No increase in in-patient detoxification completion rates following pre-hospital telephone intervention
Despite staff calling patients prior to the admission date, the proportion who presented for treatment did not increase. Nevertheless, it was a useful exercise for exchanging information and building relations.
Background: The number of patients who fail to present for planned substance abuse treatment or drop out of such treatment is a major challenge.
Objective: The objective of our study was to investigate whether a pre-hospital telephone intervention could increase the admission and completion rates for in-patient detoxification treatment. We also wanted to gain an insight into the experiences that those making the phone calls had with the intervention.
Method: We used a quantitative data collection method in order to compare a period without a telephone intervention to a period with a telephone intervention. The qualitative data we collected provided an insight into the experiences of the staff who made the phone calls. The study was conducted in the Addiction Unit at Sørlandet Hospital Trust.
Results: The telephone intervention led to a modest and non-significant 6% increase in the admission rate. There was no increase in the treatment completion rate. The intervention was viewed in a positive light by the staff who conducted the phone calls because they led to clarification and the exchange of information, and served as a starting point for relationship building.
Conclusion: Despite the fact that the intervention did not lead to significant changes in the admission and completion rates for detoxification treatment, it was nevertheless viewed as an aid for increasing the flow of information and for facilitating the service.
The drop-out rate in interdisciplinary substance abuse treatment is a major challenge. The proportion who do not complete such treatment varies from 10 to 60%, depending on the level of treatment and population surveyed (1). Treatment drop-out has been associated with, inter alia, a higher risk of relapse, multiple readmissions and poorer physical and mental health compared to those who complete their treatment (2).
In addition to treatment drop-out, failure to present for treatment is also a problem. Auspicious measures aimed at reducing drop-out rates and increasing uptake are as follows: clarifying expectations at an early stage of the treatment phase, strengthening patient relations or treatment alliance, and helping patients to muster the desire to attend, for example by providing practical information about the treatment (1).
Research in the field
Numerous international studies examine out-patient attendance rates at mental health services. A systematic review from 2014 distinguishes between a ‘simple reminder’, such as a text message, and a ‘reminder plus’, which can take the form of a personal phone call (3).
In summary, these studies showed promising results, and the simple reminder was recommended for use as a regular measure. The reminder plus was sometimes more effective than the simple reminder at reducing non-attendance, and was considered to be particularly useful for first appointments. Simple reminders were recommended for subsequent appointments.
There are considerably fewer studies on uptake of institutional treatment. A PubMed search for research articles written in English within the field of substance abuse using the search string ‘(substance related disorders[MeSH Major Topic]) AND ((((detoxification[Title/Abstract]) AND telephone[Title/Abstract])) OR pre-hospital[Title/Abstract])’ gave 35 matches. A keyword search for ‘substance related disorders’ and ‘reminder systems’ gave 13 new matches.
Only one was relevant: a pilot study that included 80 patients referred for admission to an in-patient unit. The findings showed that the admission rate was not significantly higher for the group who had been called in advance, and that the drop-out rate had not been reduced (4). More large-scale experimental studies are needed into pre-hospital reminder interventions.
Objective of the study
The objective of this study was two-fold. First, we wanted to investigate whether a pre-hospital telephone intervention could increase the admission and completion rates for in-patient detoxification treatment. In addition, we wanted to gain an insight into the experiences that those making the phone calls had with the intervention.
Method
We collected quantitative data in order to investigate the effect of a pre-hospital telephone intervention in addition to qualitative data with a view to gaining an insight into the experiences of those who performed the intervention. The study was conducted at the detoxification units in the Addiction Unit at Sørlandet Hospital Trust, located in Kristiansand and Arendal.
The catchment area for the units is mainly the counties of Aust- and Vest-Agder. There are 24 beds equally distributed between the units. On average, there are approximately 10 planned admissions per week at each of the units. Both units offer medical detoxification and clarification of motivation for further treatment.
Quantitative part of the study
A quasi-experimental (off-on) design was used to compare a period without a telephone intervention to a period with a telephone intervention (5). In the first phase, none of the participants were called prior to the planned admission. This period lasted for twelve weeks. We recorded demographic data, such as age and gender, and noted whether the patient had presented for treatment or not, as well as reasons for non-attendance – whether they had notified the unit or not – and whether the treatment was completed.
In the second phase, a pre-hospital telephone intervention was carried out. The duration of this phase was similar to the first phase. Attempts were made to call all patients referred for planned in-patient treatment at the detoxification unit during the week before the admission date. The same person in each unit made the calls on the same day every week.
