Hypothermia in surgical patients on admission to a postoperative ICU
Too many patients had hypothermia both on admission, and one hour after admission, to a postoperative intensive care unit. Elderly patients and those who had undergone laparoscopic surgery were particularly at risk.
Background: Inadvertent hypothermia in surgical patients may result in adverse outcomes such as a greater risk of bleeding and infection. In recent decades, a variety of interventions have been introduced to reduce heat loss in patients before, during and after surgery. However, practices can vary, and patients can still be susceptible to developing hypothermia.
Objective: The purpose of this study was to estimate the incidence of hypothermia in elective surgery patients who had undergone abdominal surgery or thoracic surgery while under general anaesthesia and to investigate whether the type and length of surgery and the patient’s medical condition, age and gender were associated with hypothermia.
Method: This was a prospective observational study conducted at a Norwegian university hospital. One hundred patients had their ear temperature (Tp) measured at three points in time: before surgery, on admission to the postoperative ICU, and one hour after admission to the postoperative ICU. Data were collected in the period from December 2017 to January 2018, and analysed using descriptive statistics and regression analysis.
Results: Twenty-four per cent of the patients in the study were hypothermic (Tp < 36.0 °C) on admission to the postoperative intensive care unit (ICU), and 13 per cent were hypothermic one hour after admission to the same unit. The regression analysis indicated that elderly patients (p = 0.008) and those who had undergone laparoscopic surgery (p = 0.018) had significantly higher odds of having a lower body temperature on admission to the postoperative ICU.
Conclusion: The incidence of hypothermia insurgical patients admitted to the postoperative ICU is still too high. Elderly patients and those who had undergone laparoscopic surgery were particularly susceptible to having a lower body temperature. These results should lead to more systematic temperature measurement and better warming strategies for surgical patients in the anaesthesia, surgical and postoperative wards.
Maintaining a patient’s normal body temperature in the pre-, peri- and postoperative periods is essential for patient safety, the expected surgical outcome and patient satisfaction (1, 2).
The risk of hypothermia is particularly high in patients over 60 years of age with poor nutritional status and pre-existing disease that impairs thermoregulation (3).
Inadvertent hypothermia in surgical patients may prolong the effect of general anaesthesia, reduce the immune defence leading to a higher incidence of wound infections, impair wound healing, and increase the incidence of bleeding. These complications may result in a need for blood transfusion, prolonged mechanical ventilation, and increased circulatory support (2, 4).
Surgical patients are often susceptible to heat loss due to disrobing, cool operating theatre temperatures, general anaesthesia, lengthy surgical procedures, laparotomy, and insufflation of cold, dry CO2 gas during laparoscopy (5–8).
Laparotomy is an open surgical procedure in which a large incision is made in the abdominal cavity, while in laparoscopy an endoscope is inserted via a small incision, known as keyhole surgery (5–8).
Serious complications can arise from even mild hypothermia, defined as a core temperature of 35.0–36.0 °C (2, 9). It is therefore crucial to systematically measure and document the patient’s temperature in order to quickly identify and treat hypothermia (3).
In recent decades, a variety of interventions, such as adequate covering, warm intravenous and irrigation fluids, and warmed sheets and forced-air warming blankets, have been introduced to reduce heat loss in patients before, during and after surgery (10–13). Nevertheless, studies show that the incidence of hypothermia in patients admitted to the postoperative ICU is high (17–46 per cent) (14, 15).
The first postoperative period is precarious
While anaesthetic nurses and surgical nurses are responsible for preventing hypothermia in patients before and during an operation, intensive care nurses have a special responsibility for the patient’s temperature on admission to the postoperative intensive care unit (ICU). If a patient’s core temperature drops, the risk of complications and additional post-surgical difficulties increases in an already vulnerable patient.
Intensive care nurses have a special responsibility for the patient’s temperature on admission to the postoperative intensive care unit.
The first postoperative period is the most precarious for patients. It is therefore essential that surgical, anaesthetic and intensive care nurses observe and register the patient’s vital signs to prevent and treat complications that may develop (3, 12).
International guidelines on hypothermia recommend using warming interventions for all surgical patients and measuring the patient’s temperature continually or every 15 minutes during the pre- and postoperative periods.
If a patient is hypothermic on admission to the postoperative ICU, additional warming interventions must be commenced and the patient’s temperature must be measured every 15 minutes until a normal body temperature is reached (3, 16).
