Suffering related to care among older patients on perioperative care pathways
Patients move quickly between different units during the surgical pathway. Older patients in particular are at risk of suffering related to care such as violations of dignity, neglect and poor pain management.
Background: Older patients who are admitted to hospital for surgery are moved quickly between different levels in the health service. These patients can be exposed to unnecessary suffering related to care, which can become an additional burden and impede convalescence.
Objective: To describe nurses’ experiences with suffering related to care that is inflicted on older patients undergoing surgical procedures.
Method: The study has a qualitative, exploratory design and comprises a total of seven interviews. We conducted one focus group interview, five qualitative in-depth interviews with two informants in each group and one individual interview with one nurse. Fifteen nurses participated, who either worked in the community nursing service, nursing homes or operating theatres.
Results: The nurses who participated had experienced nurses behaving disrespectfully towards older patients. Conflicts of values arose in the interaction between patients and healthcare personnel, and it was difficult to discuss unethical behaviour with managers or colleagues. Patients did not always receive appropriate pain relief and did not always receive help when they pressed the alarm button or asked for help.
Conclusion: Older patients are at risk of suffering related to care in the form of violations of dignity, neglect and lack of appropriate pain relief during the surgical pathway, where patients are moved quickly between different units. Suffering that is unnecessarily inflicted on patients can be prevented by talking to the patient and his or her family. Ethically responsible management requires good communication and ethical reflection with colleagues on observed violations of dignity.
Major changes have taken place in the treatment of surgical patients. The changes mean shorter stays in hospital in connection with surgical treatment, including for older patients. These patients can be exposed to suffering beyond the illness itself and the treatment. In this article, we chose to use the terms ‘unnecessary suffering related to care’ and ‘unnecessary suffering’.
Eriksson describes ‘suffering related to care’ as a violation of the patient’s dignity, absence of care, condemnation, punishment and the exercising of power (1). Dahlberg’s term ‘unnecessary suffering’ is described as negative encounters with healthcare personnel that make patients vulnerable, and this suffering is caused by a lack of care (2).
Everyone wants to be well looked after, receive considerate nursing care and be treated with understanding, dignity and respect by the health service (3, 4). However, patients sometimes encounter healthcare personnel who subject them to indignities, and by so doing cause them to suffer. Healthcare personnel can be rude and disrespectful, and they can ignore and humiliate patients and treat them as if they are invisible (2, 5–7).
Albina gives an example of an older man being subjected to serious violations of dignity in the form of physical touching and offensive language in connection with an operation (8). Willassen et al. refer to an example of a patient’s pain being ignored, and give examples of offensive language in the form of negative comments about the patient’s body (9).
Care pathway
In our study, the nurses refer to patients aged 60+. The World Health Organization (WHO) defines people between the ages of 60 and 75 as ‘early elderly’, and people over 75 as ‘late elderly’. Older patients are often moved to convalescence wards or their home shortly after surgery, and this process is referred to as a care pathway, treatment pathway, treatment loop or trauma chain (10).
A surgical care pathway is normally divided into three phases: preoperative, intraoperative and postoperative. The preoperative phase is the time from which it is decided that the patient should be operated until the patient arrives in the operating theatres. This period involves preparations for patients and staff. In the operating theatre, the patients are taken care of by the surgical team, which mainly consists of a surgeon, theatre nurses, an anaesthetist and a nurse anaesthetist (3, 11, 12).
Perioperative nursing care
The term ‘perioperative nursing’ was adopted in the USA in the 1970s. Lindwall and von Post define perioperative nursing as the nursing actions and nursing activities performed by theatre nurses and nurse anaesthetists during the pre-, intra- and postoperative phases of surgery, normally in operating theatres (13).
In the Nordic countries, the qualifications and areas of responsibility of these specialist nurses vary, and the scope of work for perioperative nurses can vary from hospital to hospital and from country to country (14). In its broadest sense, perioperative nursing can nowadays include contact with and caring for the patient at outpatient clinics, recovery units, day surgery operating theatres and contact with the patient via telephone before and after surgery (14).
Responsibility to protect the patient
Theatre nurses and nurse anaesthetists work in a multidisciplinary surgical team along with doctors, engineers and porters, and the entire team has a duty to work in a caring manner (4). Theatre nurses have a special responsibility for protecting patients from embarrassment and ensuring that they do not suffer indignities when they are naked or defenceless (4).
