Nutritional status assessment – a professional responsibility in community nursing
It is challenging for community nurses to screen their patients’ nutritional risk because the guidelines fail to take sufficient account of the domestic arena.
Background: According to the recommendations set out in the Norwegian Guidelines for Prevention and Treatment of Malnutrition, community nurses must assess their patients’ nutritional risk at the time of admission or registration with the health service, and regularly every month thereafter.
Purpose: To investigate how community nurses interpret and uphold sound professional practice with respect to the requirements set out in the Norwegian Guidelines for Prevention and Treatment of Malnutrition.
Method: A qualitative study involving analysis of data from two practice development projects. The incremental analysis identified meaning units, sub-themes and themes (32). Four themes were identified and categorised from across the body of material. The data include twelve group interviews with nineteen nurses employed by two different local authorities.
Results: Management support is important for the implementation of systematic nutritional screening. The nurses suggested that their familiarity with the patients and their nutritional needs is an important factor with respect to organising the practical arrangements in the home. The nurses felt it was challenging to assess the patient’s intake of food and drink around the clock. They found themselves in the field of tension between preserving the home dweller’s autonomy, complying with the recommendations for systematic nutritional screening and coping with pressures of time.
Conclusion: Nutritional care is a person-centred, practical approach adjusted to the domestic arena. The community nurses ask whether the requirements of the professional guidelines take sufficient account of the home-based context. Close cooperation between managers and staff is required for systematic assessment of nutritional risk to be achieved within the constraints imposed by existing resources.
Elderly home dwelling patients who suffer from multiple diseases, oral or dental problems, or who take multiple drugs may have reduced awareness of hunger and thirst. These problems may be underlying causes of malnutrition (1–3). Social isolation, depression and cognitive failure may also represent underlying risk factors of malnutrition (4–6). Norwegian and international studies have shown that the home-dwelling elderly are at risk of malnutrition (7–13). A number of studies point out that health care personnel have inadequate routines for, and insufficient knowledge of, the systematic recording of patients at risk of malnutrition (8, 14–16).
As early as in 2003, the European Society for Clinical Nutrition (ESPEN) recommended the use of standardised screening tools for assessing nutritional risk (17). In 2009, the Norwegian Directorate of Health recommended the use of such tools in the Norwegian Professional Guidelines for Prevention and Treatment of Malnutrition (18). The guidelines imposed a duty on the primary health service to carry out an assessment of nutritional risk on admission or registration with the service, and monthly thereafter unless there are medical factors that indicate otherwise (18).
Guidelines may serve as a catalyst
It is often a long and complicated incremental process to implement guidelines based on research-based knowledge in the healthcare services (19, 20). Nurses and managers in the primary health service must be given an opportunity to familiarise themselves with the knowledge base, how the guidelines may be interpreted and how they may benefit patients. They also need to reach agreement on how to incorporate the professional guidelines in the organisation’s local routines. At the same time, it is important that nurses become aware of and can account for their own understanding of what is important and reasonable nutritional practice. They must also have the opportunity to discuss different points of view with patients and their relatives (21).
In other words, this is not a linear or technical process through which synthesised knowledge from research is transferred to practical actions. The guidelines may nevertheless serve as a catalyst that promotes knowledge-based clinical decisions in practice (20). McCormack and McCance (22) therefore maintain that the sharing of experiences is a basic requirement for practice development. Reflective group discussions on a focused theme may also form the starting point for participant and action oriented research collaborations (23–25). This type of research approach lends itself to involving several groups that follow their own discussion process, and then subject the resultant material to an analysis of the same theme (26).
The purpose of this study was to investigate the ways in which community nurses interpret and uphold professionally sound nutritional practice in accordance with the requirements set out in the Norwegian Guidelines for Prevention and Treatment of Malnutrition (18).
Method
The study is based on and analyses qualitative data gathered through two practice development projects in which community nurses were asked to explore their own practices in relation to nutritional care. The study was carried out in two Norwegian municipalities, studies A and B, each with a population of approximately 20 000 (27, 28). The focus theme was the nutritional care provided by the community nurses and their respective interpretations of the requirements set out in the national guidelines for the profession. In study A the exploration of the community nurses’ nutritional practice was particularly focused on their use of a specific screening tool: the Nutrition Journal (Ernæringsjournalen). Data were analysed across the two projects in order to provide new insights, if possible, and involve new concepts (26).