Nurses unfamiliar with hypothermia guidelines
The guidelines, however, may be difficult to implement. In several studies, the nurses were shown to be unfamiliar with the guidelines and to have limited knowledge about hypothermia (17, 18).
While nurses may well know that laparotomy and prolonged surgery cause heat loss, and take measures to keep their patients warm, they may not be as aware of heat loss caused by other procedures such as minor surgeries and laparoscopy (19).
Objective of the study
As a consequence, the effectiveness of nursing routines for temperature control and strategies for preventing hypothermia in various surgical patients may vary.
We therefore wanted to investigate whether patients were hypothermic on admission to and during their stay in the postoperative ICU, and explore whether various factors were associated with hypothermia.
The objective of the study was two-fold:
- Estimate the incidence of hypothermia in elective surgery patients who had undergone abdominal surgery or thoracic surgery while under general anaesthesia, and
- Investigate whether the type and length of surgery and the patient’s medical condition, age and gender were associated with hypothermia.
Method
Design
We conducted a prospective observational study in which we collected data from the anaesthesia ward and the postoperative ICU of a large Norwegian hospital.
Participants
We invited patients to take part in the study on random days during a two-month period. The inclusion and exclusion criteria were as follows:
Inclusion criteria:
- age > 18 years
- planned surgery of the abdomen or thorax
- use of general anaesthesia, with or without epidural anaesthesia
Exclusion criteria:
- patients with a temperature over 37.5 °C as the baseline before surgery
- emergency patients
- patients found to be mentally unclear and disoriented or who did not speak Norwegian or English
- patients who had to deviate from the planned operation for one reason or another
- gynaecological surgery and women with a confirmed pregnancy
Data collection
Data were collected in the period from December 2017 to January 2018. All the patients invited to take part in the study agreed to do so. We registered their temperatures with an infrared ear thermometer at three different points in time: 1) before surgery, 2) on admission to the postoperative ICU, and 3) one hour after admission to the postoperative ICU.
The surgery schedule with an overview of the operation’s length and time of transfer to the postoperative ICU was used to ensure that we collected the data at the correct points in time.
Tympanic temperature measurement
Tympanic temperature measurement is carried out with an infrared ear thermometer that measures a patient’s core temperature by measuring the temperature of the blood in the arterial blood supply which passes through the hypothalamus and the tympanic membrane in the auditory canal (20).
Studies show that measuring ear temperature with an aural probe is a reliable method of charting body temperature and advantageous in terms of speed and ease of use (15, 20). The infrared tympanic membrane thermometer used in this study was made by Braun.
The thermometer was labelled in advance so that we could use the same thermometer on all the patients. The first, second and third authors jointly reviewed the instructions for use and the procedure for measuring ear temperature before starting the work to ensure a reliable registration of patients’ temperatures.
Two of the above-mentioned authors were always present during the data collection process. All three authors worked on the data collection for the same number of days.
Two of the authors measured the patient’s temperature twice in the same ear to rule out errors in measurement. We took the temperature from the patient’s right ear unless the patient had visible earwax or the ear had recently been covered.
We wrote down the temperature on two different forms before comparing them. If the temperatures differed by several decimals or fell outside the normal reference area, we performed a new measurement.
The highest registered temperature was used in the data analysis. The highest temperature is probably more representative of the patient’s core temperature since the thermometer has been in the ear canal longer and has therefore come into better contact with the tympanic membrane (12). We analysed the temperature as a continuous variable.
Independent variables
We registered clinical variables from the patients’ surgical and anaesthesiology records following surgery. These variables included type of surgery (laparoscopy/laparotomy), age, gender, ASA classification and length of surgery. We did not register the specific surgical procedure that an individual patient underwent or the warming methods used before, during and after surgery.
The length of surgery was dichotomised to less than two hours versus more than two hours. We set this limit on the basis of a meta-analysis showing that an operation lasting more than two hours doubles the risk of complications (21). The type of surgery was categorised as either laparoscopic or laparotomic.
The American Society of Anesthesiologists (ASA) Physical Status Classification System is a scale used to assess the patient’s risk factors in connection with anaesthesia. The ASA classification ranges from levels I to V. ASA I denotes a normal healthy patient, while ASA V indicates a moribund patient who is not expected to survive without the operation (22).
Analysis
When the data collection was complete, data were analysed using the Statistical Package for the Social Sciences (SPSS), version 19.0.
The statistical analysis included descriptive statistics (average, standard deviation [SD], percentages, box diagram), a graphic representation (box plot), and single and multiple linear regression analysis.
