Perceptions of postnatal care after emergency caesarean sections
Women who had given birth by caesarean section often downplayed their own complaints, felt left to their own devices and received invaluable assistance from their partner.
Background: In Norway and other European countries, women are less satisfied with the postnatal care they receive than with the antenatal and birthing care. Postnatal care in Norway is changing, with the number of nights in hospital being reduced, including for women who have undergone a caesarean section.
Objective: To investigate women’s perceptions of the physical health care they received in the maternity ward following an emergency caesarean section.
Method: Qualitative study involving a convenience sample consisting of ten women who had given birth by emergency caesarean section. We conducted semi-structured, individual interviews and analysed the data using systematic text condensation.
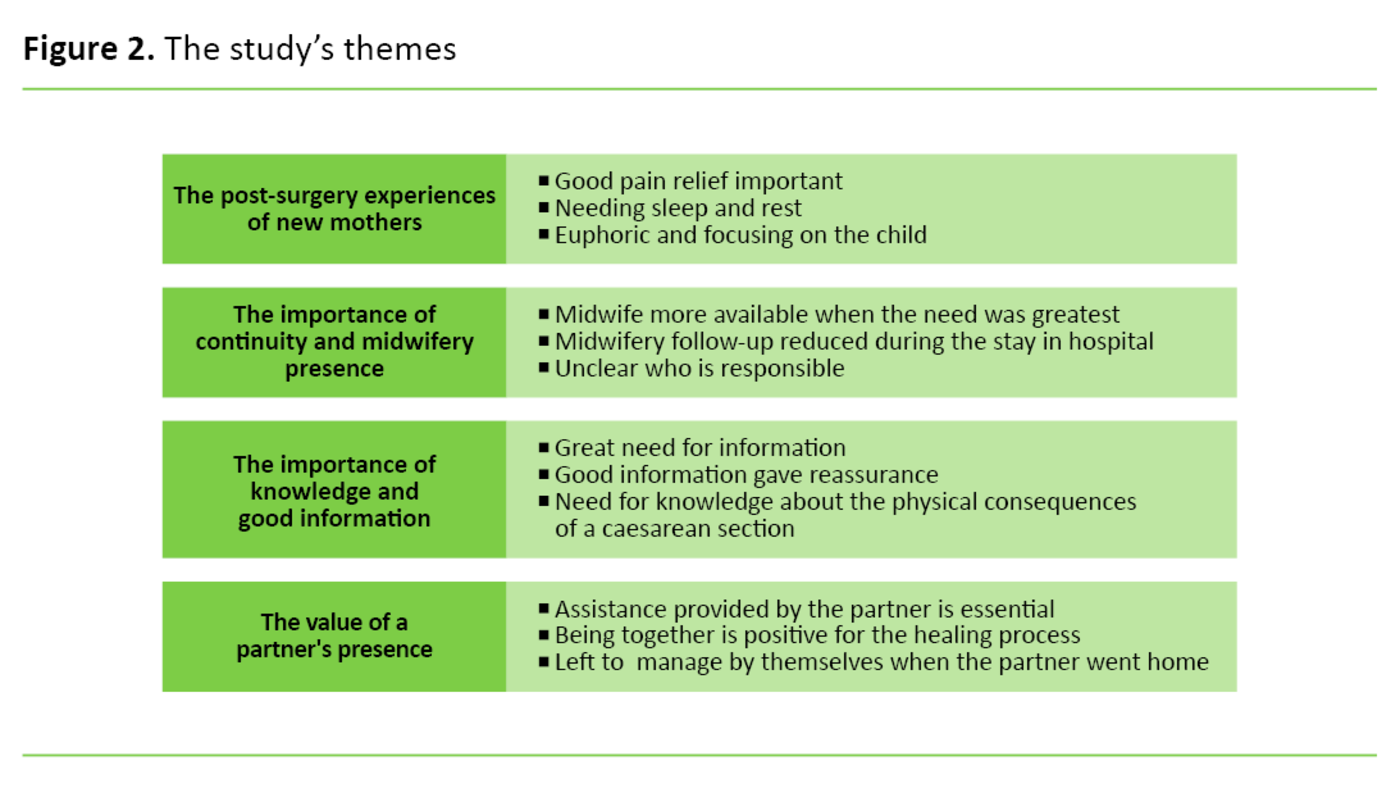
Results: The analysis highlighted four themes: the post-surgery experiences of new mothers, perceptions of continuity and midwifery presence, the importance of knowledge and good information, and the value of a partner’s presence.