Sample
We asked the managers of the community nursing services in the two municipalities to recruit nurses for participation in the practice development projects. They assisted with recruitment by issuing an information letter to their nurses. The inclusion criterion for study A was a full time work equivalent of 75 per cent. Five nurses gave their consent to participating in study A, while 14 nurses gave their consent to participating in study B. Two of the participants in study B were nursing supervisors. In total, 19 nurses agreed to take part, all of whom worked a full time equivalent of 75 per cent or more.
Data collection
The data collection method in both projects was cyclical, involving experience exchanges, critical reflection and practical problem solving (29). Participants attended a number of meetings to explore a focus theme (26). The researchers in studies A and B made use of thematic interview guides with open-ended questions adapted to the focus theme. Participants were given an opportunity to voice their experiences and to give practical examples of their nutritional work.
The researchers conducting studies A and B encouraged participants to talk and reflect between themselves without exerting control (30). If anything was unclear or required further elaboration, the researchers would ask follow-up questions along the way. By utilizing multiple meetings and an explorative reflective approach, a number of different views, basic values and practice improvement proposals were put forward (25, 26). The third author was the research supervisor for both projects and a participant moderator in study B.
We collected data over a six-month period from three groups of participants: one group of five nurses under study A and two groups under study B – one with nine (B1) and one with five (B2) participant nurses. Each group met on four occasions. The body of data consists of the researchers’ transcribed recordings of twelve group discussions, four from each group. The study A group of participants retained the same members throughout. In study B, the groups were open and new participants joined along the way, challenging the group consensus with questions and alternative views. The researchers drafted a summary note of each meeting. The note was approved by the participants at the start of the next meeting. Themes for further exploration were carried forward to the next theme guide. This procedure strengthens the participants’ involvement with the knowledge process and the studies’ communicative validity (31).
Analysis
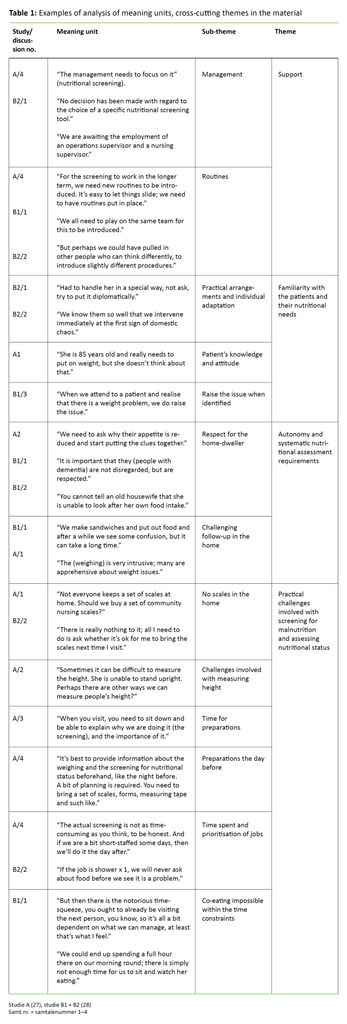
This study provides an analysis of the content of the twelve group discussions as well as the researchers’ reflections in retrospect on the possibilities and challenges encountered by the community nurses as they carry out their nutritional work. All authors studied the results of the two earlier projects. The qualitative content analysis was incremental, inspired by Graneheim and Lundman (32). As we identified meaning units, sub-themes and themes, we looked for patterns and categories across the material (table 1). When encoding the material we put emphasis on accommodating the community nurses’ different views (30). Our result chapter includes a number of quotes that highlight the participants’ different experiences.
