Inadvertent perioperative hypothermia and day surgery – nurse anaesthetists’ experience
Body temperature was measured differently and the routines were not the same. Provision should be made for a practice ensuring that staff have the necessary equipment and time to prevent inadvertent perioperative hypothermia.
Background: Patients undergoing surgery are susceptible to inadvertent perioperative hypothermia and have, therefore, an increased risk of complications. Prevention and treatment of inadvertent hypothermia are well documented. Nevertheless, research shows that measures that prevent inadvertent hypothermia are not always carried out.
Objective: To acquire greater knowledge and understanding of how nurse anaesthetists prevent inadvertent perioperative hypothermia in day surgery patients.
Method: The study has a qualitative, descriptive design using focus group interviews as a method. Two focus group interviews were conducted. The sample consisted of 13 nurse anaesthetists from day surgery units at two different hospitals. We used Malterud’s systematic text condensation strategy in the analysis.
Results: The participants found that there was insufficient standardisation of body temperature measurement, and the use of the checklist ‘Safe surgery’ was practised differently. There were different understandings of resources such as time, available equipment and financial aspects at the different hospitals – and this could impact on efforts to prevent inadvertent hypothermia. The participants mainly indicated that cooperation with the rest of the team was good, but that sometimes there were conflicting interests. The nurse anaesthetists provided compassionate care to the patient, covering their head, heating intravenous fluid and warming blankets and socks.
Conclusion: There was insufficient standardisation in respect of preventing inadvertent perioperative hypothermia among day surgery patients. Moreover, there were differences in how temperatures were measured and the units’ routines. Provision should be made for a practice whereby staff have the necessary equipment and time to prevent inadvertent hypothermia. A question on body temperature measurement should be included in the ‘Safe Surgery’ checklist in all hospitals.
Patients undergoing surgery are susceptible to inadvertent perioperative hypothermia (1–5), particularly in the case of abdominal surgery (6). Hypothermia is defined as having a core temperature below 36 °C (7). Patients undergoing surgery should have a normal temperature, and the core temperature should be measured in the case of general anaesthesia lasting longer than 30 minutes (8, 9).
During surgery under general anaesthesia, patients lose the ability to regulate their own body temperature. Anaesthetic drugs affect the hypothalamus, resulting in the impairment of the body’s own thermoregulation (5, 8, 9).
The greatest heat loss occurs in the first hour following the induction of anaesthesia (5, 7, 8, 10). The patient’s environment affects their body temperature (4, 9), and the patient loses heat to the environment through radiation, evaporation and the administration of cold fluids (5, 10). Moreover, the temperature in the operating theatre is often low to improve working conditions for the surgical team (5, 10).
Perioperative hypothermia may entail a higher risk of complications such as surgical site infections, cardiac events, increased blood loss and a need for blood transfusions in addition to a longer period of postoperative hospitalisation (4, 5, 8, 9). Factors such as age, level of morbidity, BMI and length of surgery impact differently on the degree to which the patient is susceptible to hypothermia (11).
Guidelines for nurse anaesthetists
The Norwegian Directorate of Health (12) states that planned day surgery operations constitute a large percentage of surgical interventions in Norway. Day surgery is an effective process whereby the patient is admitted to hospital and discharged the same day (13).
The number of day surgery operations increased in the period from 2013 to 2017, and in 2017, planned day surgery operations accounted for between 46 and 75 per cent of the total number of surgical interventions in all health trusts in Norway (12, 14). Nurse anaesthetists have a duty to comply with the Norwegian standard for the safe practice of anaesthesia (15) and Basic guidelines for nurse anaesthetists (16), which set out the standards for the practice of anaesthetic nursing.
The National Institute for Health and Care Excellence (NICE) is one of several international bodies that issue guidelines with a clear definition of inadvertent perioperative hypothermia and recommendations on how to prevent it (7). Moreover, the ‘Safe Surgery’ checklist should be used to ensure that measures are taken to prevent its occurrence during surgery (14).
