Antibiotic-savvy nursing students? Nursing students’ knowledge and self-assessed competence in antibiotic use and resistance
Summary
Background: Modern medicine is dependent on effective antibiotics. However, antibiotic resistance has become a rapidly growing problem in society, posing a serious threat to global health. Appropriate antibiotic use is crucial to reducing antibiotic resistance in the future. Knowledge levels among nursing students in Norway in terms of antibiotic use and resistance are largely unexplored.
Objective: To identify nursing students’ knowledge of antibiotic resistance and use. We also aimed to examine their self-assessed competence in this area.
Method: The study has a descriptive cross-sectional design. The data were collected in a questionnaire sent to nursing students at four educational institutions in Norway between September 2019 and February 2020. The questionnaire consisted of 43 questions, divided into nine questions about self-assessed knowledge level and 34 questions about knowledge of antibiotic use, divided into six themes. We used ANOVA, t-tests and bivariate correlation analyses to assess the correlation between actual knowledge of antibiotic use and self-assessed knowledge, previous work experience in the health service, voluntary or compulsory teaching, educational institution and age.
Results: Out of 480 students invited to participate in the study, 410 (84.5%) responded. The students had an average of 48.6% correct answers for all the knowledge questions combined. They were least knowledgeable about antibiotic consumption, urinary tract infection and asymptomatic bacteriuria, as well as allergies and adverse effects. A high proportion of the students rated their own knowledge of antibiotic resistance and appropriate antibiotic use as low. The higher the students scored on the knowledge level, the higher they assessed their own knowledge. Neither age, previous work experience, nor whether the teaching was voluntary or compulsory had a correlation with knowledge level.
Conclusion: Nursing students have insufficient knowledge about antibiotic resistance and appropriate antibiotic use, and they also consider themselves to have little knowledge and a low competence level. This indicates a need to strengthen students’ competence to enable them to effectively utilise their professional roles to influence and prevent antibiotic resistance. Further research should examine whether knowledge levels have improved since relevant content was introduced at several educational institutions following completion of the study.
Cite the article
Mølsæter A, Henni S, Opheim R, Høye S, Børøsund E. Antibiotic-savvy nursing students? Nursing students’ knowledge and self-assessed competence in antibiotic use and resistance. Sykepleien Forskning. 2023;18(93743):e-93743. DOI: 10.4220/Sykepleienf.2023.93743en
Introduction
The discovery and application of antibiotics is considered one of history’s most significant medical breakthroughs. Antibiotics are a prerequisite for modern medical treatment and, along with growing prosperity and vaccines, have helped to increase life expectancy and improve public health (1). Without effective antibiotics, major surgical interventions and cancer treatments would be more challenging to carry out, significantly increasing the risk of mortality (2).
Antibiotic resistance
Antibiotic resistance is a rapidly growing problem. In 2012, the World Health Organization (WHO) declared it to be one of the world’s greatest health threats (3). In 2019, it was estimated globally that almost five million deaths could be linked to antibiotic resistance (4).
Estimates show that by 2050, up to ten million deaths per year could be linked to antibiotic resistance (5). There is therefore a pressing need for new types of antibiotics, but since the 1980s, very few new classes of antibiotics have been developed (6). Treatment options are limited when known antibiotics no longer work. Common infections that are currently considered harmless could once again become severe and deadly.
Global use of antibiotics by humans increased by 65% in the period 2000–2015 (7). A direct correlation is believed to exist between increased antibiotic use and the emergence of resistant bacteria (8, 9). Restrictive and appropriate use of antibiotics is therefore crucial for preventing the development of antibiotic resistance (2, 9).
The nurse’s role in preventing antibiotic resistance
In 2015, the WHO presented a global action plan (10) for a unified strategy to combat antibiotic resistance. The same year saw the launch of Norway’s national strategy to combat antibiotic resistance (2). The Ministry of Health and Care Services developed an action plan the following year to combat antibiotic resistance in the health service, which specifically emphasised the enhancement of competence through education for nurses and other groups (9).