Research such as ours on suffering related to care throughout the treatment pathway is new. It is important to learn more about the nurses’ perspectives of the suffering inflicted on patients in the perioperative phase in order to develop the nursing care.
Objective of the article
The purpose of this article is to describe nurses’ experiences with suffering related to care that is inflicted on patients. The findings in this article appeared in a study we conducted on patient safety and older patients (15).
Method
Design
We chose a qualitative method with semi-structured interviews, and a content analysis of the data material was performed (16).
Sample
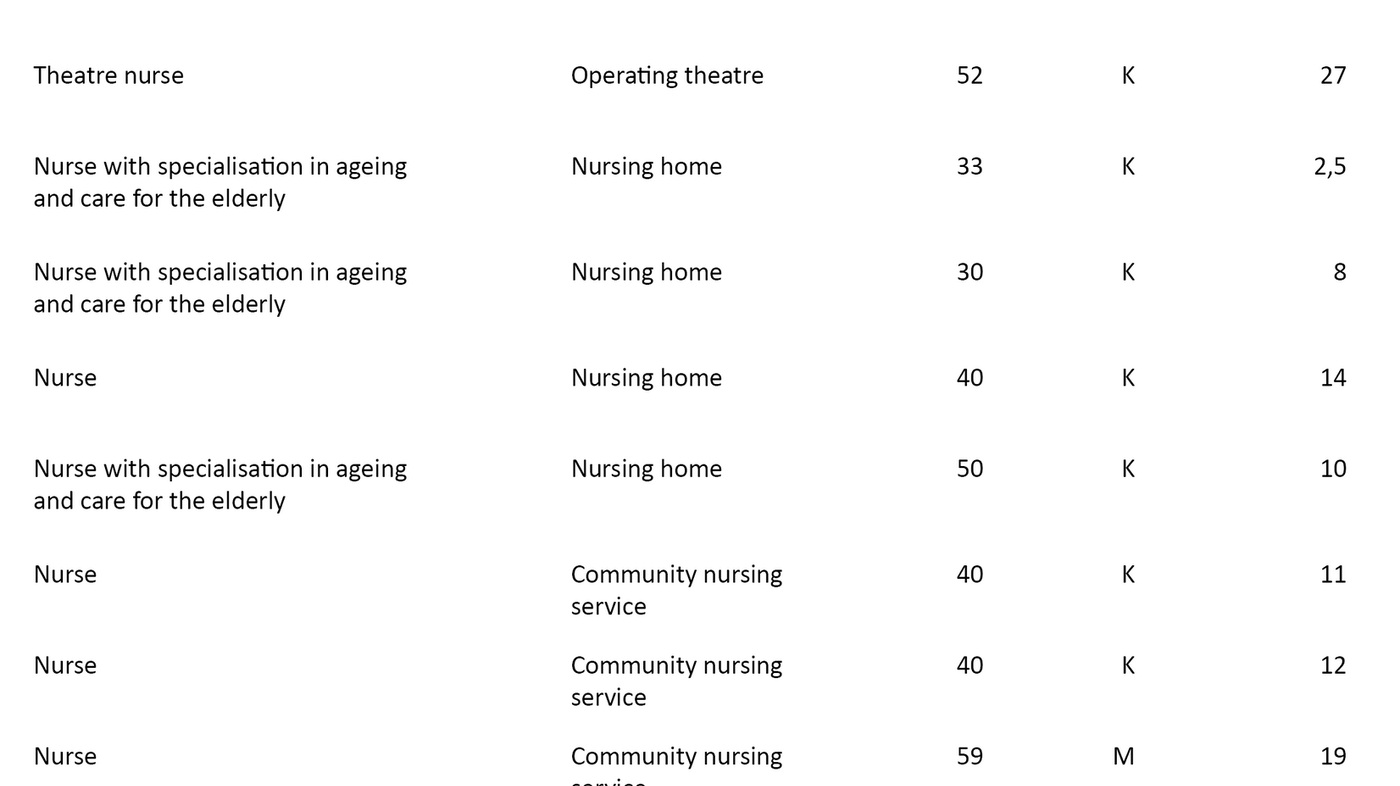
We interviewed 15 nurses working in small and large urban municipalities. These nurses worked in operating theatres, nursing homes and the community nursing service. In order to strengthen and enrich the study and gain an inside perspective from the entire course of the patient’s care pathway, we chose a combination of a focus group interview with four participants, five interviews with two participants and one individual interview. Table 1 shows detailed information about the participants.