Earlier research on the topic
Health personnel’s knowledge is vital in preventing hypothermia in individual patients (4). Nevertheless, research shows that not everyone measures body temperature pre-, intra-, and post-operatively (4, 17). In their study, Giuliano and Hendricks (3) found varying and sometimes insufficient knowledge about implementing preventive measures and which patient groups were more frequently susceptible to inadvertent hypothermia.
We found many quantitative studies on hypothermia and its outcomes (1, 2). However, there is little qualitative research on nurse anaesthetists’ experience of preventing inadvertent hypothermia. In their qualitative studies, Loe and Moe (17), and Honkavuo and Loe (18) found that body temperature measurement and preventive measures are not always carried out systematically and are not always implemented.
Nurse anaesthetists’ experience of how to prevent inadvertent hypothermia can provide more insight into what measures should be emphasised for day surgery patients. Together with other sources of knowledge, this experience must be applied in order to verify good practice. Such knowledge can indicate the need for training and the formulation of guidelines.
Objective of the study
The objective of the study was to acquire greater knowledge and understanding of how nurse anaesthetists in the day surgery unit prevent inadvertent perioperative hypothermia. The goal was to gain insight into the measures that should be implemented.
Method
Sample
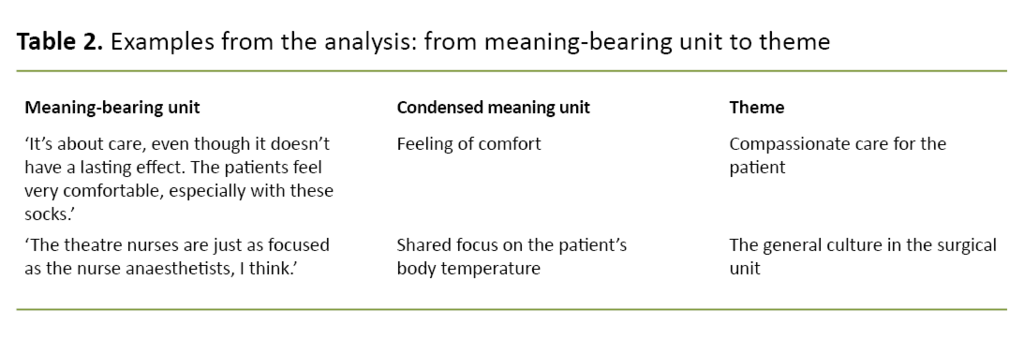
The study has a qualitative, descriptive design using focus group interviews as a method of exploring phenomena related to shared experiences and attitudes (19). We used a semi-structured interview guide (Table 1).
In order to gain experiences from both small and large hospitals, we conducted two focus group interviews at two different hospitals in western Norway in April and May 2018. We held two interviews in total, one at each hospital: there were six participants at hospital A and seven at hospital B.
We carried out a strategic selection to obtain the best possible variation in the sample so as to elucidate the research question. The inclusion criteria were as follows: nurse anaesthetists of different ages with experience of anaesthesia in relation to patients with different illnesses and of various ages, and employed in a day surgery unit at different hospitals.
Data collection
We devised the interview guide on the basis of our own experience and earlier research, and used it as support during the focus group interviews. First we carried out a pilot interview with three nurse anaesthetists to investigate whether the questions in the interview guide were comprehensible and relevant.
Together we decided to remove two of the questions that did not resonate with the field of practice. Moreover, we decided to simplify and shorten some of the questions. The second and third authors alternated between acting as moderator and assistant. The focus group interviews took place at the participants’ workplace during working hours, and lasted between 40 and 50 minutes.
Analysis
We transcribed the audio recordings immediately after the focus group interviews. The second and third author transcribed one interview each, anonymising the participants. Since all the authors are nurse anaesthetists, it was vital to be aware of our own preconceptions in order to avoid biased attitudes that might impact on the findings.
Two of the authors had long experience from the department of anaesthesia and the education of nurse anaesthetists. At one of the hospitals, the study included informants from the same workplace as the second and third authors.
The method of analysis was chosen on the basis of the type of question and data material as well as the possibility of compiling informants’ experiences in such a way that it would lead to new descriptions of the themes in the focus group discussions.