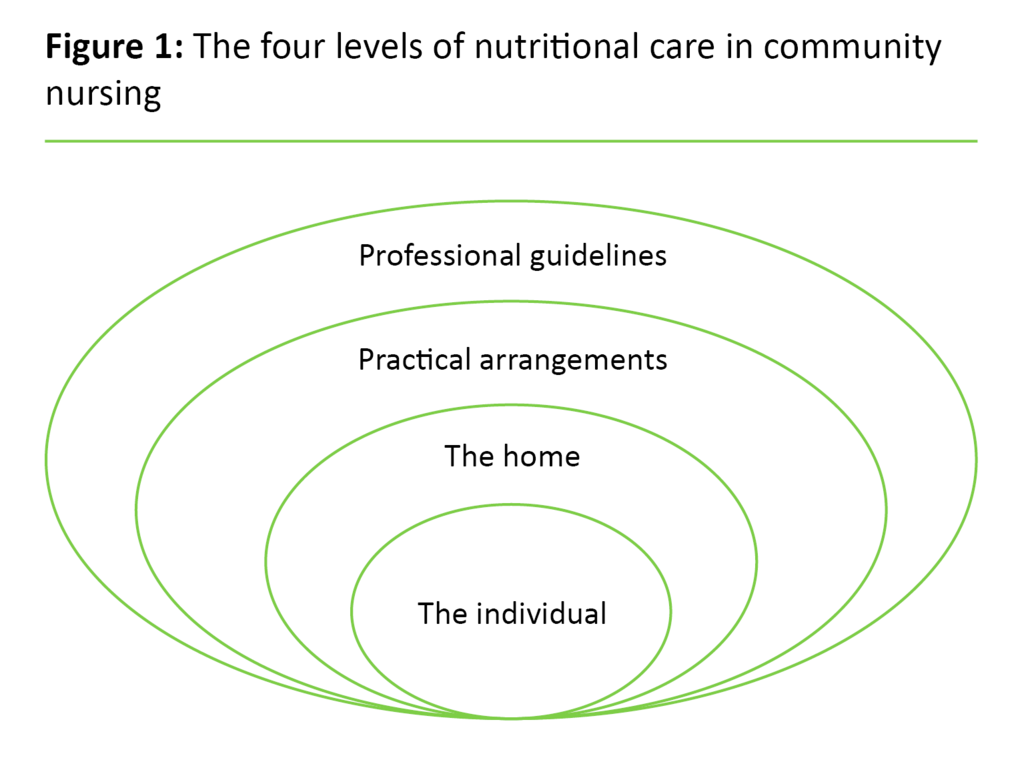
The last analytic step involved an overall interpretation of the data material seen in the light of the study’s purpose as well as earlier research. This process saw the emergence of new dimensions and understandings of the community nurses’ nutritional work. These factors are presented in our discussion chapter, and they are also illustrated in figure 1 (see below). The discussion chapter further includes a critical assessment of the validity of the analyses.
Ethical considerations
The Data Protection Official for Research (NSD) considered studies A and B separately and gave their approval of both. All participants have given their informed consent in writing. Participation was voluntary and took place during working hours. According to the NSD, this study did not require further consideration and approval.
Results
The results are presented under four themes that were identified through our analyses of all the data: 1) support, 2) familiarity with the patients and their nutritional needs, 3) patient autonomy and the requirements relating to systematic nutritional assessment, and 4) practical challenges in providing nutritional care.
Support
The nurses were agreed that for systematic nutritional screening to be implemented, the support of the local authorities was required, as well as that of the management of the community nursing service. The managers must have an interest in and awareness of the theme: “The management needs to focus on it.” Nutritional screening must be integral to the organisation and routines must be implemented, both for staff who make decisions about the provision of care services in the home, and for the providers of such care, or in the words of the nurses: “It’s easy to let things slide; we need to have routine put in place.”
In study A, the local authority had decided on the Nutrition Journal as their chosen screening tool. In study B, the local authority had yet to choose a specific nutritional screening tool. Participants in this study found it problematic that this indecision prevented them from implementing a nutritional screening tool.
Familiarity with the patients and their nutritional needs
The community nurses described the practical facilitation of meals in various patient situations as being significant. Several of them reported that they talked to their patients about what they had eaten on a daily basis, and about what they had in their fridge. The nurses emphasised that they were well acquainted with the patients and that they intervened as and when required: “We know them so well that we intervene straight away when the home becomes chaotic.” The nurses felt it was most important to prioritise the assessment of nutritional risk in the sickest patients, and in those who had lost considerable weight.