Conclusion: The study shows that women who had given birth by emergency caesarean section felt that they received poor physical health care in the maternity ward.
Many women in Norway unexpectedly undergo surgery just as they embark on life as a new mother. In 2017, 16 per cent of all births in Norway were by caesarean section, and 65 per cent (5870) of these were emergency procedures (1). However, the caesarean section rate in Norway is among the lowest in the western world (2).
Since the 1960s, new mothers have been handed an increasing degree of responsibility for their own child during their stay in the maternity ward, while the number of routine observations and interventions has been reduced (3). This development stems from the view that giving birth is a natural process, but also from a wish within the health service to prioritise patients who are seriously ill (4).
In Norway, new mothers tend to stay in hospital for two or three days after a normal birth, and early departure is desirable (5). Report no. 12 to the Storting, ‘A Happy Event’, pointed to the need for systematic collection of service user experiences and information from medical personnel in order to learn what aspects of postnatal care ought to be improved (4).
In 2016, a nation-wide survey of service users’ perceptions of antenatal, birthing and postnatal care found that the least favourable reports concerned the postnatal stay in hospital (6). When asked whether they had received sufficient information about their own physical health after the birth, as many as 19 per cent of respondents answered ‘not at all’ or ‘to a small extent’, while 27 per cent answered ‘to some extent’ (6).
Possible complications
A caesarean section may give rise to complications such as endometritis, embolism (7) and operating wound infections. The risk of re-admission to hospital is higher after a caesarean section than after a vaginal delivery (8, 9), particularly among women who have undergone emergency surgery (10). All forms of caesarean section are associated with poorer health and quality of life compared to spontaneous vaginal deliveries (11).
Studies describe dissatisfaction and insufficient postnatal follow-up in hospital (9, 12–14) and point out that postnatal care is a low-priority area that has a lower status than birthing care amongst healthcare personnel (13). According to Fenwick et al. (15), women who give birth by emergency caesarean section sometimes experience a difficult postpartum period. Many feel that they receive insufficient physical assistance at the hospital.
Objective of the study
We are aware that there are mental as well as physical aspects to the concept of health, and that its interpretation is culturally and historically conditioned. It is therefore challenging to distinguish between physical and mental health following a caesarean section, where bodily challenges and existential experiences are closely intertwined.
It is nevertheless useful to explore how women perceive the care that is provided for their physical health after an emergency caesarean section, because caesarean sections carry a higher risk of physical complications. The objective of the study was therefore to investigate how women perceived the physical health care that was provided in the maternity ward following an emergency caesarean section.
Method
Design and sample
We chose a qualitative design for the study as this is well suited for shedding light on the women’s experiences (16, 17). Using social media, we recruited a convenience sample (16) consisting of ten women. Those who wished to take part, contacted the first author and recruitment took place on an ongoing basis. Posters displayed at child health clinics in one local authority area did result in women coming forward, but these were not included in the sample because their details were received too late in the study period.
We included women who had given birth by emergency caesarean section in the period 2014–2016 and who had spent the initial postpartum period in hospital. The women were between 27 and 40 years of age, and all had been married or in a cohabiting partnership at the time of the birth. Nine women were ethnic Norwegians, while one was from a non-western background. All had a higher education. Seven women were primipara, while three were secundipara who had previously also delivered by emergency caesarean section.
We conducted individual semi-structured interviews (17) from October to November 2016. Six of the informants chose to be interviewed in their own home while four were interviewed in a meeting room at a public library. The interviews lasted between 20 and 76 minutes (40 minutes on average). Five women were accompanied by their infant during the interview, and one of them had their partner present for 5 minutes.