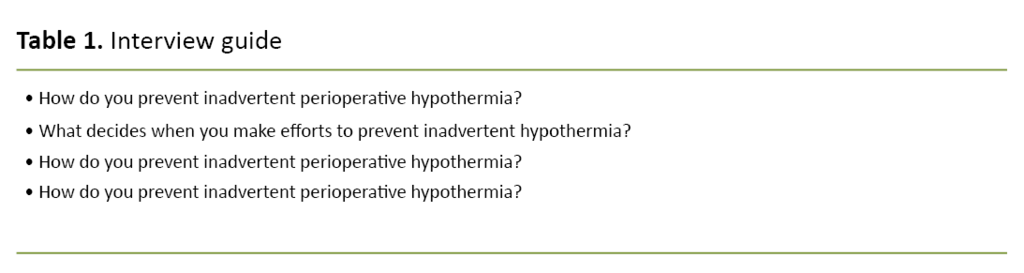
We used four-step, systematic text condensation (19). At step 1, we read through the material. This resulted in six preliminary themes that formed the basis of the analysis. At step 2, the themes formed the basis of the next step of the analysis, which entailed collating the parts of the text we wished to study in more detail.
We then formulated codes to sort the meaning-bearing units into code groups. Each code group was then divided into two to three sub-categories. While marking the meaning-bearing units, we started to systematise them. At step 3, we simplified the selected text from the second stage of analysis.
At the fourth and final step, all the selected parts of the text in the meaning-bearing units were recontextualised. See Example 1 in Table 2.
Ethics
The survey was carried out in line with the ethical guidelines of the Helsinki Declaration (18), and was assessed by the Norwegian Centre for Research Data (NSD) (project number 59291). The informants signed a consent form after receiving oral and written information about the study. Audio recordings and interview transcripts were stored in a research server.
Results
Description of the sample
The sample consisted of thirteen registered nurses (RNs): ten women and three men whose experience ranged from a few months to more than thirty years. There were six informants at hospital A: two men and four women with from one to thirty years’ experience of anaesthesia. At hospital B, there were seven informants: one man and six women whose experience ranged from a few months to twenty years.
The data analysis revealed four themes: ‘Insufficient standardisation of body temperature measurement methods and guidelines’, ‘Availability and resources’, ‘The general culture in the surgical unit’, and ‘Providing compassionate care to the patient’.
Insufficient standardisation of body temperature measurement methods and guidelines
Insufficient standardisation of body temperature measurement methods and guidelines was a theme that characterised both focus group interviews. The informants said that they measured body temperature during the perioperative period, but that routines and measurement methods varied.
Several of the participants at hospital B found it problematic that nasopharyngeal measurement could lead to bleeding in the nose and throat as well as causing bradycardia. The participants discussed the need for a common body temperature measurement method that was easy to use for both patients who are awake and patients under anaesthesia.
‘I think it’s difficult to find a reliable way of measuring body temperature where you can trust the temperature value. At least one that’s easy to use with all patients, whether they’re intubated or awake’ (hospital A).
Hospital B’s checklist did not contain a question on the measurement of body temperature.
The ‘Time-out’ and ‘Sign-out’ phases in the ‘Safe Surgery’ checklist were used at both hospitals. But there were differences in how hospitals A and B went through the checklist. The nurse anaesthetists at hospital A were reminded about body temperature measurement when the theatre nurses went through the obligatory questions in the ‘Safe Surgery’ checklist. Hospital B’s checklist did not contain a question on the measurement of body temperature:
‘It’s the theatre nurse who reads out the Time-out, and then they always read out, ‘Has the temperature been measured?’. They always ask about it, so it’s impossible to forget to measure the final intraoperative temperature at the end of surgery’ (hospital B).
‘You’ve got those who’ve become used to thinking a lot about body temperature because there’s been focus on that in the patient safety campaign related to ‘Safe Surgery’’(hospital A).
The nurse anaesthetists at hospital A had devised their own written guidelines for preventing inadvertent hypothermia. The informants at hospital B stated that they had no such guidelines and said that this could mean that different prevention measures were used. Some said that they felt there was a need for better justification of the actions they carried out so that they become more aware of which measures they should use to prevent hypothermia.