Multiple linear regression analysis was performed to test the association between the various independent variables and the dependent variable of hypothermia. The selected significance level was a p-value < 0.05.
Ethical considerations
The hospital’s Data Protection Officer approved the study as a quality enhancement project. Prior to start-up, we provided verbal information about the study to all the patients in the study, and all of them voluntarily signed a form of consent to participate.
After their surgery, patients received written information about the study, which also gave them the opportunity to withdraw from the study if they wished.
We stored the consent forms and the numbered temperature forms with variables in two separate locked drawers. All the forms were destroyed after the data analysis was completed.
Results
Most of the patients included in the study had undergone surgery related to lung cancer, aorta aneurysm, gall stones, kidney cancer, colostomy, ileostomy or bariatric surgery.
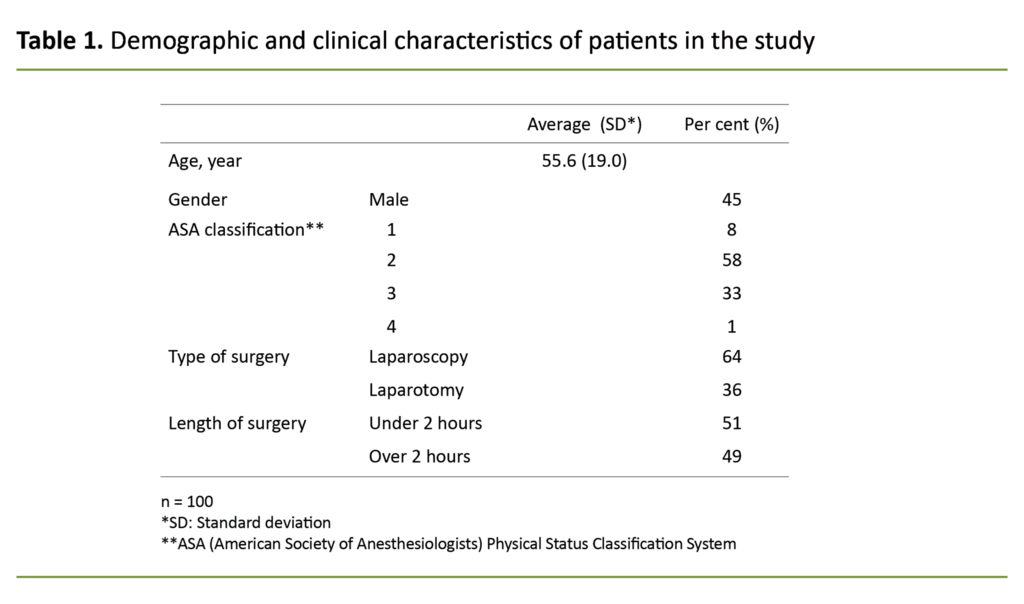
We included 100 patients in the study. Of those, 45 were men and 55 women. Their ages ranged from 19 to 93 years, with an average age of 56 years (SD = 19) (Table 1). All the patients lay in bed while awaiting surgery.
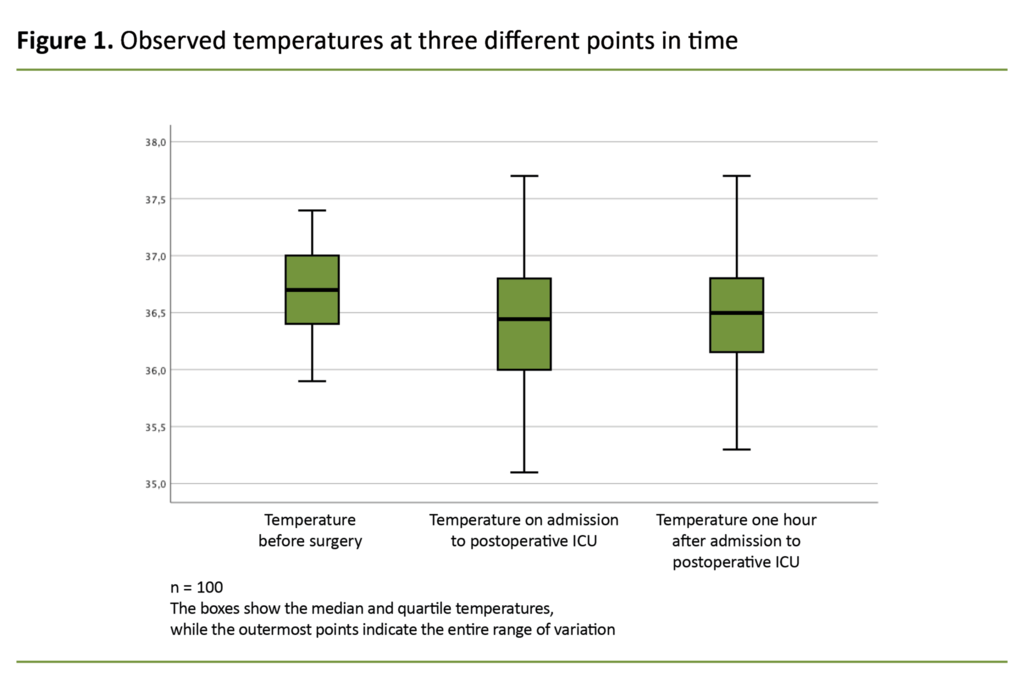
Figure 1 shows a box diagram of the median temperature and quartiles for the three points in time when temperatures were taken. The lowest registered temperature of 35.1 °C was measured on admission to the postoperative ICU.