The nurses discussed the definition of “malnutrition”. They said as follows: “We talk to them about not eating very much; we never say that they are malnourished.” A joint read-through of the national professional guidelines gave the nurses new understanding that malnourishment is the mismatch between the patient’s needs and their actual intake: “We knew that nutrition was important, but now we think more broadly.”
The nurses strengthened their professional involvement with nutrition and local knowledge through group discussions. The nurses passed on this local knowledge through reports, in staff meetings and by providing guidance: “When the assistants say: ʻHe’s so skinny’, I explain that this means we need to keep records, you see.”
Patient autonomy and the requirements for systematic nutritional assessment
The nurses stressed their own respect for the home-dwellers’ autonomy. They put particular emphasis on the domestic arena as a private space and on behaving in ways they assumed to be appropriate in the patient’s own home. Some of the nurses felt it was inappropriate to weigh the patient, because this might affect the patient’s dignity and autonomy.
During group reflection sessions it emerged that the patients themselves were reluctant to step onto the scales, and this could influence the nurses so that they skipped the weighing. Others were worried about offending the elderly women’s “pride as a housewife”: “You can’t tell an old housewife that she is unable to look after her own food intake.” During the professional reflective sessions the nurses asked questions such as: “Is it natural for them not to want to eat that much any longer?” and “Should they be allowed to choose for themselves?”
The nurses felt it was challenging to keep track of the home-dwellers’ actual intake of food and drink. They were particularly concerned about dementia sufferers who forget to eat or drink, and felt it could be difficult to follow up with systematic recording: “We never make use of drink lists, as they might be drinking when we’re not around. They live at home, after all, so there is no point.”
Practical challenges associated with providing nutritional care
The nurses discussed how they could best prepare the patients for the nutritional screening. They felt it was best to provide information about the weighing and screening for nutritional status beforehand, for instance the evening before: “A bit of planning is required. You need to bring a set of scales, forms, measuring tape and such like.” Nurses who agreed a suitable time for the weighing with the patient, were positively received: “He’s been waiting for me with those scales, you know.”
Nurses who suggested and carried out the weight check were surprised by the patients’ positive response: “I think the service users felt it was a positive thing; that it was a sign that we cared.” This motivated the nurses to raise questions about weighing with more patients. They found that systematic nutritional screening could be carried out in connection with other jobs. Relatives expressed that they were grateful for the screening. They were also grateful that professional attention was given to insufficient food intake and weight loss.
Because the nurses found that many had no scales in their own home, the community nursing service purchased several simple sets of scales. If the patient was unable to stand, there were practical challenges involved with conducting the weight check in the home. The nurses would then propose to delay the weighing until the patient was scheduled for a short stay in a nursing home. The nurses found that it could be difficult to measure height: “She is unable to stand upright.” They discussed other ways of measuring height, for example by taking under-arm measurements, but this method was never tested in practice.
Study A made use of the Nutrition Journal screening form. This tool strengthened the nurses’ observations and their interaction with the patients: “We are able to make lots of observations while we are preoccupied with this.” New nutrition-related initiatives were implemented, and they evaluated the effect relative to the patient’s situation. In their evaluation summaries, the nurses pointed out that the nutritional screening did not take up much extra time: “It’s not as time-consuming as you think.”
If the nurses were working under great pressure, some chose to postpone the nutritional screening to another day. A number of nurses in study B pointed to the staffing situation as a constraint that could prevent them from undertaking the nutritional screening. They were also critical of the local authorities’ practice of drawing up time schedules to the minute, which they felt was a professional constraint: “If the job is shower x 1, we will never ask about food before we see it is a problem.”
When the nurses were planning meals for people with a poor appetite, they accentuated the social significance of meals: “Eating together creates a sense of wellbeing.” The nurses felt that for home-dwellers who live alone and whose food intake is low, eating in the company of others would be an important initiative to improve their wellbeing. They considered that co-eating was not feasible within the time constraints imposed on community nurses. They were also critical of the practice of re-heating dinners: “Three minutes of a faint aroma emanating from the microwave will never sharpen anyone’s appetite.”