We made use of an interview guide and started the interviews with an open-ended question, asking the women to describe their transfer from the recovery unit to the maternity ward. The interview guide further included a question about the course of events that followed the decision to undertake an emergency caesarean section. These open-ended questions proved to be good conversation-starters.
The interview guide also included questions about assistance received with personal hygiene, mobilisation, pain relief and follow-up of the operation wound. After conducting the first interview, we added themes that referred to the value of the partner’s presence and to midwifery follow-up. The interviews were recorded, and the resultant audio files were transcribed verbatim.
Data analysis
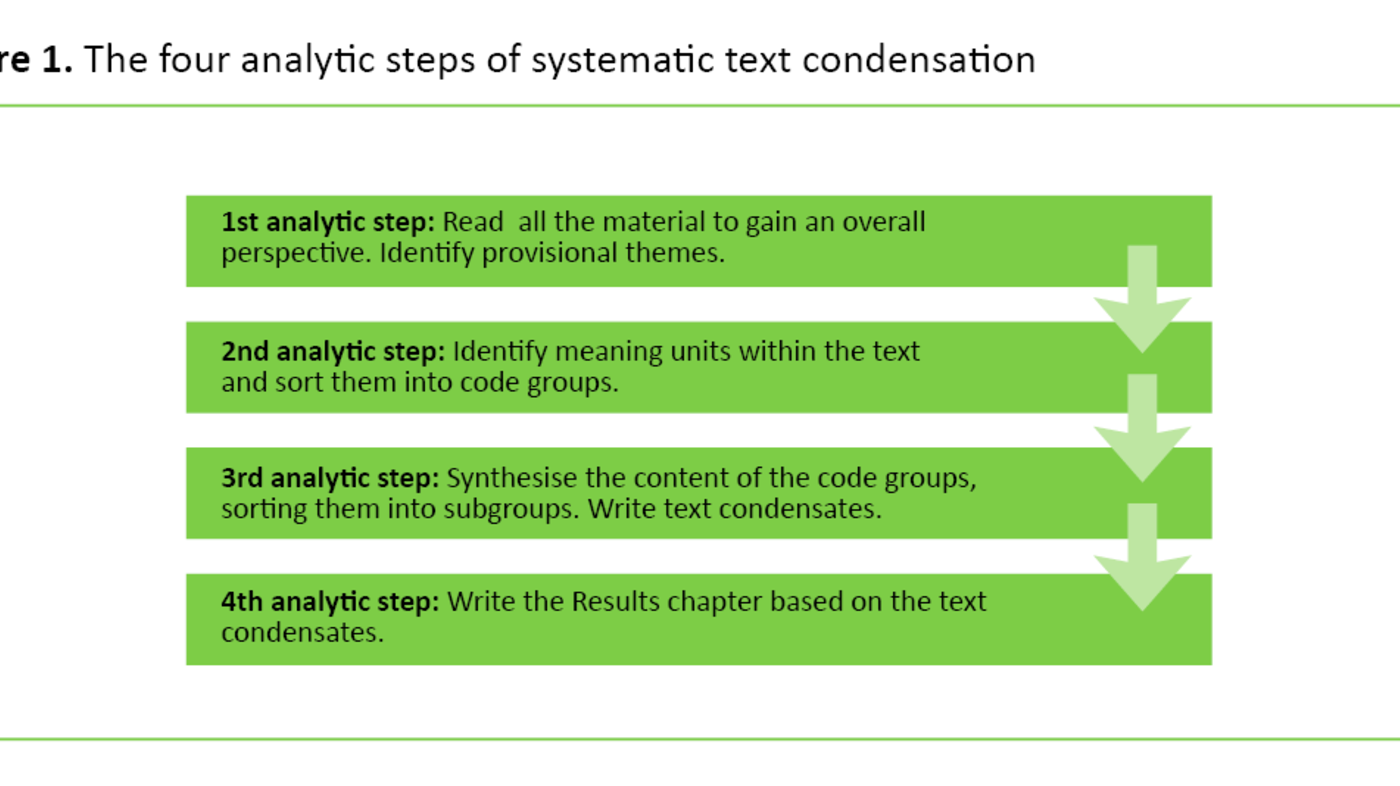
Two of the authors analysed the material by means of systematic text condensation (STC), which is a four-step thematic cross-case analysis method (16). We started the analytic work by reading all interviews in order to gain an overall perspective and identify provisional themes.
