Electronic message exchange for patients discharged from hospital
Whereas «PLO»-messages serve as a beneficial communication tool, they have to be supplemented with oral communication and meetings.
Bakgrunn: Utskriving fra sykehus til kommunal hjemmetjeneste er en sårbar situasjon for pasienter. Bruk av PLO-meldinger skal sikre at tilstrekkelig og relevant informasjon overføres ved pasientoverganger mellom sykehus og hjemmetjeneste. Sykepleiernes erfaringer med PLO-meldinger i utskrivningsprosessen er per i dag et lite utforsket område.
Hensikt: Å utforske sykepleiernes erfaringer med bruk av PLO-meldinger ved utskrivning av pasienter fra sykehus til kommunal hjemmetjeneste.
Metode: Kvalitativ studie med intervjuer av 41 helsearbeidere ved ett universitetssykehus og i tre kommuner.
Resultat: Bruk av PLO-meldinger bidro til raskere avklaring og tilgang til informasjon ved utskrivningsplanlegging og selve utskrivelsen av pasienter. Sykepleierne benyttet likevel supplerende informasjonskilder for å sikre overføring av tilstrekkelig informasjon mellom sykehus og hjemmetjeneste. Årsaken til dette var uforutsigbarhet knyttet til pasientens utreisedato, inkonsistens mellom pasientens legemiddelliste i kommuner og i sykehus, manglende informasjon i meldinger og forskjeller i faglig tilnærming mellom nivåene.
Konklusjon: PLO-meldinger er et nyttig kommunikasjonsverktøy. Det må likevel kompletteres med muntlig kommunikasjon og møter for å ivareta informasjonskontinuitet ved utskrivningsplanlegging og utskrivning av pasienter fra sykehus til hjemmetjeneste. Videre tiltak bør rettes mot hvordan informasjonsinnholdet i meldingenes fritekstfelter bør fremstå.
The Coordination Reform of 2012 specifies that communication between health personnel shall be mainly electronic (1). The goal is for all hospitals and municipalities to have introduced electronic messaging by the end of 2015 (2). Such electronic communication shall facilitate a more efficient and secure collaboration on patients moving between hospitals and municipal care services (1).
Coordination challenges in the interface between hospital and municipalities are well documented. Patients who are discharged from hospital into municipal care are particularly vulnerable (1,3): They remain in hospital waiting for municipal care services (4), the content of the information exchanged is incomplete or unclear (5-7), and the information flow is fragmented and characterised by inefficient communication lines (8-10).
Organisational factors such as poor planning of the patient transfer and limited knowledge of the patient’s condition also create challenges in the communication between hospital and municipality (11). This is also the case for cultural factors such as nurses’ different professional approaches to, and understanding of, the patient’s needs in hospital and municipal care services (12,13). National and international literature shows that there is potential in using information and communication technology (ICT) in the exchange of collaboration information (14-17).