Data collection
We contacted managers in hospitals and local authorities, who arranged contact with the nurses we interviewed. The interviews were conducted during the period March 2014 to September 2015. The main questions concerned patient safety for older patients undergoing surgery. We used an interview guide that we devised based on literature and the authors’ experiences.
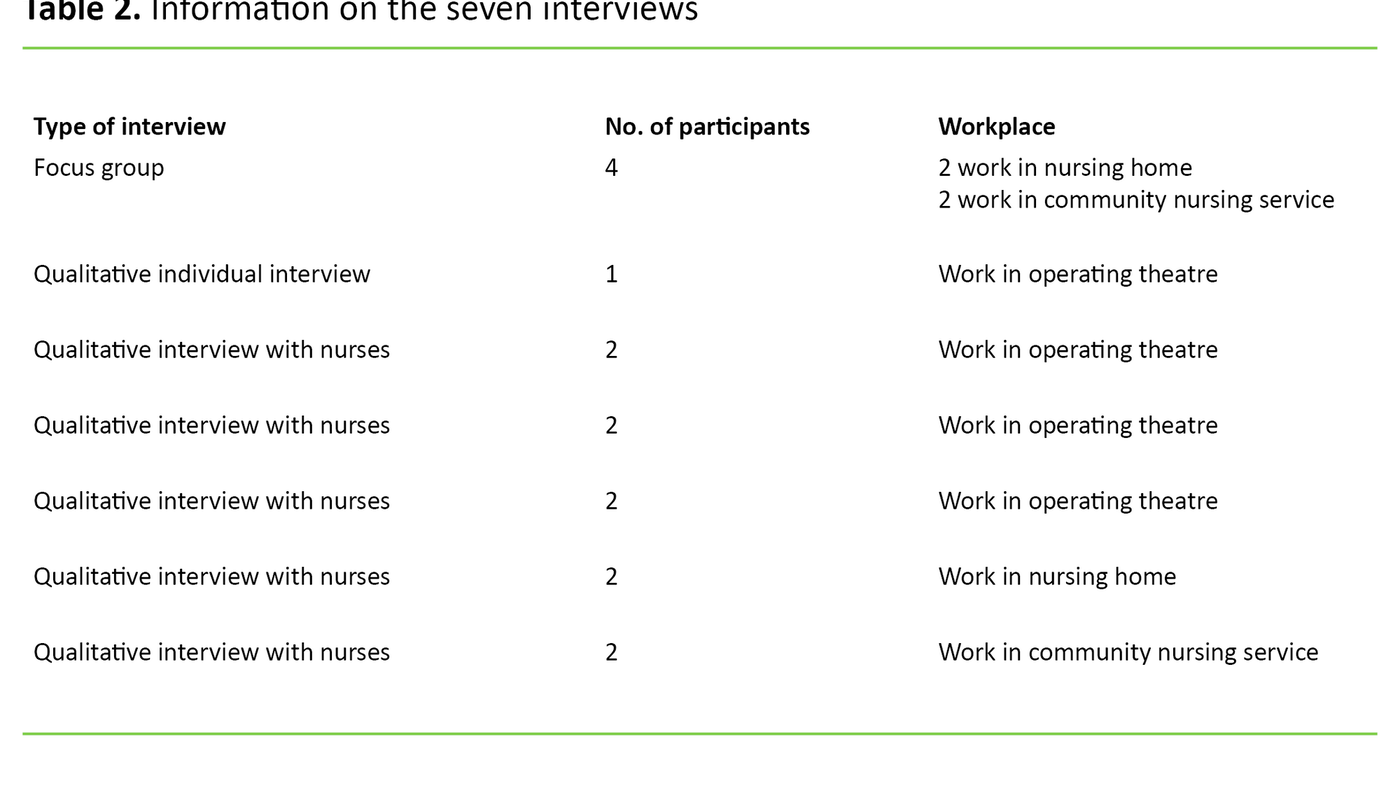
The interviews comprised of a total of 23 questions. The questions were open-ended, and we also asked for further details when the nurses described experiences in which patients had been subjected to offensive language or neglect, or had been ignored. We also asked if the nurses could give us examples of such incidents. We conducted a total of seven interviews: one interview with one participant, five interviews with two participants and one focus group interview.