The second step involved the identification and coding of meaning units. We proceeded to focus on one code group at a time, sorting the content into subgroups that represented different nuances of the phenomenon. These were then condensed. Finally, we synthesised the condensates into a single analytic text per code group, adding appropriate quotes that shed light on the text.
Ethical considerations
The project was carried out in compliance with the Declaration of Helsinki (18). The informants received written information about the study in advance, they signed a consent form prior to being interviewed, and they were informed that they were free to withdraw from the study without giving a reason at any stage before the data had been fully processed.
The Regional Committees for Medical and Health Research Ethics (REC) found that the study fell outside the scope of Norwegian legislation on health research (REC number 2016/1105). The study was approved by the Norwegian Centre for Research Data (NSD) (project number 49227). The relevant local authority approved the poster that was displayed at child health clinics.
Results
Our analysis identified four themes: the post-surgery experiences of new mothers, perceptions of continuity and midwifery presence, the importance of knowledge and good information, and the value of a partner’s presence.
The post-surgery experiences of new mothers
The informants described various degrees of pain after the caesarean section. One woman who had undergone a caesarean section on a previous occasion, explained that the pain was more frightening the first time around, because she had been worried that her wound would open. Another woman who had been unable to fall asleep on the third night after her operation was made to feel like a drug addict when the midwife told her that she no longer should be needing morphine.
Some were so focused on the child that they took no notice of their own pain until it became overwhelming, and one informant felt like a primal female who defied her pain to look after her child. For others, the pain led to a feeling of helplessness, that rendered them incapable of caring for their child.
The informants talked about a great need for sleep, rest and respite. Family rooms were important to many in ensuring that they received sufficient sleep and rest, while others chose to go home in order to satisfy this need. The chance of staff providing respite was a key factor in this respect, and it was important to them that they would have excess energy by the time they returned home.
The informants talked about a feeling of happiness when the operation was over, and everything had gone well. Nevertheless, they felt that postnatal staff ‘forgot’ about them and their situation and that breastfeeding and breastfeeding assistance became the sole focus. In the words of one of the women:
‘And when she wasn’t at work, that really nice one, it was like everything was done with. It was all about breastfeeding from then on. People seemed to be really concerned with that! But no-one focused their attention on me anymore.’ (Interview 4)
Perceptions of continuity and midwifery presence
Some of the informants described the postnatal personnel as positive and accessible, and they explained that it had been easy to ring the bell for assistance. One woman felt that the midwife took particularly good care of her on the first day and assisted her with personal care and mobilisation, thereby making her feel safe and cared for. Others described midwives who encouraged and pressurised them to get out of bed, which they considered to be positive.
There was close midwifery follow-up on the first day, but this was subsequently reduced. Most of the women considered this to be a natural course of events, but one of them had felt that this was difficult. She had been feeling increasingly unwell, but staff had considered her pain to be caused by wind. Two days after being discharged from hospital she was re-admitted with complications. The postnatal personnel had failed to spot the complications, and neither her blood pressure nor her temperature had been measured during her postnatal stay in the maternity ward.
The informants also talked about inadequate follow-up routines, and some of them had been lying for hours without receiving attention after being transferred from the recovery unit. They felt it was difficult to bother healthcare personnel unnecessarily when they were busy. Some had experienced that staff had no time to provide assistance when they rang for help, and they would have liked the midwives to have taken the initiative to look in on them.