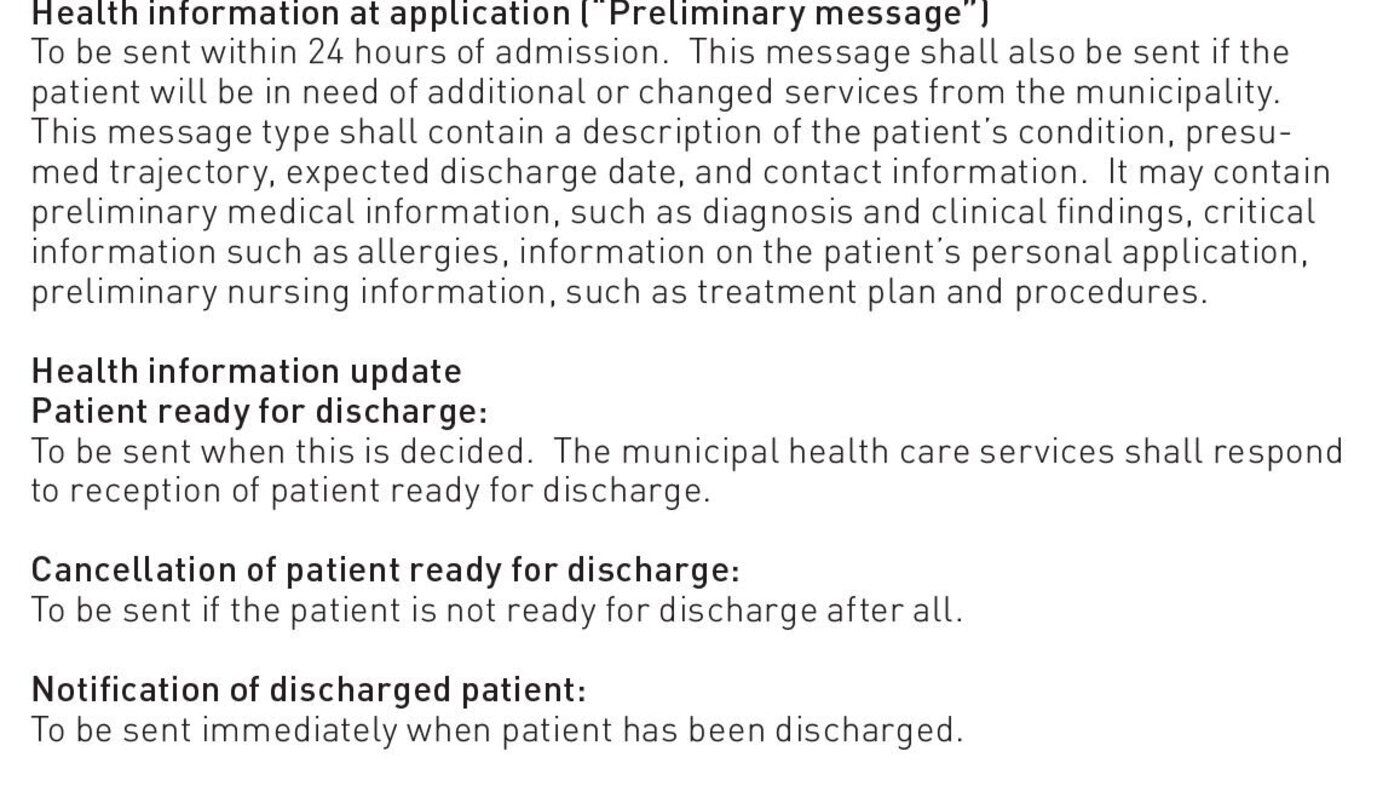
Flaws in the information exchange and communication between hospital and municipality are serious as they may lead to the patients not receiving the treatment and care they need (18-20). To ensure the transfer of sufficient and relevant information between hospital and municipality, treatment and care messages (PLO messages) have been introduced as tools to improve such collaboration. The PLO messages comprise a set of several standardised messages to support the admittance, assessment/treatment, and discharge phases of a hospital stay. Dialogue messages for current, interactive collaboration are also available (see table 1) (21,22). As of January 1, 2015, 99 per cent of all municipalities (422/428) had introduced PLO-messaging in their collaboration with hospitals. This is a sharp increase from only four municipalities in May of 2012 (23).
Limited documentation exists on the effects of various collaboration efforts in general (24), and on experiences with electronic messaging between hospital and municipal health care services in particular. Feedback from other areas in the health services on the use of electronic messaging reports gains such as increased access to necessary health information, and improved quality of the information exchanged (23,25,26). All in all, few studies have taken a direct look at the collaboration between nurses in the use of PLO messages when discharging patients from hospital to municipality.
The purpose of this study is to explore nurses’ experiences with PLO-messaging in the discharge of patients from hospital to municipal health care services. The study has at its point of departure the concept of informational continuity as defined by Haggerty et al. and Reid et al. (27-28): Informational continuity is here related to the transfer of “relevant and sufficient information” between health workers in a chain. This encompasses personal information on the patient, health condition and prior treatment, so that further services can be given in accordance with the patient’s need for assistance at the right time.