Four nurses participated in the focus group interview: two worked in a nursing home and two were part of the community nursing service. The third author was the moderator in this interview, and her task was to get the participants to talk to each other and to manage the social dynamics so that everyone was heard. The second author conducted all the interviews, while the first author took notes and asked supplementary questions (16). Table 2 shows details of the interviews.
Analysis
After the interviews, we prepared summaries and noted the main impressions. The first author transcribed all the interviews apart from one. We performed a qualitative content analysis of the data material (17, 18). This method of analysis was chosen because it is considered to be suitable for examining participants’ experiences, attitudes, motives and thoughts, as well as for examining some of the topics in more depth.
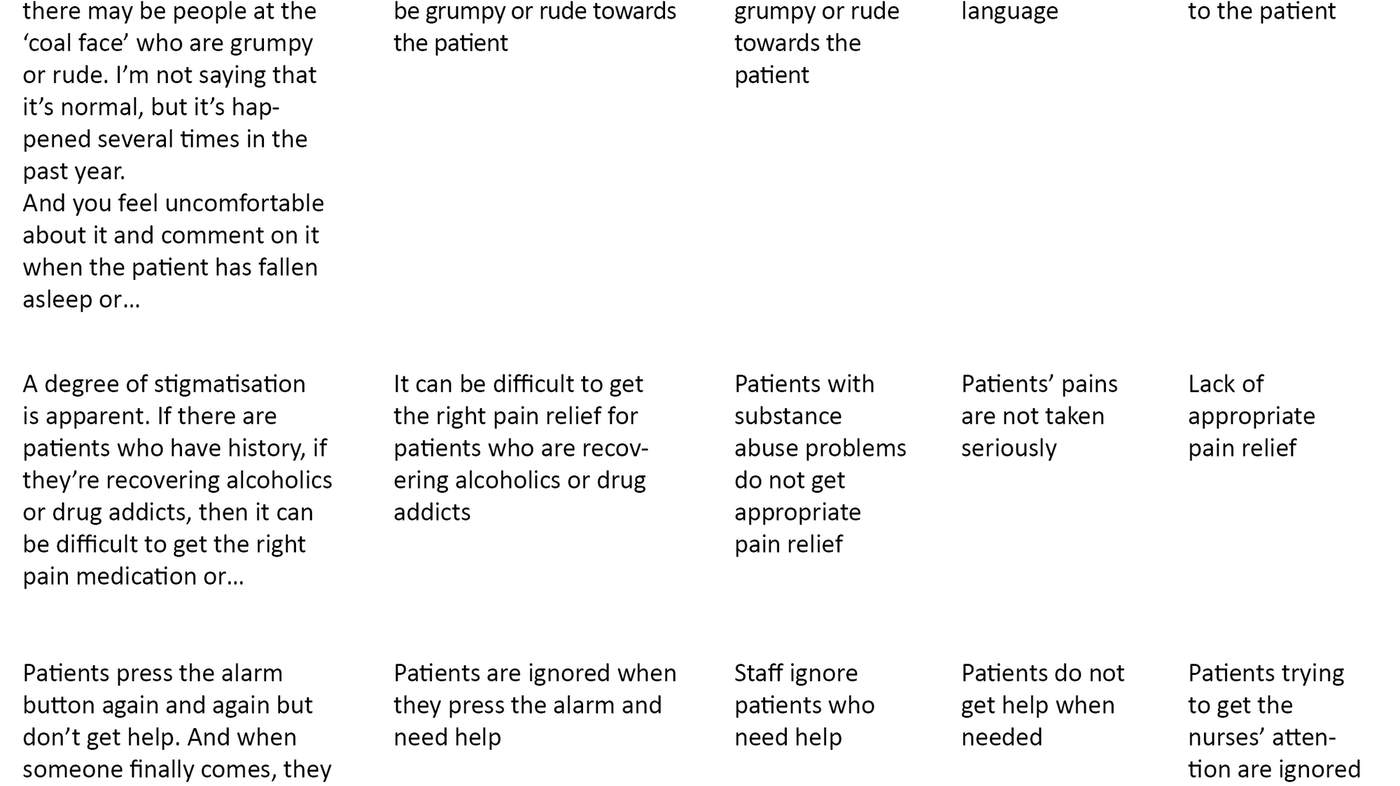
The first and second authors listened to the recordings and read through the texts several times. The statements were then broken down into meaning units, which were then condensed, coded and thematised (17, 18).