Discussion
The community nurses considered that the provision of patient-centred, practical nutritional care was important. They felt that it was challenging to meet the requirement for systematic screening of the patient’s nutritional status. In institutions they are able to observe and screen the intake of foods and liquids, but in a domestic setting it can be difficult to undertake such observations and screenings if the home-dwelling patients forget what they eat and drink. They also pointed out that it may be inappropriate to make use of such recording practices in the home.
In an effort to explain the complexity of the nutritional practice in community nursing, this is illustrated through four mutually dependent dimensions (figure 1).
The individual
The first dimension includes the nurses’ knowledge and understanding of the home-dweller’s experience of their own life situation and personal challenges. This is the very core of the nurses’ practice. This person-centred perspective goes beyond the traditional perception of individualized care (33). Person-centred care means that the nurse is familiar with the individual’s values and life story, demonstrates responsiveness and attention and involves the individual in decisions about their own physical and mental care (33). This dimension involves an understanding that the patients’ assessment of their own functional abilities may differ from that of the health care personnel (34). Decisions made by the nurse are therefore the results of negotiations between nurse and patient (35).
In nursing, nutritional person-centred care revolves around making practical arrangements for meals in cooperation with the home-dweller. Furthermore, the studies’ findings showed that the nurses were concerned about the food intake of dementia sufferers who live alone. The challenge for their nutritional practice was to support the home-dwellers autonomy while at the same time identifying the health-related challenges of reduced appetite and weight loss (6, 36).
Some nurses assumed that the patients did not wish to be weighed and were surprised that the home-dwellers and their relatives took a positive attitude to the weight check. Relatives were grateful for the screening and for professional attention being paid to insufficient food intake and weight loss. These findings coincide with earlier research which has shown that relatives are often very concerned when the patient suffers involuntary weight loss (10, 37, 38). The discrepancy between the nurses’ assumptions and the home-dwellers’ experience of being weighed, highlights the importance of ensuring that community nurses are aware of the patient’s values and preferences in their nutritional work.
The home
The next dimension includes the importance of the domestic arena to the provision of nutritional care. The home may be described in positive terms such as security, intimacy, private life and control (39). The findings of our study showed that the nurses attached importance to the home-dwellers’ independence and dignity when referring to the home. This finding matches the traditional values of the community nursing service whose hallmarks include the preservation of domesticity, and ensuring that the home remains the individual patient’s arena (40).
On the other hand, it was a challenge that the home visits were of short duration and gave little opportunity for systematic nursing observations around the clock. When seeking to develop the nutritional care work further, it will therefore be important to ask how the community nurses may strike a balance between what is appropriate in the private space, and the requirement for systematic observations.
Practical arrangements
The third dimension includes practical arrangements, which are often based on the nurses’ local knowledge relating to available time slots and their opportunity to prioritise tasks. The solution-oriented attitude of nurses with respect to practical nutritional interventions coincides with earlier studies of service-provision in the home (41). Within their own scope of action the nurses prioritised the sickest patients with a need for intake of nutrition. This matches reasonable expectations of the right course of action in a medical context (42).
The screening and follow-up of a large number of people would result in greater workloads, and this requires a level of prioritisation beyond what is available to individual nurses within the confines of their shift. The assessment of nutritional risk should therefore be included in decision-making procedures, and screening tools should be included in the documentation system and daily schedules. A number of case studies have shown that the discussion about screening tools may end up with no screening tool being chosen because no agreement is reached about which is the most useful (43). The choice of a screening tool is therefore a necessary first step (43).
Our study showed that in one municipality, the managers were involved with the choice of a screening tool, while no such decision had been made in the other municipality. Inadequately resolute support was considered to be an obstacle to a change of practice. This finding coincides with other studies which point out that managers must be active participants and drivers in the quality development effort (25). The nutritional screening is intended to help ensure that malnutrition is not ignored. According to Juul and Frich (44), “bottom-up” and “top-down” processes are all useful and important for achieving change of practice. A lack of clarity with respect to areas of responsibility may therefore prevent the development of knowledge-based practice (44).
Professional guidelines
The fourth dimension includes the need for general knowledge about nutrition and the need to understand how the professional guidelines may be applied. It is also necessary to understand how malnutrition arises, and what actions must be followed up in order to draw up long-term strategies for change (43).