The informants felt confused by constantly having to relate to new midwives, and not knowing who was responsible for them. They therefore tried to manage by themselves. A first-time mother who went home after two days described the lack of accessible staff in these terms:
‘Perhaps a slightly greater presence? You shouldn’t have to ask all the time; they should drop by every now and again and make sure that everything is all right. I felt that you were left to your own devices, as it were, and that it’s more difficult to try to grab their attention than if they had dropped by of their own accord and asked how things were. I am positive we didn’t see them at all for a good 24 hours. No-one dropped by.’ (Interview 3)
The importance of knowledge and good information
When the women were informed of what was going to happen, they felt safe, and it was easier for them to be physically active. However, they emphasised that receiving concurring information from different midwives instilled a sense of confidence. One informant explained that she had received information about mobilisation from the physiotherapist. Others missed out on that particular communication because it was the weekend, or because they were otherwise engaged when the physiotherapist called in.
The women were looking for information about how to deal with their operating wound and how to change dressings after returning home, and they felt it was strange that they were expected to take a lot of responsibility for their own medication while they were still on the maternity ward. They were handed a 24-hour dose of medicines and had to request further drugs when the containers were empty. They were asking themselves whether the midwives kept a check on the medication.
One woman had not been told why she was no longer receiving blood-thinning jabs, another reported that staff had forgotten to give her a prescription for drugs that she was meant to continue taking after returning home. When her legs started to swell, she related this to the medication that had been forgotten about and was gripped by a fear of dying.
The caesarean section was entirely unexpected for most of the primiparous women, and they described how they had skipped the chapter on caesarean sections when they were preparing to give birth. Moreover, for several of the women, their stay in the maternity ward was their first encounter with the hospital, and some felt that they existed in a bubble of morphine that made it impossible to take on board the information given. They explained that the healthcare personnel had to repeat everything:
‘It is easy to forget that this may be the only time that someone is in touch with the health service. Perhaps you thought you would be delivering your baby the normal way, and then suddenly they have operated on you. It’s like an extra added bit that you may simply not have the capacity to take in. That you have to get one of those things that the elderly use, a dosette box, or it may have to be made even clearer […] And particularly the things that are supposed to be taken as required. Because you don’t know what you need. The pain. What is normal, and what is not normal? It’s not easy to know.’ (Interview 8)
The value of a partner’s presence
The majority of the women were made to feel safer by the fact that their partner was able to stay overnight with them on the maternity ward. They explained that it was important to them to be together as a couple, since the partner had also been through a lot before the child was born. It was also a comfort that there were two people to remember information provided by staff. Many had a family room at their disposal during parts of their stay and they pointed out that this made it easy to ask the partner for assistance with things they were unable to do themselves, such as moving from one place to another, collecting food, changing nappies and lifting the child.
The women were concerned that their partners ought to be better cared for by postnatal personnel, and one informant explained that her spouse had been made to feel unwelcome when he was collecting food from the canteen. Some had found that when their spouse left the ward, staff expected the women to be able to manage by themselves. For one of the women, this made her stay in the maternity ward so difficult and painful that she chose to go home in order to receive the necessary help.
Not all the women felt a need to be accompanied by someone during their stay in the maternity ward. Some women felt it was unproblematic to ask staff for assistance and considered that they had received the help and respite they needed. However, many accentuated the fact that the assistance provided by their partner was readily available.
Several informants believed that their experience of staying in the maternity ward would have been different if they had been there without their partner, since they felt that their partner had been of greater assistance to them than the ward staff. In the words of one of them:
‘I’m a bit like, I don’t want to be a nuisance. But then I had […]. They told us straight that they had forgotten about us because we were doing so well on our own. But that was only because of my partner. He saw to everything.’ (Interview 6)
Discussion
This study describes the postnatal experiences of ten women following an emergency caesarean section. Our discussions examine these experiences in the light of patient safety theory.
The Norwegian Knowledge Centre for the Health Services defines patient safety in these terms: ‘Protection against unnecessary harm caused as a consequence of health care that the health service has provided or failed to provide’ (19). Severinsson et al. point to the importance of a systematic approach to the development of a patient safety culture, in order to prevent human suffering (20).