Availability and resources
The informants at both hospitals frequently brought up the topic of availability of equipment and resources in the unit. Several participants referred to resources such as time and financial aspects, but perceptions of these differed. The use of time in connection with preventive efforts was described in both a negative and positive manner:
‘So we always have that at the back of our minds, as least that’s what I notice. Yes, time is a resource, and we are more and more aware of that’ (hospital B).
No, we don’t have time to use Warm Touch. If we must use it, then we must, it’s the patient who decides, I suppose, and the operation’ (hospital A).
The participants at hospital A were positive to the unit’s prioritisation of financial aspects and heat-producing equipment.
Without exception, the participants at hospital A were positive to the unit’s prioritisation of financial aspects and heat-producing equipment, such as expensive, single use, self-warming blankets:
‘I have the impression that the EasyWarm blankets are very popular and are used a lot. We get new deliveries constantly, so there’s quite a big turnover’ (hospital A).
Nurse anaesthetists in both focus group interviews said that they had good access to the equipment available in the unit – heat-producing equipment such as Warm Touch was frequently used. However, factors such as noise and heat in the operating area could put a stop to using Warm Touch at hospital B. Sometimes financial aspects were mentioned as an obstacle to carrying out preventive efforts to combat hypothermia at hospital B:
‘It’s supposed to be effective, and fast. The idea is probably to use the least amount of money on equipment in the process [...] It’s all related to financial aspects’ (hospital B).
The general culture in the surgical unit
The participants in both focus group interviews described cooperation as generally good. The surgical team were keen to prevent inadvertent hypothermia, and focus was on the patient. However, it was revealed that it was mainly the theatre nurses and nurse anaesthetists that took responsibility when it came to warming measures and prevention of inadvertent hypothermia:
‘The theatre nurses are just as focused as the nurse anaesthetists, I think’ (hospital A).
The nurse anaesthetists at both hospitals said that there was an established culture where the surgical team sometimes had different requirements as to the desired temperature in the operating theatre:
‘There’s a well-established tradition in the operating theatre that consideration for the surgeon must be kept in mind. So that’s crucial’ (hospital B).
Providing compassionate care to the patients
The nurse anaesthetists at both hospitals described how they prevented inadvertent hypothermia by covering the head, for example, or warming intravenous fluid and heating blankets and socks. The informants at hospital A said that the patients really appreciated heated blankets and socks: ‘Oh, that’s lovely.’ The participants at hospital B said they had had to struggle to retain such measures, which they described as compassionate care:
‘It’s about care, even though it doesn’t have a lasting effect. The patients feel very comfortable, especially with these socks. Some people felt that the socks weren’t necessary when we moved to the new unit. But we managed to keep them by whinging about it (hospital B).
The participants at hospital B stated that they provided compassionate care to the surgical patient from the very start of the preoperative stage. The informants said that it was important to prevent hypothermia by giving patients a warming blanket while they waited to be taken into the cold operating theatre:
‘Sometimes the patients are given a blanket preoperatively to cover themselves while they’re waiting. Some RNs are good at this, others not so good [...] So I think this is an area we can really improve’ (hospital B).
Discussion
The objective of the study was to obtain more knowledge and understanding of how nurse anaesthetists in day surgery units prevent inadvertent perioperative hypothermia.
We found that the participants in both hospitals sought a reliable way of measuring body temperature – a temperature you could rely on regardless of whether the patient was awake or under anaesthesia. Bindu et al. (5) point out that body temperature measurement is the least objective intraoperative parameter.
Our findings showed that the body temperature measurement method was often a contributory cause of failure to measure body temperature. This is in line with Loe and Moe’s findings that temperature measurement pre-, intra- and post-operatively does not appear to be a fixed routine but dependent on good teamwork and communication, the personnel’s clinical assessment, the patient’s condition and organisational parameters (17).
At its most extreme, inadvertent hypothermia may lead to a longer period of hospitalisation for the patient and increased risk of mortality (4, 5, 8, 9, 18). Clinical guidelines recommend the implementation of heat-producing measures in order to prevent inadvertent hypothermia. In the case of general anaesthesia lasting more than 30 minutes, core body temperature should be measured (8, 9, 11).