A total of three staff members were involved in calling the patients. The intervention was intended to serve as an appointment reminder, and to clarify whether the patients had received the appointment letter and were ready to be admitted. In addition, we believed that the telephone intervention may be a good starting point for relationship building.
According to the informants, the biggest challenge was trying to establish contact with the patients. Some of the patients had new phone numbers that had not been recorded in the patient journals. Others did not answer their phone. The informants estimated that they managed to contact about half of the relevant patients. This was in line with the data in the quantitative part of the study.
Prior to the telephone intervention, the staff prepared themselves by reading the referrals and assessment notes. If their initial attempt to contact a patient was unsuccessful, they tried again. If they failed to established contact on the second attempt, they sought information on how to reach the patient by contacting collaborating partners and/or family members with whom the patient was in contact according to their journal.
The phone calls were logged. The staff recorded the outcome of the intervention: if they had established contact, if the patient had declined the offer of treatment, if the patient wanted up to a one-week deferral or if the patient had said that he/she would present for treatment. In the study, ‘failure to present for treatment/non-attendance’ was defined as when a patient did not meet up at the agreed time or by 2pm on the day of admission without giving advance notification.
We defined treatment drop-out as discontinued treatment, i.e. where the patient left the unit or chose to terminate the treatment before the agreed end date, contrary to the unit’s recommendation. In the quantitative analysis, we compared data on admission rates in the first phase with the period when the telephone intervention was carried out. We used a cross-tabulation analysis and chi-square test. For the analysis, we used the statistics software IBM SPSS version 21.
Qualitative part of the study
In order to describe the staff’s experiences with the intervention, we asked those who conducted the phone calls to take part in an interview, and all three agreed. The first author conducted the interviews. We used a semi-structured interview guide devised for the purpose (6).
The topics covered in the interviews were as follows: the content of the phone conversations, the patients’ responses, time spent on the intervention, the informants’ thoughts on the potential benefits of conducting such an intervention, the informants’ experiences with the calls, the challenges of the intervention and suggestions for possible improvements. Each interview lasted approximately one hour.
The first author took notes during the interviews, which she then typed into the computer. We presented a print-out of the notes to the informants and asked them to read these and make corrections if necessary. We anonymised the informants to ensure that it was not possible to know who had said what.
The interviews were analysed using the systemic text condensation method; they were read, coded and sorted, and reviewed again (7). Texts with the same content were conflated and condensed. We then reviewed the text to establish whether the themes and the condensed text under each theme gave a valid description of the context from which it was derived.
Ethical considerations
We sent the study for evaluation to the Regional Committees for Medical and Health Research Ethics (REC) (reference number 2014/1611). They considered the study to be a quality investigation, and as such was not subject to their approval. We did not, therefore, obtain individual consent from the patients. The staff who were interviewed signed a declaration of consent. The study was approved by the Norwegian Centre for Research Data (NSD) (reference number 40167).