Material and method
We used an explorative, qualitative design with semi-structured individual interviews and group interviews (8/14). The study was carried out at a university hospital and in the municipal home health care services of three municipalities in the hospital’s region. Strategic selection was used for the inclusion of the hospital and one municipality, as these were the first to introduce electronic messaging. The other two municipalities were chosen at random.
The interviews were carried out from February to November 2014 and 41 employees participated. The majority of the participants had been employed at their current unit since before the implementation of the Coordination Reform in 2012. In order to widen our understanding of the complexity of the collaborative chain, we included health personnel in a variety of roles. At the hospital, 15 nurses and two social workers from a variety of wards in three divisions participated. We interviewed 24 employees in the municipalities: 12 were practicing nurses in the municipal home health care services, 10 were nurses in coordinator-purchaser or management positions, and two were responsible for IT. Each interview lasted 40-50 minutes, was recorded and transcribed. The interview guide was worded to bring out health personnel’s views, assessments, and experiences with using PLO messages, with questions on type, frequency, information sharing, did they receive enough information to provide responsible health care, and what other forms of communication did they use. All authors participated in the data collection to ensure accuracy and consistency in the process.
We used an inductive approach in the analysis (29). First, all three authors went through the material and identified overarching themes. We found that communication and collaboration in the discharge process were central themes for informants both in hospital and municipal home health care services, and we decided to pursue this further. We worked on meaning condensation and coding (30), and then categorised the material based on three phases of a hospital stay: Admission, assessment/treatment, and the discharge phase itself. These phases represented a variety of communication and collaboration challenges. We finally went through the categories in each of the three phases and gathered them under three analytical themes. These themes make up the structure in the results chapter.
The project was reported to The Norwegian Centre for Research Data and to the regional health authority’s privacy officer. The informants were recruited through their leaders and given written information on the project. We received written consent from all participants in the study.
Major findings
The major findings show that the informants were satisfied with communicating using PLO messages, both in general and in connection with the planning of the discharge process in particular. The use of PLO messages was well integrated in the nurses’ workday and enabled a closer collaboration between hospital and municipalities. “A time saver” was a concept that kept coming up in the interviews.
The analysis showed that each phase of a hospital stay entails different challenges for the nurses with regard to communicating and coordinating the planning and execution of the discharge. Health personnel have to set a discharge date as early as at the time of admission; we have called this “predicting the unpredictable”. During the assessment and treatment phase the hospital nurses, and especially the municipal nurses, must stay updated with regard to the patient’s progress. They must also, at the same time, start planning the services to be delivered to the patient following discharge. This we address in the chapter “keeping the thread”. On the day of discharge a substantial amount of information must be communicated from hospital to municipality, and the municipal health care services must have their own services ready for the patient. We have designated this “collecting the threads”, and address it in the final part of the results chapter.
Predicting the unpredictable
Information on the patient’s health condition, need of assistance, and expected time of discharge shall be transferred from hospital to municipal services within 24 hours of admission. The nurses used the message type “Health information at application” (“Preliminary message”) to the municipality for this information. They found estimating an expected date of discharge to be a challenge. Several nurses stated that they, not the physician, determined the date. This was usually based on experience with the length of treatment related to a specific illness. At times a patient was in such poor condition that setting a discharge date was impossible. The nurses would then inform the municipal health care services that an estimated date of discharge would be communicated at some point during the patient’s stay in the hospital.
How the municipalities dealt with “Preliminary messages” varied; anything from no action initiated to using the messages as a basis for decisions. The cause of the variations is unclear. One possible explanation may be that there were marked individual differences in how the nurses filled in the health information forms. Some of the hospital nurses put it like this: “It varies, I guess … I was taught to use the (patient’s) treatment plan. The plan lists (the patient’s) communication ability, activity level and so forth, and then you fill in what is needed”. And: “But I see that many nurses here send off only one line, such as that the patient is admitted for intravenous antibiotic treatment”. So content and level of detail both varied in the messages sent to the municipality.