The first author had the main responsibility for the analysis, but regular meetings were held with all the authors where analyses, interpretations and text were reviewed and analysed. Table 3 gives examples of how the statements were broken down into meaning units, condensed meaning units and codes, and how these were sorted into sub-themes and main themes.
Ethical considerations
We provided written and oral information about the study to the managers and informants. The nurses signed an informed consent form. They stated their age, qualifications and number of years in the profession prior to interview, with the exception of the first interview, where this information was provided during the interview itself.
We informed the nurses that the study was voluntary and that they had the right to withdraw without giving a reason. Four informants withdrew on the day we had arranged to conduct the interviews. The study was reported to the Norwegian Centre for Research Data (project number 37833).
Results
The nurses in the study had experienced that suffering related to care, such as disrespectful behaviour, was being inflicted on patients, and that healthcare personnel neglected patients who were trying to get their attention. Conflicts of values made it particularly difficult for the nurses to discuss the suffering inflicted on patients with colleagues and management.
Disrespectful behaviour towards patients
The nurses from nursing homes gave examples of patients with cognitive impairments and dementia diagnoses being subjected to offensive language. They also provided examples of staff non-conformance notices being submitted because personnel had acted inappropriately towards patients.
Theatre nurses
The theatre nurses described incidences of violations of dignity by both nurses and doctors in the surgical team. This related to swearing and other language that the nurses considered to be inappropriate. One theatre nurse described it as follows:
‘You do see patients’ dignity being violated, particularly in relation to offensive language, by the nurses and doctors in the surgical team, and it’s very difficult to address the issue.’
Another theatre nurse said the following:
‘The nurse anaesthetist actually sedated a patient so that they didn’t have to experience the surgeon’s inappropriate language. I don’t think we’re the only hospital in Norway that has this problem.’
Several theatre nurses claimed that offensive language towards patients was a common problem in many operating rooms and that it was difficult to raise the issue with colleagues.
Lack of appropriate pain relief
The nurses reported that older patients did not always receive appropriate pain relief. One nurse employed in the community nursing service said the following:
‘Violations of dignity in relation to pain. I’ve experienced that a lot, where a patient’s claims of pain are treated with scepticism.’
Nurses from the community nursing service and nursing homes had witnessed the stigmatisation of patients with substance abuse problems. They had also experienced patients not being given appropriate pain relief after surgery. One nurse said the following:
‘Unfortunately, it’s perhaps all too common for us to have a high threshold for providing any medication. There’s probably a reluctance to give morphine, for example, because you then need to keep a closer eye on the patient when we’re understaffed, and nurses may also be afraid that the patient will fall.’
A nurse in the convalescence ward said that a patient told the doctor that he had received poor pain relief after surgery. It transpired from his medical records that the patient had not received any of the pain medication that had been prescribed for use as needed. The nurse made the following observation:
‘Not providing medicine when needed, that’s totally wrong. Maybe we’re afraid of giving too much pain relief as there’s been a lot of press coverage about patients being sedated, so it’s a very complicated issue.’
Patients trying to get the nurses’ attention were ignored or neglected
In the interviews, nurses described how patients who try to get the nurses’ attention are neglected. The nurses working in nursing homes said that patients were ignored, and that they did not get help when they pressed the alarm button. One said the following:
‘They’ve been ignored. When someone presses the alarm button it’s registered as a non-conformance, and no one goes to see to them.’
Nurses described it as very difficult for patients and an affront to their dignity when they do not receive help when they are in pain or discomfort, or need assistance for other reasons.
Discussion
This article highlights suffering related to care that is inflicted on older patients undergoing surgical treatment and care. In the study, we find disrespectful behaviour towards patients, lack of pain relief and neglect on the part of the healthcare personnel when patients try to get their attention. Vulnerable groups, such as patients in a state of confusion or with cognitive impairments, were particularly at risk, as were older patients with substance abuse problems.
Studies, including from operating theatres, show that patients are subjected to serious and unacceptable violations of dignity (7, 9). Albina gives examples of serious violations of dignity in a patient receiving perioperative nursing care. She points out that patients undergoing surgery are in a particularly vulnerable situation because they are anaesthetised (8).