In their reflective discussions the nurses discussed the requirements set out in the national professional guidelines with respect to assessments of nutritional risk. They voiced their professional appreciation of the need to record food intake and check the patients’ weight when assessing their nutritional risk (18). However, they also questioned whether it was possible to meet the nutritional risk assessment requirements with respect to all patients on registration with the community nursing service, and monthly thereafter.
Furthermore, the wording of the guidelines was considered to be academic and far removed from the every-day language used in clinical practice. The nurses also had no experience of using standard tools for assessing nutritional risk. These findings were not unexpected. Earlier research has demonstrated negative attitudes among nursing staff to systematic screening and nutritional assessment (41, 45). The Norwegian Board of Health Supervision have found in their system audits that 80 per cent of all local authorities undertook no systematic risk assessment with respect to nutrition (46). This demonstrates that there is a need for greater knowledge and more systematic nutritional care in community nursing.
The study’s strengths and weaknesses
The focus theme of this study concerned the nutritional care provided by community nurses and the requirements set out in the national professional guidelines. It is a strength that the study is based on and analyses data from three different groups of nurses who had explored their own practice over time. At the same time, it is a challenge that data from these groups stem from two independent projects in which the nurses in study A were more action-oriented than those who took part in study B.
The purpose of this study has therefore been to look for commonalities between the two earlier studies while ensuring that the nurses’ different views were voiced across all groups. While conducting our analyses we have however been aware that a pressure for consensus may be a possible source of error, causing participants to express a shared understanding while they in fact hold different views (26).
In both projects the researchers made use of open-ended questions and invited the nurses to share their experience of providing nutritional care in compliance with the requirements of the professional guidelines. The methodology involving reflective discussions was used in both projects since the third author acted as research supervisor for study A and as participant moderator for study B.
The objective is not to generalise from the results of the qualitative analyses (30). The study shows the nurses’ experiences while the researchers add theoretical knowledge and research methodology beyond their experience-based knowledge. Because there is little research-based knowledge available about the implementation of the Norwegian Guidelines for Prevention and Treatment of Malnutrition (18) in the community nursing service, the results of the study will have validity if they can contribute to continued discussion and inspire further studies.
Conclusion
The nutritional nursing care provided by the community nursing service is characterised by person-centred and practical approaches suitable for the domestic arena. Implementing standardised screening for nutritional risk, which is one of the requirements set out in the national professional guidelines, may therefore be seen as a challenge (18). On the other hand, the national professional guidelines create a shared knowledge base for managers and nurses. The findings of this study show that it is important to ask critical questions about whether the national professional guidelines take sufficient account of the domestic context. The community nurses have limited opportunities to accurately record the intake of food and drink around the clock.
In order to strengthen the nutritional work carried out by community nurses, it is important to continue sharing experiences and to contribute to critical reflection on ways that standardised mapping tools may serve to provide quality assurance of practice. To implement systematic assessments of nutritional risk within the existing framework of resources, it is essential that management and staff within the community nursing service work in closer partnership with patients and their relatives.
References
1. Sortland K, Gjerlaug AK, Harviken G. Vektdokumentasjon, kroppsmasseindeks, måltidsfrekvens og nattefaste blant eldre sykehjemsbeboere – en pilotstudie. Vård i Norden 2013;33(1):41–5.
2. Keller HH. Promoting food intake in older adults living in the community: a review. Applied Physiology, Nutrition, and Metabolism 2007;32(6):991–1000.
3. Arvanitakis M, Van Gossum P, Coppens L, Doughan A. Nutrition in care homes and home care: Recommendations – a summary based on the report approved by the Council of Europe. Clinical Nutrition 2009;28(5):492–6.
4. Smoliner C, Norman K, Wagner K-H, Hartig W, Lochs H, Pirlich M. Malnutrition and depression in the institutionalised elderly. British Journal of Nutrition 2009;102(11):1663–7.
5. Stajkovic S, Aitken EM, Holroyd-Leduc J. Unintentional weight loss in older adults. (Case study). CMAJ: Canadian Medical Association Journal 2011;183(4):443.
6. Tamura BK, Bell CL, Masaki KH, Amella EJ. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: A systematic review of the literature. Journal of the American Medical Directors Association 2013;14(9):649–55.