“Keeping the thread”
The nurses at both levels provided examples that sending updated health information forms during the hospital stay was well integrated in their work practice. We did, however, find that these changes and updates were not always sufficient for the municipality to make decisions. In order to gather the missing information, or clarify issues regarding the patient’s health condition and level of functioning, the municipal health care services contacted the hospital through dialogue messages. At times the municipality also called the hospital on the telephone. As one informant put it: “Some information is missing – that is why we call. And - it’s about ‘what are their thoughts (on this patient)?’ And about knowing a bit more when there is only a few words jotted down (in the Health Information Form)”. The municipal care services would at times also use assessment visits to the hospital, but such practice varied between municipalities. The informants emphasised that an assessment visit might uncover discrepancies between the hospital’s and the municipality’s description of the patient’s need for care. This had consequences for the care services the patient would receive upon discharge: “We have those (the patients) we are uncertain about, or those that are new to us, or those that they describe as having a great need of treatment and care: It is not always that the (proper care need) is reported. So when we have no idea and nobody has seen the patient before, we go (to make an assessment visit) … Firstly, this simplifies the whole case work bit for us … another thing is that we have several times ended up with a totally different service (for the patient) than what the hospital has reported “ (Municipality).
We found that nurses in both hospital and municipality needed to know that messages had been received by collaborating health personnel. However, the hospital nurses suggested that there were differences in opinion as to what extent nurses were required to confirm reception of PLO-messages: “We thought that maybe it is a requirement that the municipality must confirm having received the PLO message. But, as some municipalities say: ‘no, we haven’t been told that this is a requirement’. We can see that the message has been sent, but we cannot see whether they (the municipality) have read it” (Hospital). The hospital considered feedback to be a precondition for proper planning of the patient’s discharge. It was important in order to inform the patient of what services he or she would receive upon discharge, and for ordering an ambulance to transport the patient.
Both hospital and municipalities used PLO messages to keep track of the patient flow. More specifically, the nurses used the content of the messages as a basis for working out their own manual lists, either on paper or electronically. The municipality used these lists to keep track over time of patients ready for discharge. This ensured that no patients dropped out of the system: “And then the list really is quite good. You constantly keep in mind whom to ask for, or check whether the patient has arrived home (…). Yes – it’s sort of a shadow account”. We also found an example of the hospital using such a list to keep track of patients in and out of a ward, or to identify needs for nursing support from the hospital for patients who were discharged into municipal home health services: “If the patient is going home with CVC (central venous catheter), the municipal employees need training. Then we have to deploy an ambulating team”.
Gathering the threads
The discharge situation started with the hospital nurses sending “Notification of patient ready to be discharged” to the municipality. The nurses also filled in and sent off the message type “Discharge report”. Some nurses said that they also sent a paper printout of the discharge report along with the patient. Discharging a patient on a Friday afternoon constituted a typical situation: “The patient does not always arrive home during office hours and this may leave those (municipality) who are going to receive the patient without access to the relevant information” (Hospital). The patient was also given a medication list and discharge summary, if completed, on paper by the hospital.
The hospital nurses reported that filling in the Discharge report was difficult at times. This was due to the very format of the report. It is “a bit awkward”, as one nurse put it. The nurses had a guide to follow, but they felt that the pointers in the guide overlapped. Some also experienced it as doing the same work twice as the discharge report is almost identical to the Health information form, even if they were able to reuse texts through cutting and pasting.
Practicing nurses in the municipal home health care services were frequently not involved until the very day of discharge, when they received the message ‘Patient ready for discharge’. The nurses said that at times they experienced that for already known users, the message with the discharge report from the hospital did not arrive until a couple of days after the user’s arrival home. They solved this predicament by making a copy of the paper copy the user was given at the hospital. For municipalities that did not receive the patient medication list electronically, the paper version that accompanied the patient represented an added challenge. The nurses frequently experienced discrepancies between the medication list accompanying the patient and the list of medications the patient was on before being admitted to hospital. This added to their workload; the patient’s primary physician had to be contacted through electronic messages or via telephone to confirm the changes in medication. The nurses also had to spend time on manually entering the medication changes into the report: “And then, at times, that list (medication list) doesn’t quite agree (with the medication list prior to admission), or there are pills on the old list that we think he (the patient) ought to keep taking. And then we have to, when the next workday arrives, confer with the primary physician on whether that [medication] should in fact be discontinued or …” (Municipality). There were no corresponding statements where electronic medication lists were introduced.