It can be difficult to get healthcare personnel to talk about such reprehensible behaviour. According to Eriksson, patients can feel spiritual and mental distress as a result of humiliation by fellow human beings. They may also feel a sense of guilt in relation to their treatment or illness. These are feelings that are manifested within the patient, but they can also occur due to the judgmental attitude of nursing staff (1).
Lindwall and von Post describe how patients suffer during humiliating actions. They explain that if healthcare personnel really want to protect a patient’s dignity, they must force themselves to see what they do not want to see. Furthermore, they argue that conflicts of values arise when nurses witness rude behaviour by other healthcare personnel. They conclude that it is necessary to discuss and reflect on such reprehensible behaviour, which causes the patients to suffer and leaves them feeling humiliated (19).
Perioperative care involves theatre nurses and nurse anaesthetists safeguarding patient care. Their role is to protect patients from suffering beyond that caused by the surgical procedure. Dahlberg and Martinsen describe how perioperative nurses are there to protect patients from violations of dignity and ensure that they are not subject to any unnecessary suffering (2, 4).
Nordtvedt believes that moral sensitivity is characterised by identifying and intercepting the morally relevant features of a situation. To illustrate a situation where nurses should be particularly careful with patients, he uses the example of protecting a patient’s dignity when exposed (20). Theatre nurses are well-versed in such situations in connection with the surgical positioning of patients, i.e. placing them in a particular physical position to enable the operation to be carried out. The theatre nurse must safeguard the patient’s integrity and dignity by preventing their body from being exposed (20).
Guidelines on professional ethics state that the nurse must safeguard the individual patient’s dignity and integrity, and that the patient has the right to comprehensive nursing care, the right to shared decision-making and the right not to be subjected to indignities (21). According to the legislation, healthcare personnel must perform the work in a way that meets the requirement for professionally responsible and caring nursing (13). Our study shows that serious violations of dignity have occurred and that suffering related to care has been inflicted on patients.
Disrespectful behaviour towards patients
Nurses have a professional, ethical and legal responsibility to speak out against violations of patients’ dignity and to not participate in or tolerate unacceptable behaviour (3, 21, 22). The nurses described how they felt uncomfortable when such undesirable events occurred, which concurs with the findings of Lindwall and von Post (13).
The nurses had experienced difficult situations and had chosen to give the patients extra sedatives to make them sleep. They wanted to spare patients from verbal outbursts by members of the surgical team. This method of protecting vulnerable patients is debatable, but nurses can feel pressure to act and resolve the situation in the best way possible.
It is important that healthcare personnel have good collaboration skills and that they find good ways to communicate. It is not uncommon for conflicts to arise in the operating room. In the worst case, conflicts can pose a risk to a patient’s safety, or the patient can feel violated (13, 14).
Our findings are consistent with Willassen et al. (15), who describe undignified care and violations of dignity in perioperative practices and conclude that there is a need for reflection and discussion on ethics and dignity in the field. They further conclude that these issues need to be discussed in study programmes in order to raise awareness of attitudes and help change these for the benefit of patients, staff and students (9).
There are many different explanations for disrespectful behaviour towards patients. It can be blamed on work-related stress factors, physical or mental illness, abuse, thoughtlessness or fear of making a mistake (18). Power hierarchies, fear of reprisal or bullying are some of the reasons why healthcare personnel are unable to deal with these difficult situations. Various communication problems also cause adverse events (15).
Nordtvedt believes that there are many explanations for how a moral breakdown can occur. He cites power hierarchies, blind obedience, emotional numbness, ideology, sadism and lack of empathy as causes of moral breakdown (23). The degree of openness in the patient safety climate will determine how easy staff think it is to talk about risks and adverse events in the workplace (24).
In the USA, professional development courses for nurses and doctors whose conduct poses a risk to patient safety have long been used as a tool for behavioural change. Early feedback from staff and managers is important for the employee to understand the impact of his or her behaviour (25).
Lack of appropriate pain relief
Our findings show that patients do not always receive appropriate pain relief following surgical procedures. The nurses gave examples of individual patients being stigmatised. The examples concerned drug addicts and are taken from nursing homes and the community nursing service.
The lack of appropriate pain relief for vulnerable patient groups after surgery is a serious situation that leads to suffering for the patients. Pain-based behaviour, pain-based emotions and experiences of pain differ from patient to patient, and they are also contingent on culture (26).