Patient safety culture is made up of several subthemes, such as leadership, teamwork, communication and learning, and must be fair, evidence based and patient focused (21). When Currie and Richens investigated how midwives perceive patient safety culture, they found that patient safety may be compromised by pressures to ensure that women are moved swiftly on through the delivery and postnatal wards (22).
Failed to take on board the women’s needs
Our informants explained that they had felt a need for rest, respite and adequate pain relief, but that staff appeared to be more concerned with breastfeeding than with their post-surgical recovery. They explained that it was difficult to lift the child. Similar findings were described in a study conducted by Hillans (23), in which 68 per cent of the women who had undergone an emergency caesarean section felt it was difficult to lift the child and to move around. They did not receive any acknowledgement of these difficulties from the midwives.
It is thought-provoking that neither the midwives nor the women themselves recognised their physical needs. The fact that the surgical procedure is referred to as a caesarean section may cause staff to consider it a less serious procedure than the surgical intervention it is (23). One study showed that after undergoing a caesarean section, women felt that regaining normality was their top priority as they sought to inhabit their new maternal role; concealing their physical needs after the operation is one way of doing this (15).
It is important for midwives to know that women who have delivered by caesarean section sometimes downplay their own complaints. In the interest of patient safety, the midwife needs to focus on the woman – she needs to be patient-oriented. The guidelines on postnatal care (5) do not include a chapter specifically on caesarean sections. They only describe basic postnatal care procedures.
In Norway, the incidence of emergency and elective caesarean sections is rising. In order to safeguard a high standard of follow-up for this patient group, it would therefore, in our view, be useful for the guidelines to include a good description of postnatal care for women who have given birth by caesarean section.
Long periods without receiving attention
The informants described how important it is that postnatal healthcare personnel make themselves accessible and provide good care. They had found that while they received close follow-up on the first day after surgery, the level of attention was then reduced, and they were left to their own devices for long periods. They felt uncomfortable about bothering busy maternity staff, and some felt that healthcare personnel had expected them to manage by themselves when their partner had gone home.
The women who had undergone an emergency caesarean section on a previous occasion were generally happier with the follow-up that they received. Two of the women had received counselling and had drawn up a plan for their postnatal hospital care. Hjälmhult and Økland (14) found that postpartum women received little help or practical support from staff, and that the women felt they were not treated as individuals. Similar findings are described in other studies (24–28).
Our informants explained that they had endured hours without receiving attention from postnatal personnel immediately after transfer from the recovery unit. One informant was even told that the ward was busy, and that the staff had forgotten about her.
According to Thorstensson et al. (25), women were left to their own devices for hours without receiving attention, whether delivery had been vaginal or by caesarean section. This is disconcerting considering the fact that women who have undergone a caesarean section have an elevated risk of complications. At the same time, the rate of birthing women with risk factors is rising (29, 30), which means that there is a general need for better postnatal care.
One of our informants felt increasingly unwell during her postnatal stay in hospital, but neither her blood pressure nor her temperature was measured. She returned home in poor health and was re-admitted after two days due to complications associated with the caesarean section. Complications associated with caesarean sections and surgical deliveries are undesirable incidents that may jeopardise patient safety, particularly when the complications are not identified before discharge from hospital and the follow-up responsibility is left to the woman herself and a potential partner.
The clinical guidelines issued by the National Institute for Health and Care Excellence (NICE) specify that fit and healthy women should be discharged from hospital no earlier than 24 hours after a caesarean section, but that prior to discharge they must be monitored in hospital with a view to complications (7). Postnatal personnel must be available and trained to undertake the required observations.
Good help and support provided by the partner
Studies show that women’s satisfaction with their postnatal stay in hospital increases if their partner can stay with them (26). Our study highlights the partner’s presence as being highly valuable for women who have given birth by caesarean section. Some informants were unable to imagine how they would have coped on the postnatal ward without the assistance of their partner, while others chose to go home to make sure they would receive adequate assistance and respite.
The informants’ descriptions of how important it is to receive help, support and care from their partner gives the impression that the partner’s presence is of great value. Patient safety should be part of the ward culture rather than dependent on the presence of relatives. However, the practical assistance that a relative is able to provide for a new mother who is recovering from surgery is a weighty argument for prioritising family rooms for these couples.