Discussion
The purpose of this study was to explore nurses’ experiences with the use of PLO messages at the discharge of patients from hospital to municipal health care services. One major finding was that the nurses expressed satisfaction with being able to communicate and exchange information electronically. The use of PLO messages was well integrated into the workday. However, the nurses reported that the PLO messages did not support all aspects of their communication needs. They therefore used supplemental communication channels to ensure informational continuity. They were thus able avoid any unfortunate consequences for the patient. This challenges the Coordination Reform’s aim to make electronic communication the preferred form of communication between health personnel (1).
Electronic messaging had to be supplemented with oral speech and in person meetings to clarify and explore ambiguities, and/or gather additional information. This was due to, a. o., the lack of predictability with regard to the patient’s discharge date, inconsistencies between the patient’s medication list in the municipality and in the hospital, information missing in messages, and differences in professional approach between levels. In this way the study’s findings nuance the image of earlier reported gains from electronic messaging. This proves increased access to necessary health information and improved quality of content in the information transferred (26). The findings are nevertheless in accordance with other research that concludes that electronic communication solutions in the health services must frequently be supplemented with other communication channels (31-34).
The need to supplement with other channels of communication (telephone and assessment visits) to gather sufficient and relevant information on the patient was particularly voiced by the municipal nurses. They frequently had to circumvent the messaging system in order to secure the treatment of the patient. This was due to inconsistencies between the (paper) medication list accompanying the patient and the patient’s medication list prior to admission. In accordance with examples from the literature, this study shows that manual information exchange on medication may represent a threat to patient security (25,37). This was not reflected in cases where electronic medication lists were in use (25,37).
The need for supplemental communication channels also related to the information content in messages passed from hospital to municipality, such as “Preliminary message”, which initiated the discharge process. In accordance with findings in studies from before the electronic messaging system was implemented (12,13), the nurses in hospital and municipality still had different professional approaches to the patient’s health condition. The hospital nurses related the message information to diagnosis and treatment, e.g. that the patient was admitted with pneumonia and would receive intravenous antibiotic treatment. The municipal nurses, on the other hand, needed information on the patient’s total level of functioning, need for assistance, and preferences. Such information was needed in order to prioritise the most seriously ill patients for further care in a nursing home. This was also necessary in order to plan for care services and technical aids or equipment prior to the patient’s arrival home, and thus avoid any postponement of patient treatment and follow-up (18). The need for oral clarifications and additional information was especially evident in the case of patients who had not formerly been users of municipal services, the so-called “0-user”.
Standardised PLO messages are based on standard content elements with a possibility of adding free text. Our findings show that the nurses found the use of free text in the PLO messages to be a challenge. Although the hospital nurses were able to harvest text content from an electronic patient report, they nevertheless reported individual variations in the wording of the messages. This would be the case, for instance, with regard to the richness of the textual description and which fields were used. The results of a recently published article does show, however, that the fact that the messages they write will be stored in the report system makes nurses pay more attention to the way they express themselves in writing (38).
The use of free text with individual choices of words and phrasing may make the hospital’s documentation of health services and the patient’s level of functioning appear somewhat fragmented to the receiver, the municipality. One possible explanation is that the report leaves room for unstructured documentation and that there was overlap in the work performed due to the similarities between the “Health information form” and the “Discharge report”. More recent literature, however, points to explanatory factors such as differences in the report systems in hospital and municipality, and that the profession lacks a standardised national model for the nurses’ reports (22). That health personnel communicate in an agreed-upon, professional language - semantic interoperability (22) - is an important precondition for exchanging and sharing information across levels.