The median temperature for all three points in time was within normal body temperature: 36.7 °C before surgery, 36.4 °C on admission to the postoperative ICU, and 36.5 °C one hour after admission to the postoperative ICU.
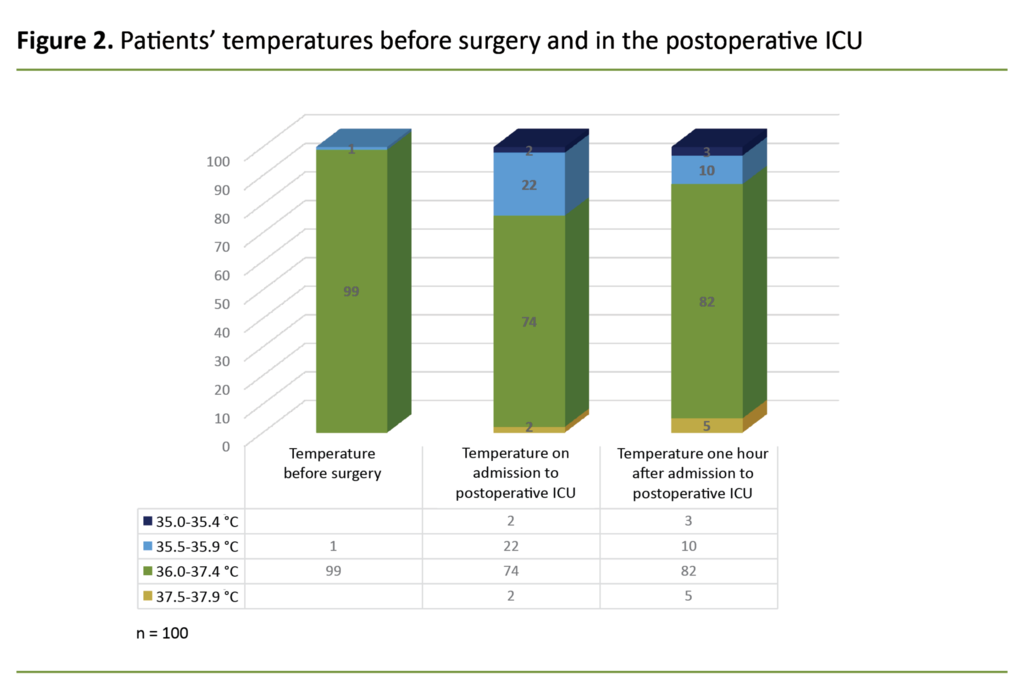
Figure 2 presents data in a histogram with three bars representing the three different points in time when temperatures were measured. Of the 100 patients, 37 were registered as being hypothermic at one or both points in time while in the postoperative ICU.
Twenty-four per cent of the patients were hypothermic on admission to the postoperative ICU, while 13 per cent were hypothermic one hour after admission.
Twenty-four per cent of the patients were hypothermic on admission to the postoperative ICU.
Two patients had a temperature less than 35.4 °C on admission to the postoperative ICU, and this rose to three patients one hour after admission to the postoperative ICU.