Failure to give patients appropriate pain relief represents a serious lack of care (1). Possible solutions for nurses may be to update their knowledge of pain and pain-based behaviour and emotions in different cultures, participate in learning networks and form a closer working relationship with pharmacists and doctors. Pain relief can help prevent falls among older patients.
Multidisciplinary collaboration, annual medication reviews and home care rehabilitation all play a major role in fall prevention. Fall prevention in healthcare institutions is a priority area for the Norwegian patient safety programme (27).
Closer collaboration between the specialist health service and the primary health service, better nursing documentation, the use of interpreters and the sharing of necessary information when patients are moved between different levels in connection with surgical procedures are all crucial (28). It is essential to develop greater collaboration across treatment levels.
Patients trying to get the nurses’ attention were ignored or neglected
The nurses from the nursing homes provided examples of patients not receiving help when they pressed the alarm button. Dahlberg also refers to examples where patients do not have access to the alarm button and are therefore unable to call for help when needed (2).
Report no. 13 to the Storting, ‘Quality and Patient Care’, states that patients’ families are concerned about the lack of dignity, care, trust and safety for frail people over the age of 80 living at home. They do not receive help at the agreed time, and there are not enough qualified staff (24). The families are often a source of strength for older patients when they are admitted to a hospital or nursing home and when they receive home nursing care.
Martinsen gives an example where a woman with cancer who is in the last week of her life was denied assistance from a nurse to find a more comfortable position. The woman pressed the alarm button, but did not get help. The nurse acted shamelessly and used the fact she was busy as an excuse for not helping a vulnerable patient in severe pain (28). Malmedal points out that bad attitudes and poor management, lack of knowledge and tight financial frameworks may be the reasons behind patients not receiving help (6).
Conclusion
We collected data across health service levels. In the study, there are examples of disrespectful behaviour, lack of appropriate pain relief and neglect when the patients tried to get the staff’s attention, and the findings suggest that unnecessary suffering is inflicted on older patients. The nurses’ most important task is to alleviate suffering and promote good health. Nurses, managers and other healthcare personnel must work together to prevent more suffering being inflicted on older patients, particularly when continuity in the nursing is a challenge.
The study shows the importance of person-centred care, better collaboration between the different service levels and better pain management. Perioperative nurses must communicate with the patient throughout the entire course of the patient’s care pathway, and not just at the time of surgery.
The study also shows that the primary and specialist health services should include Lindwall and von Post’s perioperative dialogue model. This model places the focus on patient dignity, which includes contact with patients and their families, and dialogue between staff within and between units. Openness and discussion in connection with violations of dignity in the working environment are needed to improve the safety climate. It is crucial that nurses discuss how to deal with such situations.
More research is needed in this area, which also encompasses patients’ and their families’ experiences of suffering related to care that is inflicted in connection with surgery. Nurses should lead the way in promoting a caring environment for patients and staff, and they must have the courage to address adverse events. By not reporting unacceptable behaviour, they are allowing such attitudes and behaviour to continue.
We thank the informants who participated in the study and the managers who helped us gain access to the field. We also thank the Norwegian Association of Operating Room Nurses for providing project funds, which made the study possible.
References
1. Eriksson K. Det lidende mennesket. TANO; 1995. Available at: https://www.nb.no/nbsok/nb/0d79cb121e3390070c32a13495f4b681?lang=no#24(downloaded 05.04.2018).
2. Dahlberg K. Vårdlidande – det onödiga lidandet. Nordic Journal of Nursing Research. 2002;22(1):4–8.
3. Dåvøy GAM, Eide PH, Hansen I. Operasjonssykepleie. 2. ed. Oslo: Gyldendal Akademisk; 2018.
4. Martinsen K. Operasjonssykepleieren og den sårbare pasienten. In: Dåvøy GAM, Eide PH, Hansen I, eds. Operasjonssykepleie. 2. ed. Oslo: Gyldendal Akademisk; 2018: p. 130–146.
5. Schjøtler G, Delmar C. Angst, sårbarhed og skam – operationspatienters sanseerfaringer. Klinisk Sygepleje. 2016;30(01):17–30.
6. Malmedal W. Sykehjemmets skyggesider: når beboere i sykehjem utsettes for krenkelser og overgrep. Oslo: Kommuneforlaget; 1999. Available at: http://www.nb.no/nbsok/nb/87e05ae260bb654022d3df693f62e068.nbdigital?lang=no#0(downloaded 14.03.2018).