Technology can open up to new ways of working (39). A somewhat surprising finding in this study was that hospital and municipal nurses both used the PLO messages to keep track of the patient flows. Such use did, however, vary within and between levels. A possible explanation is the uncertainties surrounding the patient’s expected date of discharge from hospital. The municipalities reported receiving a series of change of date messages regarding patients’ discharge dates. This would complicate their user records. The municipal care services would have to make sure that the patients did not drop out of the system as well as adapt the planning of services and resources. Another explanation may relate to whether the PLO messaging system has a function for feedback on messages received, and how well known this is within an organisation (25). For nurses on both levels it was important to receive notification of whether their messages had been received and read.
The study’s limitations
The sample of one hospital and three municipalities is too small to draw any general conclusions regarding the nurses’ experiences with the use of PLO messages at discharge of patients from hospital to municipal home health care services. Neither have we considered organisational factors or the length of time the PLO messages have been in use at the various units. Findings discussed in relation to earlier research do, however, support the validity of the study.
Conclusion
PLO messaging provides a useful communication tool in the discharge process. It must, however, be supplemented by oral communication and personal meetings in order to safeguard informational continuity with regard to discharge planning and discharge of patients from hospital to municipal home health care services. In order to strengthen the message exchange system’s role as a communication tool, more work is needed on the content of the message form’s free text fields. Achieving a common understanding for the need for information across health service levels is also important.
The study is supported by The Research Council of Norway, RCN project no 229623-SIKT (EVASAM-programme).
References
1. St.meld. nr. 47 (2008-2009).
Samhandlingsreformen: Rett behandling – på rett sted – til rett
tid. Oslo: Helse-og Omsorgsdepartementet (HOD); 2012.
2. Norskhelsenett årsrapport
2013.Norsk Helsenett; Tilgjengelig fra:
https://www.nhn.no/om-oss/Documents/arsrapport-NHN-2013.pdf.
Nedlastet 21-10-2015.
3. Bauer M, Fitzgerald L,
Haesler E, Manfrin M. Hospital discharge planning for frail older
people and their family. Are we delivering best practice? A review
of the evidence. Journal of Clinical Nursing.
2009;18(18):2539–46.
4. KS FOU-prosjekt nr. 124005.
Utskrivningsklare pasienter – endrer praksis seg. Oslo: Rambøll
Mangement Consulting, 2012. Tilgjengelig fra:
http://www.ks.no/contentassets/dffac809f5934f4bbf69c8348c5c47ec/124005_….
Nedlastet 21-10-2015.
5. Olsen RM, Hellzén O, Enmarker
I. Nurses’ information exchange during older patient transfer:
prevalence and associations with patient and transfer
characteristics. International Journal of Integrated Care, mars
2013. ISSN 1568–4156. Tilgjengelig fra:
http://www.ijic.org/index.php/ijic/article/view/879. Nedlastet
21-10-2015.
6. Olsen RM, Hellzén O, Skotnes
LH, Enmarker I. Breakdown in informational continuity of care
during hospitalization of older home-living patients: a case study.
International Journal of Integrated Care, mai 2014. ISSN 1568–4156.
Tilgjengelig fra:
http://www.ijic.org/index.php/ijic/article/view/1525. Nedlastet
21-10-2015.
7. Storm M, Siemsen IMD,
Laugaland KA, Dyrstad DN, Aase K. Quality in transitional care of
the elderly: Key challenges and relevant improvement measures.
International Journal of Integrated Care. Mai 2014. ISSN 1568–4156.
Tilgjengelig fra:
http://www.ijic.org/index.php/ijic/article/view/URN%3ANBN%3ANL%3AUI%3A1….
Nedlastet 21-10-2015.
8. Danielsen B, Fjær S.
Erfaringer med å overføre syke eldre pasienter fra sykehus til
kommune. Sykepleien Forskning. 2010;5(1):28-34.
9. Hellesø R, Lorensen M,
Sorensen L. Challenging the information gap – the patients transfer
from hospital to home health care. International Journal of Medical
Informatics. 2004;73(7–8):569–80.
10. Innspill til Helse- og
omsorgsministerens arbeid med samhandlingsreformen. Statens
helsetilsyn, 2008. Tilgjengelig fra:
https://helsetilsynet.no/no/Publikasjoner/Brev-hoeringsuttalelser/Utval….