Results
Quantitative findings
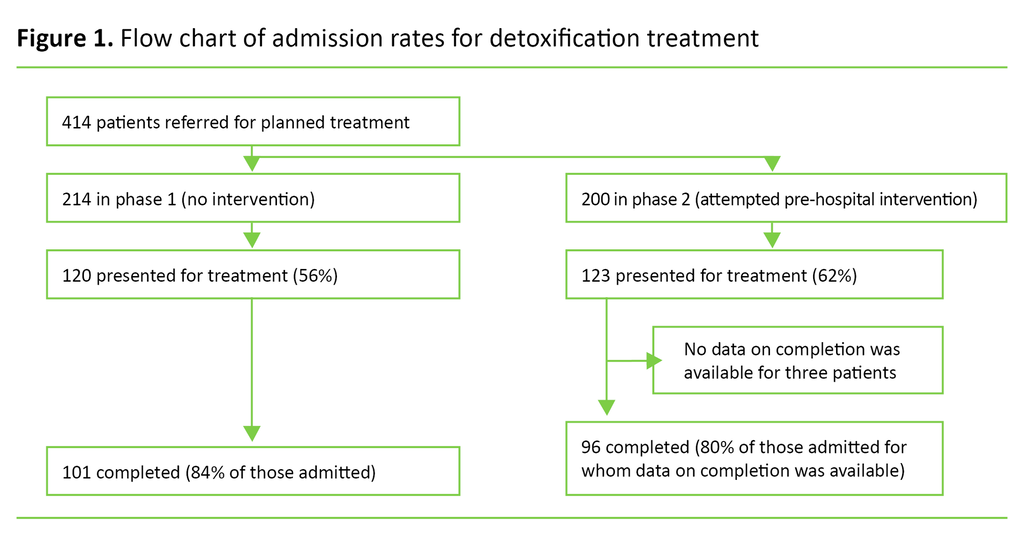
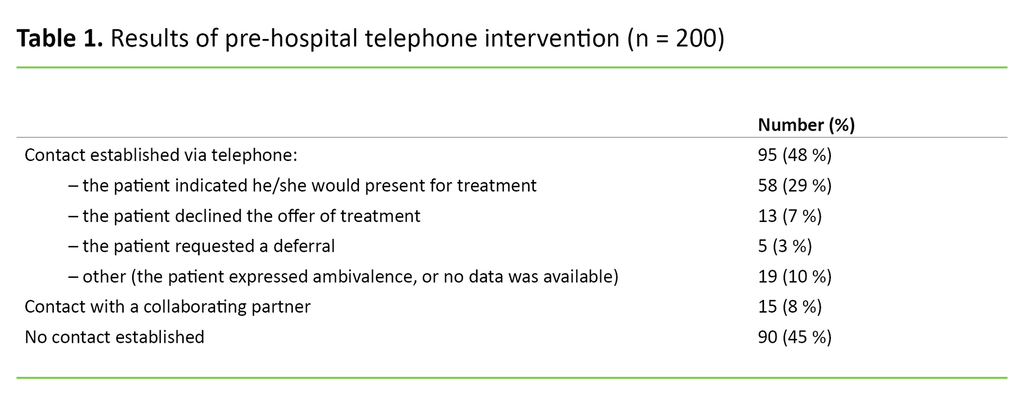
In total, we included 414 patients in the study. Of these, 125 (30%) were women, and the mean age was 38 years (standard deviation (SD) = 13). We included 214 in the first phase without a telephone intervention, and 200 in the second phase with a telephone intervention (Figure 1). In the intervention phase, the informants managed to contact 48% of the patients (Table 1).
A total of 13 (7%) patients declined the offer of treatment: ten because they did not want it, and three because they had received and accepted another offer or did not need detoxification. Five patients (3%) received a deferral. In total, 10% of the patients with an admission date provided the informants with information that formed the basis for logistical changes in the intake (Table 1).
When we compared the phases, 120 (56%) of patients presented for treatment at the unit in the phase without a telephone intervention, while the corresponding figure for the phase with a telephone intervention was 123 (62%) (Figure 1). Overall, 41% did not present for treatment. The higher figure by 6 percentage points in the intervention phase was not significant (χ2 = 1.3, p = 0.26).
No data was available on the completion of treatment for three of the 243 patients who presented for treatment, and these were therefore excluded from further analysis. A total of 43 (18%) patients did not complete their treatment. The completion rate in the two phases was 84% and 80% (Figure 1) in phase 1 and phase 2 respectively (χ2 = 0.71, p = 0.40).
Qualitative findings
The informants reported that the phone calls lasted an average of five minutes, and the longest call was twelve minutes long. They were unsure whether the intervention helped increase the admission and completion rates for the detoxification treatment.
Furthermore, the informants had the impression that most people they spoke to on the phone had already made a decision, and that the intervention did not alter this choice. Nevertheless, the informants believed that the patients found the conversations to be helpful.
Relationship building
The informants felt that the phone calls were useful as a starting point for building relations prior to admission. They qualified this by explaining that their experiences with conducting the intervention had been purely positive. Many of the patients also gave the impression that they appreciated the intervention.
When the patients who had spoken to the informants on the phone presented for treatment, the patients were able to remember the phone conversations:
‘When the patients I called arrived for treatment, I sometimes said hello and commented that we had spoken on the phone earlier. The patients then often remembered our conversation and I felt that contact had already been established.’
Clarifications
The informants believed that the intervention helped to clarify a number of points. The conversations established whether the patients had received the offer of detoxification and whether they planned to present for treatment. Most of the patients who said they would attend did in fact do so. Some of the patients that informants contacted were not aware that they had been offered detoxification treatment, partly because they had changed their address and had not received the letter.
Other patients asked for the treatment to be deferred, and this was normally granted. The informants were notified several times that the patient they were trying to contact had either already been admitted to another department or had started detoxification with a different follow-up method or on their own. During the phone calls, several practical matters and expectations relating to the patient’s stay at the unit were also clarified.
