.06.2018).
27. Dalen M. Intervju som forskningsmetode – en kvalitativ tilnærming. Oslo: Universitetsforlaget; 2004.
28. Elo S, Kääriäinen M, Kanste O, Pölkki T, Utriainen K, Kyngäs H. Qualitative content analysis: a focus on trustworthiness. SAGE Open. Jan. 2014. DOI: 10.1177/2158244014522633
29. Helse- og omsorgsdepartementet. Nasjonal diabetesplan 2017–2021. Oslo: Helse- og omsorgsdepartementet; 2017. Available at: https://www.regjeringen.no/contentassets/701afdc56857429080d41a0de5e35895/nasjonal_diabetesplan_171213.pdf (downloaded 15.11.2021).










Comments