There is insufficient standardisation in relation to how the guidelines are applied
Written guidelines for the prevention of inadvertent hypothermia had been devised at hospital A, but at the same time, our informants asserted that there was insufficient standardisation in how they were practised. The Norwegian standard for the safe practice of anaesthesia (15) and Basic guidelines for nurse anaesthetists (16) address body temperature as an important element in the monitoring of anaesthesia, and describe the importance of using adequate methods to measure body temperature. However, these documents do not discuss methods of measurement, the temperature measurement site or when measures should be implemented.
Research shows that core temperature should be measured at sites where there is good circulation and high comparability with the rest of the body (5, 9). Nurse anaesthetists are dependent on the unit’s resources and guidelines (15, 16) as well as on their own knowledge, routines for measuring patients’ temperature and further monitoring of temperature.
The ‘Safe Surgery’ checklist was practised differently
The ‘Safe Surgery’ checklist was used at both hospitals but there were different practices in relation to body temperature measurement. The checklist was intended to ensure that measures to prevent inadvertent hypothermia were implemented (14).
The ‘Safe Surgery’ checklist was used at both hospitals but there were different practices in relation to body temperature measurement.
Haugen et al. (20, 21) point out that the implementation of the ‘Safe Surgery’ checklist has led to mostly positive results, ensuring improved patient safety. For example, the prevention of inadvertent perioperative hypothermia leads to fewer cases of postoperative surgical site infections, fewer blood transfusions, reduced administration of antibiotics and better cardiac and pulmonary function.
Differences in financial aspects
The findings in our study showed that there were differences in how the informants referred to resources such as time and financial aspects. Some participants described this more positively and were unaffected by the pressure of time and the focus on financial aspects as opposed to other participants who said that these could be an obstacle to efforts to prevent hypothermia.
According to Naalsund and Steen-Hansen (13), day surgery is seen as a cost-effective process. Day surgery is profitable from a socio-economic perspective and will free-up beds for other patient groups (13). Emberland (22) outlines an ever-growing focus on cost effectiveness and financial factors, meaning more and more complex operations will be conducted as day surgery.
The general culture affected the use of warming measures
Our findings showed that the general culture played a role in the implementation of warming measures. The participants described the excellent cooperation between nurse anaesthetists and theatre nurses in the prevention of inadvertent hypothermia. According to Eide (23), this is an interdisciplinary task requiring the cooperation of the surgical team.
Nightingale (24) highlights the fact that taking responsibility is not just a matter of taking the right precautions yourself but also ensuring that everyone else takes responsibility. Moreover, we found that consideration for individual needs in the surgical team appeared to outweigh the patient’s needs.
In both hospitals, hypothermia is prevented through actions the informants describe as providing compassionate care to the patients.
Leonardsen describes how different individuals in a surgical team experience interdisciplinary cooperation in the team. He outlines a hierarchical system in which there may be conflicts of interest (25).
In both hospitals, hypothermia is prevented through actions the informants describe as providing compassionate care to the patients. According to Martinsen, care can also be demonstrated through practical actions (26). The warm socks and blankets may serve to illustrate the care the RNs provide to patients, and this can be seen in the light of our work ethics.
The guidelines for nurse anaesthetists state that the surgical team must make every effort to ensure the best possible patient care (16). Nortvedt highlights the importance of a health service where the patient is seen and heard (27).
Methodological considerations
The choice of focus group interviews is a strength of the study. Experiences and opinions that the informants shared in the group discussion promoted new reflections and thoughts. We noted many good descriptions of themes that may be relevant for increasing awareness about the prevention of inadvertent perioperative hypothermia in day surgery patients.
According to Malterud (19), experience, knowledge and familiarity with the context is an advantage in qualitative research. However, our preconceptions as nurse anaesthetists and the conduct of research in our own workplace may have resulted in biased attitudes that may have impacted on the findings.