Some of the patients had negative ideas about the detoxification, and the informants then informed them that the conditions were better than the patients feared, for example, patients have their own rooms in the units.
Other practical issues that could be clarified were how long they would remain at the unit and whether it was possible to arrive later in the day than the time specified. The informants also provided information about the unit’s routines and location, transport to the unit and the staff’s attitude to the use of drugs and medication during treatment.
During the phone call, some patients expressed ambivalence towards the treatment. The informants then tried to adopt a supportive manner:
‘If the patient I’m calling has mixed feelings about the treatment, I make it clear that the offer still stands and that they are welcome if they decide to go ahead. I also tell them that the unit wishes to be informed about their choice the day before admission. Most people then call and let us know by the deadline.’
The informants believed that providing clarification helped prepare the patients for their stay at the unit and strengthened the patients’ sense of coping:
‘Some of the younger patients in particular who are referred for detoxification for a drug use disorder feel afraid and insecure, and may therefore need confirmation and reassurance that they are expected. The information provided can make it easier for them to form a picture of their stay at the unit, and what awaits them.’
Receiving information about the patients
The informants reported that when preparing for the intervention and calling the patients they received some information about them that they would not otherwise have received. This information was useful for informants as well as the rest of the unit:
‘I’m often asked by the others, and especially the doctors in the unit, if I’ve had contact with the patients being admitted and if there was anything in particular that came to light during the conversation that could have a bearing on their stay at the unit.’
The content of the calls was recorded in the patient journals, which provided the admission staff in the unit with clarification and information about whether the patients were available.
The unit found the information a useful aid in the planning of admissions and bed availability. Where patients declined the offer, the units could offer the space to others who had been referred, or use the space for acute admissions. This led to greater predictability in terms of intake and improved the logistics in the units.
Challenges
In cases where the informants did not manage to establish contact with the patient or the collaborating partner that issued the referral, the informants were unsure whether it was appropriate to contact the patient’s family. They feared creating a dilemma if it transpired that the patient’s family was unaware of the referral. In addition, the informants wondered if they would undermine the good preparatory work carried out by the community-based services:
‘The system is extensive, and the patients come across a large number of people each with their own opinions.’
This was especially true in cases where they had read before the intervention that the person they were calling was ambivalent to being treated at the unit. They resolved this by treading carefully and not trying to provoke a decision that the patient was not ready to make.
Discussion
Telephone contact with patients prior to treatment did not significantly increase the proportion who presented for detoxification, and nor did the treatment completion rate increase. The staff who conducted the intervention generally perceived the measure as positive: the phone call enabled them to establish a starting point for relationship building, and to provide and receive information and clarify various points.
The informants reported several challenges, such as whether they would be breaching confidentiality by calling the family of patients they had not managed to contact, and whether their conversation with the patient could undermine the good preparatory work carried out by the community-based services.
Many did not present for treatment
Forty-one per cent of the patients did not present for treatment. The corresponding figures from two detoxification units at the University Hospital of North Norway show a non-attendance rate of 33 and 30% respectively (8). The high proportion of patients who failed to present for treatment shows that the topic of our study is highly relevant.
Our study covered a larger number of respondents than an earlier pilot study, but the findings were similar: there was no clear evidence that a telephone intervention was an effective measure for ensuring that patients presented for treatment (4). The informants were of the opinion that the patients had largely made up their minds beforehand, and that the phone call did not change their position.
Despite the fact that the intervention did not increase the admission rate, earlier studies have shown that patients missed out on some of the benefits that the informants believe the patients gained from the telephone intervention. For example, a national survey estimates that half of the in-patients undergoing interdisciplinary substance abuse treatment had not received satisfactory information about the treatment they were to receive (9).
A survey conducted at the Addiction Unit also showed that there were challenges linked to patients not receiving adequate information (10). Receiving information on an ongoing basis was crucial to patients being able to have a say in their treatment and making optimal choices (11).
The informants also found that the telephone intervention provided them with supplementary information about the patients, which was useful for optimum facilitation of the patient’s stay at the unit. Good knowledge of patients is essential to providing appropriate treatment that is adapted to the individual patient’s needs (12). The intervention can therefore help to ensure that patients and staff receive the necessary information.
Contacting the patient is recommended
Earlier studies recommend that a ‘reminder plus’ is given for first-time admissions to an in-patient unit, i.e. that the patient is contacted (3). In our study, the informants reported that even the patients who had been in hospital before had questions. The intervention also meant that intake planning could be more systematic and considered.