7. Saletti A, Johansson L, Yifter-Lindgren E, Wissing U, Österberg K, Cederholm T. Nutritional status and a 3-year follow-up in elderly receiving support at home. Gerontology 2005;51(3):192–8.
8. Sørbye LW. Frail homebound elderly: basic nursing challenges of home care : a comparative study across 11 sites in Europe. Tromsø: Universitetet i Tromsø, Seksjon for sykepleie- og helsevitenskap; 2009.
9. Yang Y, Brown CJ, Burgio KL, Kilgore ML, Ritchie CS, Roth DL et al. Undernutrition at baseline and health services utilization and mortality over a 1-year period in older adults receiving Medicare home health services. Journal of the American Medical Directors Association 2011;12(4):287–94.
10. Kvamme J-M, Olsen J, Florholmen J, Jacobsen B. Risk of malnutrition and health-related quality of life in community-living elderly men and women: The Tromsø study. Quality of Life Research 2011;20(4):575–82.
11. Mirmiran P, Hosseini-Esfahani F, Jessri M, Mahan LK, Shiva N, Azizi F. Does dietary intake by Tehranian adults align with the 2005 dietary guidelines for Americans? Observations from the Tehran lipid and glucose study. Journal of Health, Population, and Nutrition 2011;29(1):39–52.
12. Rist G, Miles G, Karimi L. The presence of malnutrition in community-living older adults receiving home nursing services. Nutrition & Dietetics 2012;69(1):46–50.
13. Myhre T, Haugen HK, Willumsen T, Bergland A. Tannhelse og livskvalitet hos personer etter hjerneslag. Sykepleien Forskning 2014;9(2):114–22. Available at: https://sykepleien.no/forskning/2014/05/tannhelse-og-livskvalitet-hos-personer-etter-hjerneslag(downloaded 02.05.2017).
14. Mowé M, Diep L, Bøhmer T. Greater seven – year survival in very aged patients with body mass index between 24 and 26 kg/M2. Journal of the American Geriatrics Society 2008;56(2):359–60.
15. Söderhamn U, Christensson L, Idvall E, Johansson A, Bachrach-Lindström M. Factors associated with nutritional risk in 75-year-old community living people. International Journal of Older People Nursing 2012;7(1):3–10.
16. Bjerrum M, Tewes M, Pedersen P. Nurses’ self-reported knowledge about and attitude to nutrition – before and after a training programme. Scandinavian Journal of Caring Sciences 2012;26(1):81–9.
17. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN Guidelines for nutrition screening 2002. Clinical Nutrition 2003;22(4):415–21.
18. Helsedirektoratet. Nasjonale faglige retningslinjer for forebygging og behandling av underernæring. Oslo: Helsedirektoratet. 2009.
19. Green SM, James EP. Barriers and facilitators to undertaking nutritional screening of patients: A systematic review. Journal of Human Nutrition and Dietetics 2013;26:211–21.
20. Rycroft-Malone J. Implementing evidence-based practice in the reality of clinical practice. Worldviews on evidence-based nursing / Sigma Theta Tau International, Honor Society of Nursing 2012;9(1):1.
21. Bjornsdottir K. The ethics and politics of home care. International Journal of Nursing Studies 2009;46(5):732–9.
22. McCormack B, McCance TV. Development of a framework for person-centred nursing. Journal of Advanced Nursing 2006;56(5):472–9.
23. McCormack B, McCance, Tanya. Practice development in nursing and healthcare (2. ed.). Somerset, NJ, USA: John Wiley & Sons. 2013.
24. Hummelvoll JK. Verdiundersøkende samtaler i lokalsamfunnsbasert psykisk helsearbeid. Tidsskrift for psykisk helsearbeid 2006;3(02):116–29.
25. Jensen LH. Kvalitetsutvikling i pleie- og omsorgstjeneste i sykehjem og hjemmebaserte tjenester – muligheter og begrensninger : et praktisk deltagende aksjonsforskningsprosjekt. (Doktorgradsavhandling). Oslo: Universitetet i Oslo, Institutt for sykepleievitenskap. 2009.
26. Hummelvoll JK. Flerstegsfokusgruppeintervju – en sentral metode i deltagerbasert og handlingsorientert forskningssamarbeid. Klinisk Sygepleje, 2010;24(3):4–13.