We were aware of these factors and sought to ensure that our own knowledge, experiences and perceptions had minimal influence. The interview guide was trialled in a pilot interview. We planned to hold three focus group interviews across three hospitals, but for practical reasons, we recruited informants for two focus group interviews at two hospitals.
The sample was therefore smaller than planned. To achieve data saturation, more focus group interviews might have provided richer data. A more even gender distribution might have been advantageous in terms of sample variation (19), but at the same time the aim of a homogeneous sample must be balanced against variation in the sample. It is the diversity of experience that creates nuances in the data.
The study might have been strengthened if the theatre nurses had been included, since the prevention of inadvertent perioperative hypothermia is the shared responsibility of the surgical team. However, in this study we wished to focus attention on nurse anaesthetists’ experience of preventing inadvertent hypothermia, since research on this topic is scarce.
Conclusion
There was insufficient standardisation in the prevention of inadvertent perioperative hypothermia in day surgery patients, which may indicate that body temperature measurement and routines should be more consistently monitored. Moreover, provision should be made to ensure a practice where staff have the equipment and available time to prevent inadvertent hypothermia.
Providing information on the guidelines and teaching staff in day surgery units about inadvertent hypothermia are also helpful. A question on body temperature measurement should be included in the ‘Safe Surgery’ checklist at all hospitals.
It would be interesting to map interdisciplinary cooperation and the use of checklists in a more comprehensive study, and to interview all professionals represented in the surgical team.
References
1. Shaw CA, Steelman VM, DeBerg J, Schweizer ML. Effectiveness of active and passive warming for the prevention of inadvertent hypothermia in patients receiving neuraxial anesthesia: a systematic review and meta-analysis of randomized controlled trials. J Clin Anesth. 2017;38:93–104. DOI: 10.1016/j.jclinane.2017.01.005
2. Liu S, Pan Y, Zhao Q, Feng W, Han H, Pan Z, et al. The effectiveness of air-free warming systems on perioperative hypothermia in total hip and knee arthroplasty: a systematic review and meta-analysis. Medicine (Baltimore). 2019;98(19):e15630. DOI: 10.1097/MD.0000000000015630
3. Matilda E, Westergaard-Nielsen E, Henricson M. Preoperative peripheral and core temperature: an observational study at a day-surgery unit. Br J Nurs. 2020;29(3):160–4. DOI: 10.12968/bjon.2020.29.3.160
4. Giuliano KK, Hendricks J. Inadvertent perioperative hypothermia: current nursing knowledge. AORN J. 2017;105(5):453–63. DOI: 10.1016/j.aorn.2017.03.003
5. Bindu B, Bindra A, Rath G. Temperature management under general anesthesia: compulsion or option. J Anaesthesiol Clin Pharmacol. 2017;33(3):306-16. DOI: 10.4103/joacp.JOACP_334_16
6. Sagiroglu G, Ozturk GA, Baysal A, Turan FN. Inadvertent perioperative hypothermia and important risk factors during major abdominal surgeries. J Coll Physicians Surg Pak. 2020;30(2):123–8. DOI: 10.29271/jcpsp.2020.02.123
7. NICE, National Institute for Health and Care Excellence. Hypothermia: prevention and management in adults having surgery [published 23.04.2008, updated 14.12.2016, cited 23.03.2018]. NICE; 2008. Available at: https://www.nice.org.uk/guidance/cg65
8. Sessler DI. Perioperative thermoregulation and heat balance. Lancet. 2016;387(10038):2655–64. DOI: 10.1016/S0140-6736(15)00981-2
9. Sessler D. Perioperative temperature management. I: Post TW, red. UpToDate. Waltham, MA: UpToDate. Available at: https://www.uptodate.com/contents/perioperative-temperature-management (downloaded 28.09.2019).
10. Berg T, Hagen O. Forebygging og behandling av anestesirelaterte komplikasjoner. In: Dåvøy GAM, Eide PH, Hansen I, eds. Operasjonssykepleie. 2nd ed. Oslo: Gyldendal Akademisk; 2018. pp. 280–1.