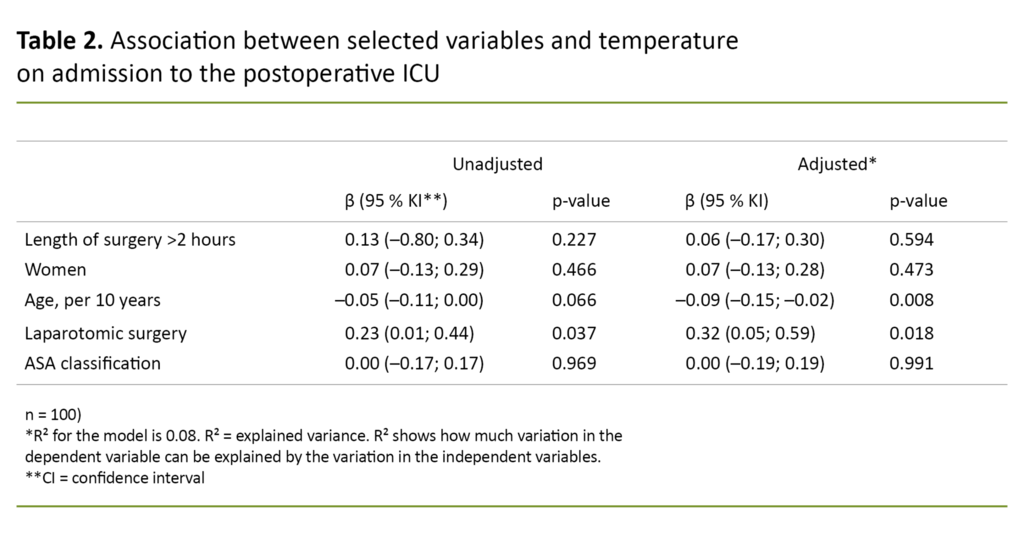
The results from the multiple linear regression analysis show that type of surgery and age have a statistically significant association with body temperature on admission to the postoperative ICU. The findings indicate that the expected core temperature declines by 0.1 °C for every ten-year increase in a patient’s age.
Patients who underwent laparoscopic surgery had an average temperature 0.32 °C lower than patients who did not have this type of surgery.
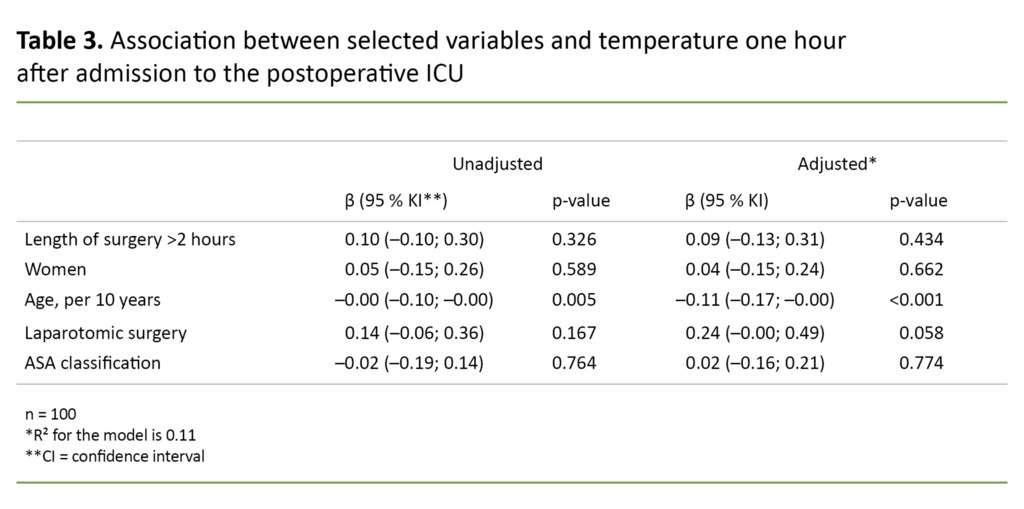
In Table 3, the regression analysis shows that only an elderly age has a statistically significant association with temperature one hour after admission to the postoperative ICU.
The independent variables may explain the temperature on admission to the postoperative ICU by 8 per cent (Table 2) and one hour after admission by 11 per cent (Table 3).
Both regression analyses show that length of surgery, ASA classification and gender are not associated with hypothermia in patients in the postoperative ICU.
Discussion
The purpose of this study was to estimate the incidence of hypothermia in patients in the postoperative ICU. We also wanted to investigate which groups of surgical patients were the most susceptible to developing hypothermia.
The findings indicate that the incidence of hypothermia in patients on admission to the postoperative ICU was high (24 per cent). The groups susceptible to low body temperature were elderly patients and patients who had undergone laparoscopic surgery.