Nedlasted: 21-10-2015.
11. Shah F, Burack O, Boockvar
KS. Perceived Barriers to Communication Between Hospital and
Nursing Home at Time of Patient Transfer. Journal of the American
Medical Directors Association. 2010;11(4):239–45.
12. Hellesø R, Fagermoen MS.
Cultural diversity between hospital and community nurses:
implications for continuity of care. International Journal of
Integrated Care. Feb 2010. ISSN 1568–4156. Tilgjengelig fra:
http://www.ijic.org/index.php/ijic/article/view/508. Nedlasted:
21-10-2015.
13. Valaker I. Et helhetlig
behandlingsforløp -om samhandling rundt pasienter. I: Bukve O,
Kvåle G (red). Samhandling og kvalitet i helseorganisasjoner. Oslo:
Universitetsforlaget AS; 2014.
14. Naustdal A-G, Netteland G.
Sjukepleiedokumentasjon i eit elektronisk samhandlingsperspektiv.
Sykepleien Forskning. 2012;7(3): 270–7.
15. Heimly V, Hygen J. The
Norwegian Coordination Reform and the Role of Electronic
Collaboration. Electronic Journals of Health Informatics.
2011;6(4). Tilgjengelig fra:
http://www.ejhi.net/ojs/index.php/ejhi/article/view/176.
Nedlastet:21-10-2015.
16. Marcotte L, Kirtane J, Lynn
J, McKethan A. Integrating Health Information Technology to Achieve
Seamless Care Transitions. Journal of Patient Safety. 2015.
Tilgjengelig fra:
http://journals.lww.com/journalpatientsafety/Fulltext/publishahead/Inte….
Nedlastet: 21-10-2015.
17. Hewner S, Seo JY.
Informatics´ Role in Integrating Population and Patientcentered
Knowledge to improve Care Transitions in Complex Chronic Disease.
Online Journal of Nursing Informatics. 2014;18(2). Tilgjengelig
fra:
http://www.himss.org/resourcelibrary/TopicList.aspx?MetaDataID=3055.
Nedlastet: 21-10-2015.
18. Netteland G, Naustdal A-G.
Risikofaktorer ved overganger. I: Bukve O, Kvåle G(red).
Samhandling og kvalitet i helseorganisasjoner. Oslo:
Universitetsforlaget AS; 2014.
19. Dunnion ME, Kelly B. All
referrals completed? The issues of liaison and documentation when
discharging older people from an emergency department to home.
Journal of Clinical Nursing. 2008;17(18):2471-9.
20. Berntsen G, Høyem A, Gammon
D. Helsetjenesten sett fra pasientens ståsted. Tromsø: Nasjonalt
senter for samhandling og telemedisin, Universitetssykehuset
Nord-Norge; 2014. NST-rapport 07–2014.
21. Helsedirektoratet. Veiviser
– Hvordan komme i gang med elektronisk meldingsutveksling i
kommunen. IS-1920. Oslo 2011. Tilgjengelig fra:
https://helsedirektoratet.no/retningslinjer/veiviser-hvordan-komme-i-ga….
(Nedlastet:21-10-2015).
22. Svanes M, Nyhus VÅ, Hagen O,
Bømark SR, Vabo G, Holen-Rabbersvik E. Veileder for klinisk
dokumentasjon av sykepleie i EPJ (v. 5.0). Norsk Sykepleierforbunds
Faggruppe for e-helse, 2015. Tilgjengelig fra:
https://www.nsf.no/vis-artikkel/2481424/10503/Ny-veileder-for-klinisk-d….
Nedlastet: 08-10-2015.
23. Slagsvold H.
Meldingsutbredelse i kommunehelsetjenesten. Norsk Helsenett SF,
2015. tilgjengelig fra:
https://nhn.no/aktuelt/Documents/vedlegg/KomUT-sluttrapport.pdf.
(Nedlastet: 21-10-2015).