11. Broback BE, Skutle GØ, Dysvik E, Eskeland A. Preoperativ oppvarming med varmluftsteppe forebygger hypotermi under operasjon. Sykepleien Forskning. 2018;13(65819):e-65819. DOI: 10.4220/Sykepleienf.2018.65819
12. Helsedirektoratet. Samdata spesialisthelsetjenesten 2015. Oslo: Helsedirektoratet; 2016. IS-2485. Available at: https://www.helsedirektoratet.no/rapporter/samdata-spesialisthelsetjenesten/Samdata%20Spesialisthelsetjenesten%202015.pdf (downloaded 04.03.2018).
13. Naalsund U, Steen-Hansen E. Dagkirurgiske pasienter. In: Dåvøy GAM, Eide PH, Hansen I, eds. Operasjonssykepleie. 2nd ed. Oslo: Gyldendal Akademisk; 2018. pp. 449–62.
14. Pasientsikkerhetsprogrammet. Trygg kirurgi. Oslo: Helsedirektoratet; 2014. Available at: https://pasientsikkerhetsprogrammet.no/om-oss/innsatsomrader/trygg-kirurgi (downloaded 26.03.2021).
15. Anestesisykepleierne NSF. Norsk standard for anestesi. Oslo: Anestesisykepleierne NSF; 2016. Available at: https://www.alnsf.no/anestesisykepleierne/norsk-standard-for-anestesi (downloaded 20.03.2018).
16. International Federation of Nurse A. Grunnlagsdokument for anestesisykepleiere. Oslo: Anestesisykepleierne NSF; 2016.
17. Loe SAK, Mo BE. Forebygging og behandling av utilsiktet peroperativ hypotermi hos operasjonspasienten: en kvalitativ studie av anestesi- og operasjonssykepleieres erfaringer. Gjøvik: Høgskolen i Gjøvik; 2010.
18. Honkavuo L, Loe SAK. Nurse anesthetists' and operating theater nurses' experiences with inadvertent hypothermia in clinical perioperative nursing care. J Perianesth Nurs. 2020;35(6):676–81. DOI: 10.1016/j.jopan.2020.03.011
19. Malterud K. Kvalitative forskningsmetoder for medisin og helsefag. 4th ed. Oslo: Universitetsforlaget; 2017.
20. Haugen AS, Sevdalis N, Søfteli. Impact of the World Health Organization surgical safety checklist on patient safety. Anesthesiology. 2019;131(2):420–5. DOI: 10.1097/aln.0000000000002674
21. Haugen AS, Waehle HV, Almeland SK, Harthug S, Sevdalis N, Eide GE, et al. Causal analysis of World Health Organization's surgical safety checklist implementation quality and impact on care processes and patient outcomes: secondary analysis from a large stepped wedge cluster randomized controlled trial in Norway. Ann Surg. 2019;269(2):283–90. DOI: 10.1097/SLA.0000000000002584
22. Emberland I. Anestesisykepleierens ivaretakelse av operasjonspasienten i det korte møtet: Vurdering av muligheter, handling og begrunnelse [Master's Thesis]. Tromsø: Det helsevitenskapelige fakultet, Institutt for helse- og omsorgsfag, UiT Norges arktiske universitet; 2017. Available at: https://munin.uit.no/handle/10037/12733 (downloaded 26.03.2021).
23. Eide PH. Forebygging av hypotermi. In: Dåvøy GAM, Eide PH, Hansen I, eds. Operasjonssykepleie. 2nd ed. Oslo: Gyldendal Akademisk; 2018. pp. 307–19.
24. Nightingale F. Notater om sykepleie. 2nd ed. Oslo: Universitetsforlaget; 1997.
25. Leonardsen A-CL. Tverrfaglig samarbeid i operasjonsteamet. Nordisk sygeplejeforskning. 2015;5(2):218–27.
26. Martinsen K. Omsorg, sykepleie og medisin: historisk-filosofiske essays. Oslo: Tano; 1989.
27. Nortvedt P. Er omsorg realistisk? Sykepleien. 2014;102(5):66–7. Tilgjengelig fra: https://sykepleien.no/etikk/2014/04/er-omsorg-realistisk (downloaded 12.03.2021).










Comments