7. Linh M, Bergens A. När beteendet blir en patientsäkerhetsrisk. Läkartidningen. 2015;112:DFI6. Available at: https://www.researchgate.net/profile/Marion_Lindh/publication/281828685_In_Process_Citation/links/5638d96408ae4bde5021e00f.pdf(downloaded 14.04.2018).
8. Albina JK. Patient abuse in the health care setting: The nurse as patient advocate. AORN Journal. 2016;103(1):73–81.
9. Willassen E, Blomberg A-C, von Post I, Lindwall L. Student nurses’ experiences of undignified caring in perioperative practice – Part II. Nursing Ethics. 2015;22(6):688–99.
10. Orvik A. Organisatorisk kompetanse: innføring i profesjonskunnskap og klinisk ledelse. 2. ed. Oslo: Cappelen Damm Akademisk; 2015.
11. Rothrock JC, McEwen DR, Alexander EL. Alexander's care of the patient in surgery. 15. ed. St. Louis, MO: Elsevier Mosby; 2015.
12. Lindwall L, von Post I. Perioperativ vård: att förena teori och praxis. Lund: Studentlitteratur; 2008.
13. Lindwall L, von Post I. Perioperativ vård: den perioperativa vårdprocessen. Lund: Studentlitteratur; 2000.
14. Steelman VM. Concepts basic to perioperative nursing. In: Rothrock JC, ed. Alexander's care of the patient in surgery. St. Louis, MO: Elsevier Mosby; 2015: p. 1–15.
15. Eliassen E, Holla S, Bondas T. Risiko for uheldige hendelser i perioperative pasientforløp til eldre – en kvalitativ studie. Klinisk Sygepleje. 2018;32(2):94–110.
16. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 3. ed. Oslo: Gyldendal Akademisk; 2015.
17. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–12.
18. Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nursing & Health Sciences. 2013;15(3):398–405.
19. Lindwall L, von Post I. Preserved and violated dignity in surgical practice – nurses’ experiences. Nursing Ethics. 2014;21(3):335–46.
20. Hansen I, Brekken RS. Leiring av pasienten på operasjonsbordet. In: Hansen I, Eide PH, Dåvøy GAM, eds. Operasjonssykepleie. Oslo: Gyldendal Akademisk; 2018: p. 320–39.
21. Yrkesetiske retningslinjer for sykepleiere : ICNs etiske regler. Oslo: Norsk Sykepleierforbund; 2011. Available at: https://www.nsf.no/vis-artikkel/2193841/17102/Yrkesetiske-retningslinjer(downloaded 12.04.2018).
22. Lov 2. juli 1999 nr. 64 om helsepersonell (helsepersonelloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-64(downloaded 18.02.2019).
23. Nordtvedt P. Makt kan føre til ondskap. Oslo: Sykepleien; 2014. Available at: https://sykepleien.no/sites/default/files/publication-pdf/etikk_11.pdf (downloaded 03.04.2018).
24. Meld. St. nr. 13 (2016–2017). Kvalitet og pasientsikkerhet 2015. Oslo: Helse- og omsorgsdepartementet; 2016. Available at: https://www.regjeringen.no/no/dokumenter/meld.-st.-13-20162017/id2524141/(downloaded 18.02.2019).
25. Samenow CP, Worley LLM, Neufeld R, Fishel T, Swiggart WH. Transformative learning in a professional development course aimed at addressing disruptive physician behavior: a composite case study. Academic Medicine. 2013;88(1):117–23.
26. Ellingsen S, Drageset S. Peroperativ smertelindring. In: Dåvøy GAM, Eide PH, Hansen I, eds. Operasjonssykepleie. 2. ed. Oslo: Gyldendal Akademisk; 2018. p. 478–89.
27. Forebygging av fall i helseinstitusjoner. Pasientsikkerhetsprogrammet I trygge hender 24/7. Oslo: Helsedirektoratet. Available at: http://www.pasientsikkerhetsprogrammet.no/om-oss/innsatsomr%C3%A5der/forebygging-av-fall-i-helseinstitusjoner(downloaded 18.02.2019).
28. Naustdal A, Netteland G. Sjukepleiedokumentasjon i eit elektronisk samhandlingsperspektiv. Oslo: Sykepleien Forskning. 2012;3(7):270–7. DOI: 10.4220/sykepleienf.2012.0133.










Comments