Strengths and weaknesses of the study
All of the authors are midwives with either a masters or doctoral degree on top of many years’ experience of work in delivery and maternity wards, including professional development. One author is still working as a midwife in clinical practice, while two are training midwifery students. Our work experience has impacted on our understanding of the data.
We used semi-structured interviews to gain insight into the women’s experiences (16), combined with thematic cross-case data analysis. This method was useful and pragmatic given our relatively large body of data (16), and the informants talked willingly about their postnatal experiences. This enabled us to collect a rich material that contributed to shedding light on the study’s research question.
Three women had experience of more than one caesarean section. They found it unproblematic to distinguish between the caesarean sections but talked about their experiences in relation to both operations.
The women we recruited contacted us after seeing a social media post shared by midwifery colleagues and others among their personal Facebook networks. The use of social media and snowball sampling (16), i.e. that the informants communicated the information to other potential recruits, meant that the sample was somewhat homogeneous, since all informants were resourceful women with a higher education.
On the other hand, it is a strength of the study that both primiparous and secundiparous women took part. The inclusion of more women with an immigrant background would have strengthened the study’s external validity, as there is a higher risk of emergency caesarean section among immigrant women (30).
Conclusion
The study shows that women who had given birth by emergency caesarean section experienced inadequate care for their physical health after surgery. Although the postnatal women felt no pressure to go home early, several experienced that midwifery help and support was not always available to the extent that they needed it. Some endured long periods without receiving attention, little assistance was forthcoming once their partner had gone home, medicines were forgotten about and complications were overlooked.
There is a need for further research to be carried out on the quality of postnatal care provided in Norwegian hospitals. There is also a need to investigate the consequences of inadequate follow-up after delivery by caesarean section for the mother, the child and the wider family.
References
1. Folkehelseinstituttet. Keisersnitt utført, standardstatistikk. Medisinsk fødselsregister, 2017. Available at: http://statistikkbank.fhi.no/mfr/(downloaded 02.05.2019).
2. Betrán A, Ye J, Moller A-B, Zhang J, Gülmezoglu A, Torloni M. The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLoS One. 2016;11(2):e0148343. DOI: 10.1371/journal.pone.0148343.
3. Venheim MA, Reinar LM. Barselomsorg. In: Brunstad A, Tegnander E, eds. Jordmorboka. Oslo: Akribe; 2010. p. 535–46.
4. Meld. St. nr. 12. (2008–2009). En gledelig begivenhet : om en sammenhengende svangerskaps-, fødsels- og barselomsorg. Oslo: Helse- og omsorgsdepartement; 2009.
5. Helsedirektoratet. Nasjonal retningslinje for barselomsorgen – Nytt liv og trygg barseltid for familien. Oslo; 2013.
6. Sjetne IS, Holmboe O. Brukererfaringer med fødsels- og barselomsorgen i 2016 (PasOpp-rapporter), Folkehelseinstituttet. PasOpp-rapport December 2017. Available at: https://www.fhi.no/globalassets/dokumenterfiler/rapporter/pasopp/2017/fodsel-og-barsel/brukererfaringer-med-fodsels--og-barselomsorgen-i-2016.-nasjonale-resultater.pdf(downloaded 21.06.2018).
7. NICE – National Institute for Health and Care Excellence. Care after caesarean section. 2012. Available at: https://pathways.nice.org.uk/pathways/caesarean-section#path=view%3A/pathways/caesarean-section/care-after-caesarean-section.xml&content=view-node%3Anodes-care-of-the-woman(downloaded 20.06.2018).
8. Declercq JE, Barger RM, Cabral JH, Evans JS, Kotelchuck JM, Simon JC, et al. Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstetrics & Gynecology. 2007;109(3):669–77.
9. Borders N. After the afterbirth: a critical review of postpartum health relative to method of delivery. Journal of Midwifery & Women's Health. 2006;51(4):242–8.