The new regulations on national guidelines for nursing education include learning outcomes for antibiotic use and the development of resistance (11). Nurses perform daily tasks related to antibiotics, which impacts on usage. They therefore play a crucial role in what is termed ‘antibiotic stewardship’ (12, 13).
Antibiotic stewardship is defined as a coherent set of actions that promote responsible use of antibiotics (14). Such actions can, for example, include monitoring antibiotic use, reviewing antibiotic prescription practices, skills enhancement, information flow, improved sample collection and communication of results from microbiological testing, reassessment of indications and drug choices, infection diagnostics, good infection control and infection prevention (9, 15–18).
Several review articles have been published recently on antibiotic stewardship and the complex and important role of nurses in reducing the development and spread of antibiotic resistance (17–20). A consistent theme is that effective and successful antibiotic stewardship is dependent on nurses’ efforts (18–20) and that more education is needed on the topic, both in clinical practice and in nursing education (17, 19).
Education and knowledge on the topic are essential for enhancing nurses’ competence, recognition, self-confidence, motivation and awareness of how they can contribute (17–19). A Norwegian study shows that when nurses acquire more knowledge about antibiotics, they become more engaged (21).
A Spanish cross-sectional study demonstrates how nursing students have a low level of knowledge about antibiotics, especially antibiotic resistance (12). The study concludes that more education and knowledge are needed and that these should be better incorporated into the nursing curriculum.
Nursing education has a unique opportunity to incorporate antibiotic stewardship into its curricula. However, an English study shows that 37% of educational institutions do not include antibiotic stewardship in their curriculum, and only 12.9% teach antibiotic stewardship principles (22). This is despite international research demonstrating that teaching antibiotic stewardship to nursing students increases their awareness of antibiotic resistance and infection prevention (23).
Healthcare personnel in Norway participated in a study of knowledge and behaviour in relation to antibiotic use and resistance across 30 EU/EEA countries (24). The study showed that Norwegian healthcare personnel’s knowledge of antibiotic use was on a par with other European countries. However, knowledge gaps were identified, which emphasises the need for education in this area (24).
The level of knowledge among nursing students in Norway in relation to antibiotics use and resistance is a relatively unexplored area of research. This is also the case for factors within the education and individual characteristics of students that may impact on their knowledge level. Research in this area could help initiate targeted measures to enhance the knowledge of nursing students, enabling them to contribute to the prevention of antibiotic resistance.
Objective and research questions
The objective of the study was to identify nursing students’ knowledge of antibiotic resistance and use, and to examine their self-assessed competence in this area.
Research questions:
- How do nursing students assess their own knowledge and role in relation to antibiotic resistance and use?
- What is the level of knowledge among nursing students in relation to antibiotic resistance and use?
- What correlation is there between nursing students’ actual knowledge and self-assessed knowledge? We also examined whether the following factors impacted on actual and self-assessed knowledge: previous work experience in the health service, educational institution and age, as well as whether the teaching was voluntary or compulsory.
Method
Design
The study employed a descriptive cross-sectional design (25). The data were collected in a questionnaire sent in printed format to nursing students at four educational institutions in Norway between September 2019 and February 2020. We used the STROBE checklist for reporting cross-sectional designs.
Sample and data collection
Nursing students from the four educational institutions in south-east and south-west Norway participated in the study. We formally approached institutions that had been offered teaching material on the topic from the Antibiotic Centre for Primary Care (ASP), the Norwegian Institute of Public Health (FHI) and the National Centre for Antibiotic Use in Hospitals (NSAS).
The institutions invited the students to a teaching session where the teaching materials were used. The students who attended were asked to complete a questionnaire before the session started. They were given approximately 15 minutes to answer the printed questionnaire in the auditorium. The participants were second-year students (institution 3) and third-year students (institutions 1, 2 and 4).
All students had completed all or part of their clinical practice in a hospital setting and primary care. The teaching was compulsory at two of the four institutions.
Questionnaire
The questionnaire was developed by an expert panel consisting of professionals with a background in general medicine, internal medicine, infectious diseases, epidemiology and nursing science (Appendix 1 – in Norwegian).