27. Velken R. Ernæringskartlegging i hjemmebasert omsorg «Sammen er vi sterke». (Master's thesis). Drammen: Høgskolen i Buskerud, Avdeling for Helsefag. 2010.
28. Meyer S, Jensen LH. Hjemmesykepleieres erfaring med ernæringsarbeid og kartlegging av underernæring. Rapport fra Høgskolen i Buskerud, nr. 92. Drammen: Høgskolen i Buskerud. 2012.
29. Kemmis S. Exploring the relevance of critical theory for action research: Emancipatory action research in the footsteps of Jürgen Habermas. I: Reason PB, Bradbury H. (red.). Handbook of Action Research. London: SAGE. 2001 (p. 94–105).
30. Halkier B, Gjerpe K. Fokusgrupper. Oslo: Gyldendal Akademisk. 2010.
31. Kvale S, Brinkmann S, Anderssen TM, Rygge J. Det kvalitative forskningsintervju (2. ed.). Oslo: Gyldendal Akademisk. 2009.
32. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today 2004;24(2):105–12.
33. McCormack B, McCance T. Person-Centred Nursing : Theory and practice. Hoboken, NJ, USA: Wiley-Blackwell. 2010.
34. Petersen HVH, N. Geriatriske patienters egenvurdering av funktionsevne ved udskrivelse til hjemmet. Klinisk Sygepleje 2009;23(2):43–54.
35. McCormack B. A conceptual framework for person-centred practice with older people. International Journal of Nursing Practice 2003;9(3):202–9.
36. Tomstad ST, Soderhamn U, Espnes GA, Soderhamn O. Lived experiences of self-care among older, home-dwelling individuals identified to be at risk of undernutrition. Journal of Multidisciplinary Healthcare 2012;5:319–27.
37. Plathe H, Jensen LH. Pårørendes opplevelser og erfaringer ved ufrivillig vekttap hos lungekreftpasienter i palliativ fase. Sykepleien Forskning 2012;7(2):124–31. Available at: https://sykepleien.no/forskning/2012/06/parorendes-opplevelser-og-erfaringer-ved-ufrivillig-vekttap-hos(downloaded 04.04.2017).
38. Grov EK, Eklund ML. Reactions of primary caregivers of frail older people and people with cancer in the palliative phase living at home. Journal of Advanced Nursing 2008;63(6):576–85.
39. Manzo LC. Beyond house and haven: toward a revisioning of emotional relationships with places. Journal of Environmental Psychology 2003;23(1):47–61.
40. Solheim M, Aarheim KA, Gamlem K. Kan eg komme inn? : verdiar og val i heimesjukepleie. Oslo: Gyldendal Akademisk. 2004.
41. Bachrach‐Lindström M, Jensen S, Lundin R, Christensson L. Attitudes of nursing staff working with older people towards nutritional nursing care. Journal of Clinical Nursing 2007;16(11):2007–14.
42. Johannessen KI, Molven O, Roalkvam S, Aakre M. Godt, rett, rettferdig : etikk for sykepleiere. Oslo: Akribe. 2007.
43. Visvanathan R. Undernutrition and housebound older people. Nutrition & Dietetics 2009;66(4):238–42.
44. Juul HJ, Frich JC. Kartlegging av underernæring i sykehus: hva hemmer og fremmer sykepleieres bruk av screeningverktøy for identifisering av ernæringsmessig risiko? Nordisk Sygeplejeforskning 2013; 3(2):77–89.
45. Klitzke M, Sjömar J, Adolfsson P, Kirsebom M, Nordin K. Sjuksköterskors kunskap om och attityder till underernäring. Uppsala: Uppsala Universitet, Institutionen för folkhälso- och vårdvetenskap. 2013. Available at: http://www.diva-portal.org/smash/get/diva2:637245/FULLTEXT01.pdf(downloaded 04.04.2017).
46. Statens helsetilsyn. Krevende oppgaver med svak styring: samlerapport fra tilsyn i 2010 med kommunenes sosial- og helsetjenester til eldre. Oslo: Statens helsetilsyn. 2011.










Comments