10. Armson BA. Is planned cesarean childbirth a safe alternative? CMAJ: Canadian Medical Association Journal. 2007;176(4):475–6.
11. Petrou S, Kim SW, McParland P, Boyle EM. Mode of delivery and long-term health-related quality-of-life outcomes: a prospective population-based study. Birth. 2016;44(2): 110–9.
12. Barimani M, Oxelmark L, Johansson SE, Langius-Eklof A, Hylander I. Professional support and emergency visits during the first 2 weeks postpartum. Scandinavian Journal of Caring Sciences. 2014;28(1):57–65.
13. Fahey JO, Shenassa E. Understanding and meeting the needs of women in the postpartum period: the perinatal maternal health promotion model. Journal of Midwifery & Women’s Health. 2013;58(6):613–21.
14. Hjälmhult E, Økland T. Hva barselkvinner er opptatt av den første tiden hjemme med en nyfødt. Sykepleien Forskning. 2012;7(3):224-30. DOI:
10.4220/sykepleienf.2012.0128.
15. Fenwick S, Holloway I, Alexander J. Achieving normality: The key to status passage to motherhood after a caesarean section. Midwifery. 2009;25(5):554–63.
16. Malterud K. Kvalitative forskningsmetoder for medisin og helsefag. 4. ed. Oslo: Universitetsforlaget; 2017.
17. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 3. ed. Oslo: Gyldendal Akademisk; 2015.
18. WMA, World Medical Association. Helsinkideklarasjonen 2013. Available at: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/(Nedlastet 20.06.2018).
19. Helsedirektoratet. Pasientskader i Norge [Internet]. Oslo: Helsedirektoratet; 2012 [updated 29.01.2019, cited 15.01.2019]. Available at: http://www.pasientsikkerhetsprogrammet.no/om-oss/om-pasientsikkerhetsprogrammet/pasientskader-i-norge.
20. Severinsson IE, Haruna M, Rönnerhag M, Berggren I. Patient safety, adverse healthcare events and near-misses in obstetric care – a systematic literature review. Open Journal of Nursing. 2015;5:1110–22.
21. Sammer CE, Lykens K, Singh KP, Mains DA, Lackan NA. What is patient safety culture? A review of the literature. Journal of Nursing Scholarship. 2010;42(2):156–65.
22. Currie L, Richens Y. Exploring the perceptions of midwifery staff about safety culture. British Journal of Midwifery. 2009;17(12):783–90.
23. Hillan EM. Issues in the delivery of midwifery care. Journal of Advanced Nursing. 1992;17(3):274–8.
24. Ellberg L, Högberg U, Lindh V. ‘We feel like one, they see us as two’: new parents’ discontent with postnatal care. Midwifery. 2010;26(4):463–8.
25. Thorstensson S, Andersson A, Israelsson S, Ekström A, Wahn EH. To build a bridge between two worlds: Mothers' experiences of professional support at the maternity ward. Health Care for Women International. 2016;37(10):1067–81.
26. Barimani M, Vikstrom A. Successful early postpartum support linked to management, informational, and relational continuity. Midwifery. 2015;31(8):811–7.
27. Hildingsson IM, Sandin-Bojö A-K. ‘What is could indeed be better’ – Swedish women’s perceptions of early postnatal care. Midwifery. 2011;27(5):737–44.
28. Fenwick J, Butt J, Dhaliwal S, Hauck Y, Schmied V. Western Australian women's perceptions of the style and quality of midwifery postnatal care in hospital and at home. Women and Birth. 2010;23(1):10–21.
29. Folkehelseinstituttet. Fakta om fruktbarhet, fødsealder og helse. Oslo: Folkehelseinstituttet; 2016. Available at: https://www.fhi.no/fp/gravide-og-fodende-kvinners-helse/fruktbarhet-fodealder-og-helse---fa/(downloaded 02.05.2019).
30. Sorbye IK, Daltveit AK, Sundby J, Stoltenberg C, Vangen S. Caesarean section by immigrants' length of residence in Norway: a population-based study. European Journal of Public Health. 2015;25(1):78–84.










Comments