The questionnaire included demographic questions (age category and previous work experience before starting their bachelor’s degree) and questions about self-assessed knowledge and the participant’s role in relation to antibiotic use. It also consisted of questions about knowledge of antibiotic resistance, antibiotic use and infection control. The questions were based on the teaching material from ASP, FHI and NSAS, as well as discussions by the expert panel. The questionnaire has not been validated.
Part 1 – self-assessed knowledge and role in relation to antibiotic use
Part 1 consisted of eight questions, where students assessed their own knowledge and role in relation to infection control, infection prevention, sample collection, monitoring antibiotic use and opportunities to influence antibiotic use, the difference between broad-spectrum and narrow-spectrum antibiotics, and actions to prevent antibiotic resistance.
Response alternatives were given on a Likert scale from 1–7, where 1 corresponded to ‘I have no knowledge’, and 7 corresponded to ‘I have all the necessary knowledge’. Since response alternative 4 is considered a neutral score, self-reported knowledge between 5 and 7 was considered ‘a high level of knowledge’. The possible total score for Part 1 of the questionnaire ranged from 8 to 56.
The students at institutions 3 and 4 (n = 98) were given an additional self-assessment question in the questionnaire, where they were asked about the extent to which they believed that nurses can influence the use of antibiotics. This was not included in the total score.
Part 2 – knowledge questions
This part consisted of 34 knowledge questions. The questions were grouped into six competency areas: appropriate antibiotic use (ten questions), infection control (five questions), resistance (four questions), antibiotic consumption (nine questions), urinary tract infection and asymptomatic bacteriuria (five questions), and allergies and adverse effects (one question). The maximum score for the knowledge questions was 42.
Six of the questions had multiple correct answers, resulting in a higher possible maximum score than the total number of questions. This allowed for an additional eight points. Two questions had the response alternatives ‘Yes’, ‘No’ and ‘Don’t know’, 18 were multiple-choice questions, also with the option of ‘Don't know’, and 14 had the response alternatives ‘True’ and ‘False’.
Validity and reliability
To strengthen the questionnaire’s validity and reliability, those guiding the development of the questionnaire had expertise in antibiotic use and questionnaire methodology. They provided input on the content, design and formulation of questions.
The questions were based on the expected knowledge level of third-year nursing students, the teaching materials, the regulations on national guidelines for nursing education (11) and the national clinical guidelines for antibiotic use in primary and specialist health care (26, 27). The validity of the questionnaire content was thus confirmed and based on an expert consensus (25). The questionnaire was tested on representative users by two nursing students, who provided feedback on the content, wording and time usage.
Analysis
The data from the questionnaire were entered in the statistical program SPSS, version 27 by the first author. The first and last author carried out regular checks during this process and performed a comprehensive check of the complete dataset to identify errors or omissions prior to analysis. A small proportion of participants did not answer some of the questions. These were coded as missing values and were excluded from further analysis. For each of the six different competency areas, a total score was calculated for each participant. Results exceeding 60% of the possible maximum score were defined as an acceptable level of competence.
For the knowledge questions, correct answers were recoded as 1 and incorrect answers were recoded as 0. We analysed the background data and nursing students’ self-assessed knowledge and knowledge levels using descriptive analyses. The variables ‘Self-assessed knowledge level’ and ‘Actual knowledge level’ were normally distributed.
We therefore used t-tests and bivariate correlation analyses to assess the correlation between actual knowledge and self-assessed knowledge and the background variables previous work experience in the health service before commencing the nursing education (Yes/No) and voluntary or compulsory education. We used ANOVA to test differences between the educational institutions and age categories. All analyses were performed in collaboration with a statistician and in accordance with Norman 2010 (28). P-values < 0.05 were considered statistically significant.
Ethics
The study was submitted to the Norwegian Centre for Research Data, which confirmed that it was not subject to notification as it solely entailed processing anonymous information that could not be traced back to individuals. The data were collected in a printed questionnaire. The students were given written information about the purpose of the questionnaire survey. Responding to the questionnaire was considered to indicate their consent to the data being published. The students were informed that participation was voluntary.