Maintaining the patient’s temperature during surgery
The proportion of postoperative hypothermia (24 per cent) in patients in this study may suggest that not all patients were sufficiently warmed during the pre- and perioperative periods. This figure is high compared with a recent, large German study that shows an incidence of postoperative hypothermia of 8.3 per cent (23).
Our findings are nonetheless comparable to findings from other studies showing that the incidence of postoperative hypothermia in patients ranges from 17 to 46 per cent (14, 15, 24). All these studies used an infrared tympanic membrane thermometer for registering patients’ temperatures.
Due to the high incidence of peri- and postoperative hypothermia, new guidelines on preoperative warming of all surgical patients have been introduced (3). One study has shown that only ten minutes of preoperative warming may be effective in maintaining a patient’s normal body temperature during surgery (25).
Our study found no association between individual, well-known risk factors for developing hypothermia, such as prolonged surgery, laparotomic procedures and higher ASA classification (7, 26). This finding may suggest that groups of patients have received good, effective warming treatment.
Inadequate care for elderly patients
The study indicated, however, that elderly patients received inadequate care for hypothermia, as we found an association between a patient’s elderly age and lower body temperature. Elderly patients are predisposed to hypothermia due to impaired thermoregulation, which is caused by reduced muscle mass and changes in metabolism (27).
The study also showed an association between laparoscopic surgery and lower body temperature. This may indicate that not enough warming interventions were used on these patients or that the measures taken were not effective enough.
The study indicated that elderly patients received inadequate care for hypothermia.
In laparoscopic surgery, cold, dry CO2 gas is insufflated into the abdominal cavity, resulting in heat loss and the risk of developing hypothermia (8).
The surgical team may not always be aware of this. Laparoscopy is performed during both major and minor surgical procedures. In one study, surgical, anaesthesia and intensive care nurses ranked minor surgery as having the lowest risk factor for patients developing hypothermia (18, 19).
Warming strategies needed for all surgical patients
A recent randomised control trial showed that the use of forced-air warming blankets is significantly more effective in preventing hypothermia during laparoscopy than passive warming strategies when the procedure lasts more than one hour (28).
Guidelines and procedures for preventing hypothermia related to various types of surgery were introduced in the surgical and anaesthesia wards in question. Unfortunately, we did not register which warming methods were used for the patients in this study.
According to the guidelines on preventing inadvertent hypothermia, all surgical patients must be warmed, preferably with forced-air warming blankets (3, 16, 29).
Guidelines from the National Institute for Health and Clinical Excellences (NICE) recommend using a forced-air warming device for all surgical patients who will be anaesthetised for more than 30 minutes and/or who have a temperature below 36 °C when they are ready to be transferred to the postoperative ICU (9).
Maintaining the patient’s temperature during a stay in the postoperative ICU
Two of the patients in the study had a temperature below 35.4 °C on admission to the postoperative ICU. One hour after admission, 13 per cent of the patients still had hypothermia, while the number of patients with a temperature below 35.4 °C had risen to three.
One hour after admission, 13 per cent of the patients still had hypothermia.
We know that guidelines for systematic temperature control and warming interventions for hypothermic patients had not been introduced in the postoperative ICU in our study at the time of temperature registration. According to the guidelines, the patient’s temperature must be measured immediately after admission to the postoperative ICU.
The aim is to minimise heat loss from the skin and vulnerable areas, cooling caused by the infusion of cold fluids, or the use of cold gasses to aid in respiration. Patients who are hypothermic must be warmed until they reach a normal body temperature (11, 16).
Nurses were not told about hypothermic patients
Although interventions for warming patients with inadvertent postoperative hypothermia are the same as for pre- and perioperative hypothermia, the basis for these interventions is completely different for patients who are conscious.
Treating hypothermia in the postoperative ICU is complex, as the patient’s pain, nausea and shivering are all associated with lower body temperature. When hypothermia occurs, it is essential that interventions to try to warm up the patient are initiated as quickly as possible to minimise potential complications.
Most patients are conscious immediately following surgery, and it is important that each and every measure is well tolerated and effective (11, 16).
We found it to be ethically challenging to withhold information about hypothermia in patients from the nurses with responsibility for those patients. In only one case did we report a patient’s temperature to the relevant intensive care nurse in the postoperative ICU at the start of the data collection process.