24. Holte H, Lidal I, Gundersen
M. Utskrivning av pasienter med kronisk sykdom: effekt av ulike
former for samhandling mellom sykehus og kommunehelsetjeneste.
Rapport fra Kunnskapssenteret – Systematisk oversikt. 2013.
Tilgjengelig fra:
http://www.kunnskapssenteret.no/publikasjoner/utskrivning-av-pasienter-….
(Nedlastet:25-05-2015).
25. Borgen K, Melby L, Hellesø
R, Steinsbekk A. Elektronisk meldingsutveksling mellom
hjemmetjenestene og fastleger. Sykepleien Forskning.
2015;10(1):42–8.
26. PricewaterhouseCoopers. Gode
modeller for elektronisk meldingsutveksling i helsesektoren.
Kostnader og gevinster for små kommuner. På oppdrag fra KS og Norsk
Helsenett, 2014. Tilgjengelig fra:
http://www.ks.no/fagomrader/utvikling/fou/fou-rapporter/fou-elektronisk….
(Nedlasted:21-10-2015).
27. Haggerty JL, Reid RJ,
Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care:
a multidisciplinary review. BMJ 2003;327:1219.
28. Reid RJ, Haggerty JL,
McKendry R. Defusing the confusion: Concepts and Measures of
Continuity of Healthcare: Canadian health Services Research
Foundation; 2002. Tilgjengelig fra:
http://www.cfhi-fcass.ca/SearchResultsNews/02-03-01/58a53ce8-39f2-466a-….
29. Tjora AH. Kvalitative
forskningsmetoder i praksis. Oslo: Gyldendal akademisk;
2012.
30. Malterud K. Kvalitative
metoder i medisinsk forskning: en innføring. Oslo:
Universitetsforlaget; 2011.
31. Paulsen B, Romøren TI,
Grimsmo A. A collaborative chain out of phase. International
Journal of Integrated Care. Mars 2013. ISSN 1568–4156. Tilgjengelig
fra:
http://www.ijic.org/index.php/ijic/article/view/URN%3ANBN%3ANL%3AUI%3A1….
Nedlastet:11-05-2015.
32. Brattheim BJ, Toussaint PJ,
Faxvaag A. When Information Sharing is not Enough. Stud Health
Technol Inform. 2011;169:359-63.
33. Mäenpää T, Suominen T,
Asikainen P, Maass M, Rostila I. The outcomes of regional
healthcare information systems in health care: A review of the
research literature. International Journal of Medical Informatics.
2009;78(11):757–71.
34. Nordberg M. Elektronisk
sykepleierapport utfordrer sykepleiekontinuiteten. Sykepleien Fag.
2015(02):50–3.
35. Frydenberg K, Brekke M. Poor
communication on patients’ medication across health care levels
leads to potentially harmful medication errors. Scandinavian
Journal of Primary Health Care. 2012;30(4):234–40.
36. Kohn LT, Corrigan J,
Donaldson MS. To err is human: building a safer health system.
Washington, D.C.: National Academy Press; 2000.
37. Lyngstad M, Melby L, Grimsmo
A, Hellesø R. Toward Increased Patient Safety? Electronic
Communication of Medication Information Between Nurses in Home
Health Care and General Practitioners. Home Health Care Management
& Practice. 2013; 25(5): 203–211.
38. Melby L, Brattheim BJ,
Hellesø R. Patients in transition – improving hospital – home care
collaboration through electronic messaging: providers’
perspectives. Journal of Clinical Nursing. 2015 Sep 15. doi:
10.1111/jocn.12991. [Epub ahead of print].
39. Vimarlund V, Olve N-g,
Scandurra I, Koch S. Organizational effects of information and
communication technology (ICT) in elderly homecare: a case study.
Health Informatics Journal. 2008;14(3):195–210.
40. Vestlandsheftet. Veileder
for utbredelse av elektroniske meldinger mellom kommune, fastlege
og helseforetak på Vestlandet. Tilgjengelig fra:
https://www.bergen.kommune.no/bk/multimedia/archive/00152/Veilederen_p_….
Nedlastet: 21-10-2015.










Comments