Results
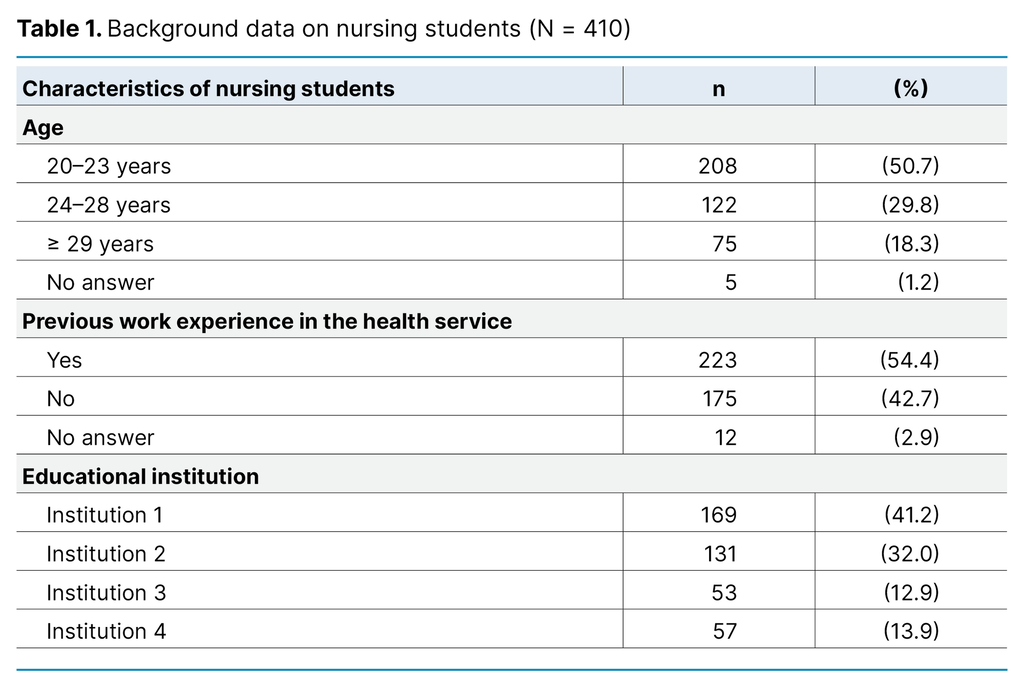
Of the 480 nursing students invited to participate, 410 responded to the survey. This corresponds to a response rate of 85.4%. The majority of respondents were in the youngest age category (20–23 years), and 54% had work experience from the health service before starting their bachelor’s degree (Table 1).
Self-assessed knowledge
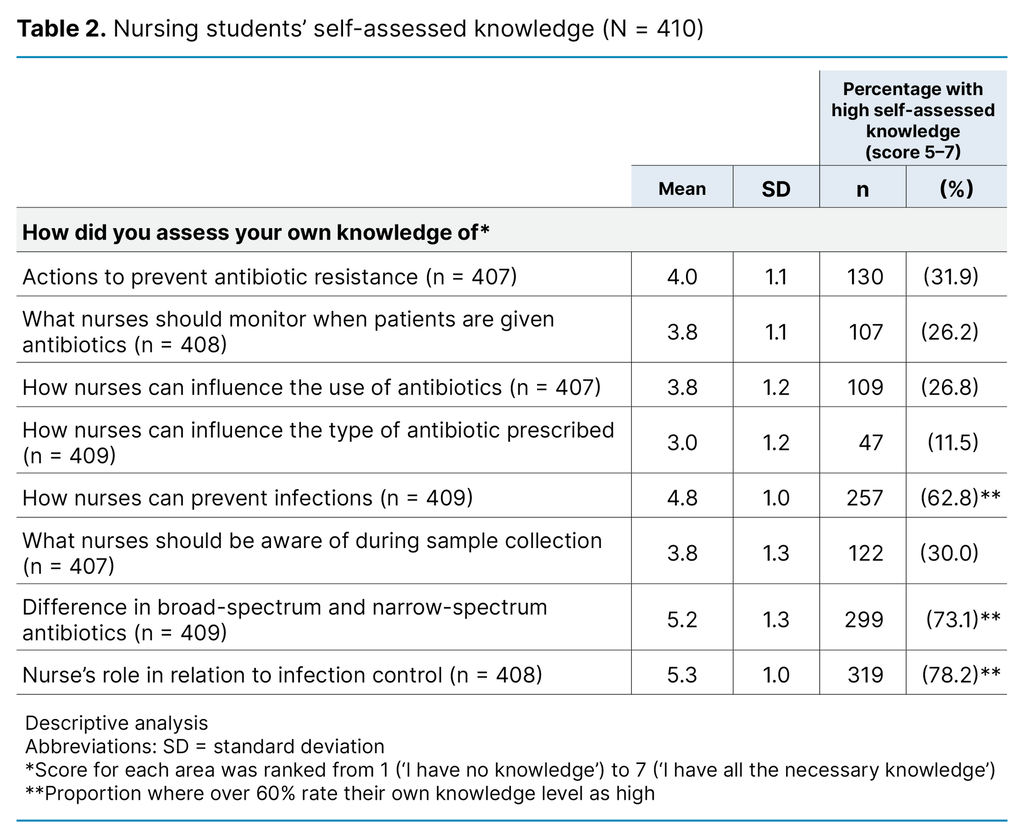
On five out of eight self-assessment questions, less than 32% of students rated their own knowledge level as high. On three self-assessment questions related to infection control, the difference between broad-spectrum and narrow-spectrum antibiotics, and infection prevention, over 60% rated their own knowledge level as high (> 5) (Table 2).