This case concerned a patient with a temperature of 35.1°C one hour after admission to the postoperative ICU. Due to the patient’s low temperature and clinical condition, we decided that the intensive care nurse should be informed of her patient’s temperature.
Strengths and weaknesses of the study
A strength of this study is that infrared tympanic temperature measurement was frequently used in comparable studies (7, 14, 15, 24), making it possible to compare the results.
The study has several weaknesses. First, infrared tympanic temperature measurement is not as reliable as measuring temperature with a pulmonary artery catheter, which is a highly reliable measurement of a patient’s core temperature (30).
One study has shown that a tympanic membrane thermometer registers a temperature 0.1–0.4 per cent lower than a pulmonary artery catheter (30). Thus, the incidence of hypothermia in our study may be overestimated.
However, even if 0.5 degrees were added to the measured tympanic temperature, there would still be an incidence of hypothermia in the patients in this study.
To enhance the reliability of our measurements, two authors, rather than one, collected the data. We wrote down the temperatures taken on different forms before comparing the numbers. In addition, we used the highest registered temperature to ensure that the temperature measurement was reliable.
Secondly, it was difficult to be an ‘anonymous’ observer. The fact that we were visible during the data collection should be taken into account when interpreting the findings. Thirdly, the population is small, and the data are collected from one hospital. This decreases the generalisability of the results.
A final weakness of the study is that the explained variance among the variables in Tables 2 and 3 was 8 and 11 per cent. This variance is relatively small. Other variables not included in this study may have a more significant association with hypothermia.
Other potential variables may be height, weight, specific diagnosis or procedure, insufficient warming interventions or the type of warming interventions used before, during and after surgery. The fact that these variables were not registered weakens the validity of this study.
Conclusion
This study shows a high incidence of hypothermic patients, both on admission to the postoperative ICU and one hour after admission to the postoperative ICU at a Norwegian hospital. Elderly patients and patients who had undergone laparoscopic surgery were the two groups most susceptible to having a low body temperature.
The results should lead to more systematic temperature measurement and better warming strategies for surgical patients, on both the anaesthesia and the surgical wards.
To ensure a good patient trajectory in the postoperative ICU, systematic temperature control should be introduced as routine on a par with the measurement of other vital signs so that hypothermic patients are identified at an early stage and are sufficiently warmed, thereby avoiding complications from hypothermia.
We wish to express our gratitude to the patients who took part in this study. Many thanks to Gunhild Bakkalia Bjørnå, a professional development nurse who helped to guide and adapt this study. Thanks also to the personnel of the anaesthesia, surgical and postoperative wards where this study was carried out.
References
1. Wagner VD. Patient safety chiller: unplanned perioperative hypothermia. AORN J. 2010;92(5):567–71.
2. Leeth D, Mamaril M, Oman KS, Krumbach B. Normothermia and patient comfort: a comparative study in an outpatient surgery setting. J Perianesth Nurs. 2010;25(3):146–51.
3. Torossian A, Brauer A, Hocker J, Bein B, Wulf H, Horn EP. Preventing inadvertent perioperative hypothermia. Dtsch Arztebl Int. 2015;112(10):166–72.
4. Akers JL, Dupnick AC, Hillman EL, Bauer AG, Kinker LM, Wonder AH. Inadvertent perioperative hypothermia risks and postoperative complications: a retrospective study. AORN J. 2019;109(6):741–7.
5. Miyazaki R, Hoka S. What is the predictor of the intraoperative body temperature in abdominal surgery? J Anesth. 2019;33(1):67–73.
6. Lenhardt R. Body temperature regulation and anesthesia. Handb Clin Neurol. 2018;157:635–44.
7. de Brito Poveda V, Galvao CM, dos Santos CB. Factors associated to the development of hypothermia in the intraoperative period. Rev Lat Am Enfermagem. 2009;17(2):228–33.
8. Jacobs VR, Morrison JE jr., Mettler L, Mundhenke C, Jonat W. Measurement of CO(2) hypothermia during laparoscopy and pelviscopy: how cold it gets and how to prevent it. The Journal of the American Association of Gynecologic Laparoscopists. 1999;6(3):289–95.
9. National Institute for Health and Clinical Excellence. Clinical practice guideline. The management of inadvertent perioperative hypothermia in adults. London: National Institute for Health and Clinical Excellence; 2007. Available at: https://www.nice.org.uk/guidance/cg65/update/CG65/documents/perioperative-hypothermia-inadvertent-guideline-guideline-for-consultation2 (downloaded 14.01.2020).