The biggest challenge was getting hold of the patients; only half could be reached. In order to establish contact with more patients, efforts could be made to call them in the evening, and not just during the day as in this project. One suggestion that could have improved the relationship-building aspect of the intervention is for the person admitting the patient at the unit to also call the patient.
Resource use for the intervention seemed to be reasonable: a rough estimate shows a full-time equivalent of 0.15 for each unit. After the study was completed, the staff wondered if they should continue the intervention as it had positive secondary consequences, but did not give the desired increase in admission or completion rates. A reminder by text could be an option.
Such reminders are standard practice for out-patient consultations, but only for second and subsequent appointments after it has been clarified if the patient wants such reminders and their phone number has been verified. We therefore considered text reminders to be unsuitable for in-patients.
One of the units in our study continued with a systematic telephone intervention. Each unit should conduct a cost-benefit analysis to assess whether it is worth using resources on such a measure. The benefits that were identified in the qualitative findings should also be included in this analysis.
Strengths and weaknesses of the study
The strength of the quantitative part of the study was that we systematically compared two periods with and without an intervention and had a relatively large sample of patients. In order to make the intervention manageable for the staff, we needed to use a quasi-experimental design instead of randomisation.
There were few informants in the qualitative part of the study. We only selected the staff who had actually conducted the phone calls because they were in the best position to comment on the practice employed. In terms of further development of the intervention, it would have been useful to explore the patients’ own experiences and perceptions of the telephone contact: what they considered to be useful about the intervention and what can be improved.
Conclusion
A pre-hospital telephone intervention did not lead to any significant increase in the admission or completion rates for detoxification treatment, and these findings cannot therefore justify the use of resources.
The staff nevertheless found that the intervention was useful and positive because it led to clarification, the exchange of information and established a starting point for relationship building. We can thus view the intervention as a way of meeting the health authorities’ requirement for patients to receive more information about the service and for the service to be better adapted to the individual patient.
References
1. Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev. 2013;33(8):1010–24.
2. Stark MJ. Dropping out of substance abuse treatment: A clinically oriented review. Clin Psychol Rev. 1992;12(1):93–116.
3. McLean S, Gee M, Booth A, Salway S, Nancarrow S, Cobb M, et al. Targeting the Use of Reminders and Notifications for Uptake by Populations (TURNUP): a systematic review and evidence synthesis. Health Services and Delivery Research. 2014;2(34).
4. Gariti P, Alterman AI, Holub-Beyer E, Volpicelli JR, Prentice N, O'Brien CP. Effects of an appointment reminder call on patient show rates. J Subst Abuse Treat. 1995;12(3):207–12.
5. Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Boston: Houghton Mifflin; 2002.
6. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 2. ed. Oslo: Gyldendal Akademisk; 2009.
7. Malterud K. Kvalitative metoder i medisinsk forskning : en innføring. 2. ed. Oslo: Universitetsforlaget; 2003.
8. Brox H, Eilertsen MK, Hårvik V, Jakobsen T. Kartlegging av pasienter som avbryter eller ikke møter til rusbehandling ved Psykisk helse- og rusklinikken, UNN HF. Delrapport 1 fra prosjekt «Hindre drop-out fra rusbehandling» ved Psykisk helse- og rusklinikken. Tromsø: Universitetssykehuset Nord-Norge; 2016.
9. Haugum M, Holmboe O, Iversen HH, Bjertnæs ØA. Pasienterfaringer med døgnopphold innen tverrfaglig spesialisert rusbehandling (TSB). Resultater etter en nasjonal undersøkelse i 2015. Oslo: Kunnskapssenteret; 2016.
10. Gallefoss L, Årseth AL. Drop-out prosjektet. Delrapport 2: Pasientforløp og drop- out i overgang fra Avd. for rus- og avhengighetsbehandling (ARA) Sørlandet Sykehus HF til videre behandling i private døgninstitusjoner. Kristiansand: ARAs forskningsserie; 2016.
11. Helsedirektoratet. Veileder om rehabilitering, habilitering, individuell plan og koordinator. Oslo: Helsedirektoratet; 2015. Available at: https://helsedirektoratet.no/retningslinjer/rehabilitering-habilitering-individuell-plan-og-koordinator(downloaded 09.05.2018).
12. Helse- og omsorgsdepartementet. Opptrappingsplanen for rusfeltet (2016–2020). Prop. 15 S (2015–2016). Oslo: Helse- og omsorgsdepartementet; 2015.










Comments