10. AORN Recommended Practices Committee. Recommended practices for the prevention of unplanned perioperative hypothermia. AORN J. 2007;85:972–88.
11. Warttig S, Alderson P, Campbell G, Smith AF. Interventions for treating inadvertent postoperative hypothermia. Cochrane Database of Systematic Reviews. 2014;(11):CD009892.
12. Madrid E, Urrutia G, Roque i Figuls M, Pardo-Hernandez H, Campos JM, Paniagua P, et al. Active body surface warming systems for preventing complications caused by inadvertent perioperative hypothermia in adults. Cochrane Database of Systematic Reviews. 2016;4:CD009016.
13. Campbell G, Alderson P, Smith AF, Warttig S. Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database of Systematic Reviews. 2015;(4):CD009891.
14. Karalapillai D, Story D, Hart GK, Bailey M, Pilcher D, Schneider A, et al. Postoperative hypothermia and patient outcomes after major elective non-cardiac surgery. Anaesthesia. 2013;68(6):605–11.
15. Salota V, Slovakova Z, Panes C, Nundlall A, Goonasekera C. Is postoperative tympanic membrane temperature measurement effective? Br J Nurs. 2016;25(9):490–3.
16. Bashaw MA. Guideline implementation: preventing hypothermia. AORN J. 2016;103:304–13.
17. Munday J, Delaforce A, Forbes G, Keogh S. Barriers and enablers to the implementation of perioperative hypothermia prevention practices from the perspectives of the multidisciplinary team: a qualitative study using the Theoretical Domains Framework. J Multidiscip Healthc. 2019;12:395–417.
18. Hegarty J, Walsh E, Burton A, Murphy S, O'Gorman F, McPolin G. Nurses' knowledge of inadvertent hypothermia. AORN J. 2009;89(4):701–4, 7–13.
19. Giuliano KK, Hendricks J. Inadvertent perioperative hypothermia: current nursing knowledge. AORN J. 2017;105(5):453–63.
20. Gasim GI, Musa IR, Abdien MT, Adam I. Accuracy of tympanic temperature measurement using an infrared tympanic membrane thermometer. BMC Res Notes. 2013;6:194.
21. Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect (Larchmt). 2017;18(6):722–35.
22. Doyle DJ, Garmon EH. American Society of Anesthesiologists Classification (ASA Class). Treasure Island, Florida: StatPearls Publishing; 2020.
23. Kleimeyer JP, Harris AHS, Sanford J, Maloney WJ, Kadry B, Bishop JA. Incidence and risk factors for postoperative hypothermia after orthopaedic surgery. J Am Acad Orthop Surg. 2018;26(24):e497–e503.
24. Karalapillai D, Story DA, Calzavacca P, Licari E, Liu YL, Hart GK. Inadvertent hypothermia and mortality in postoperative intensive care patients: retrospective audit of 5050 patients. Anaesthesia. 2009;64(9):968–72.
25. Horn EP, Bein B, Bohm R, Steinfath M, Sahili N, Hocker J. The effect of short time periods of pre-operative warming in the prevention of peri-operative hypothermia. Anaesthesia. 2012;67(6):612–7.
26. Kongsayreepong S, Chaibundit C, Chadpaibool J, Komoltri C, Suraseranivongse S, Suwannanonda P, et al. Predictor of core hypothermia and the surgical intensive care unit. Anesth Analg. 2003;96(3):826–33.
27. Mohanty S, Rosenthal RA, Russell MM, Neuman MD, Ko CY, Esnaola NF. Optimal perioperative management of the geriatric patient: a best practices guideline from the American College of Surgeons NSQIP and the American Geriatrics Society. J Am Coll Surg. 2016;222(5):930–47.
28. Su SF, Nieh HC. Efficacy of forced-air warming for preventing perioperative hypothermia and related complications in patients undergoing laparoscopic surgery: a randomized controlled trial. Int J Nurs Pract. 2018;24(5):e12660.
29. Torossian A, Van Gerven E, Geertsen K, Horn B, Van de Velde M, Raeder J. Active perioperative patient warming using a self-warming blanket (BARRIER EasyWarm) is superior to passive thermal insulation: a multinational, multicenter, randomized trial. Journal of Clinical Anesthesia. 2016;34:547–54.
30. Nierman DM. Tools that we use: if you can't measure it, you can't manage it. Critical Care Medicine. 2007;35(1):312–3.









Comments