A total of 98 students answered the self-assessment question about the extent to which they believed nurses could influence the use of antibiotics in primary and specialist health care, and 76.5% rated their own ability to exert influence as high (> 5).
Nursing students’ knowledge levels
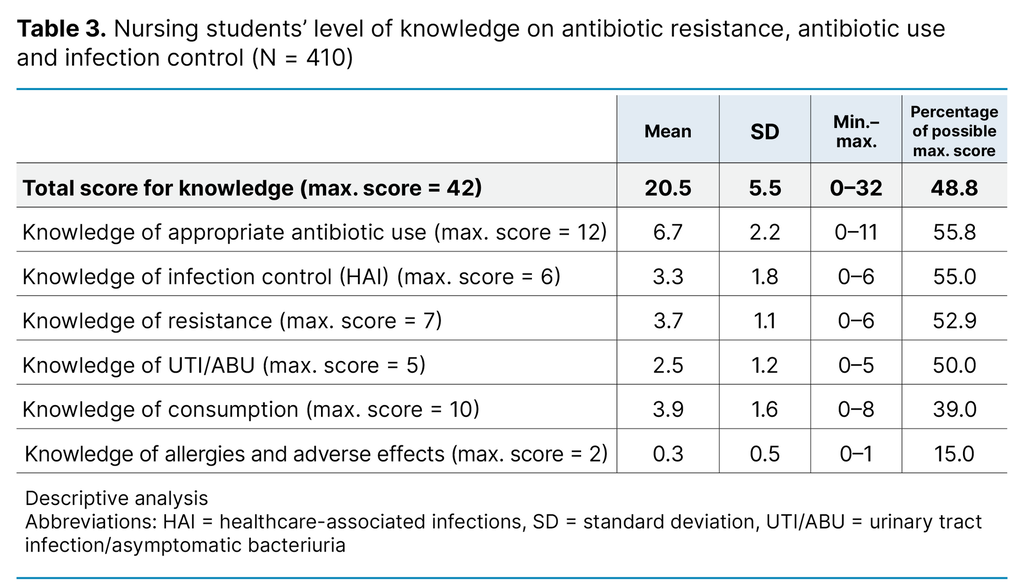
The students’ averaged 48.8% correct answers. They were least knowledgeable about antibiotic consumption, urinary tract infection and asymptomatic bacteriuria, as well as allergies and adverse effects. For the remaining topics of antibiotic resistance, appropriate antibiotic use and infection control, the students’ highest correct answer rate was between 52.9% and 55.8% (Table 3).
Correlation between self-assessed knowledge level, measured knowledge level and background variables
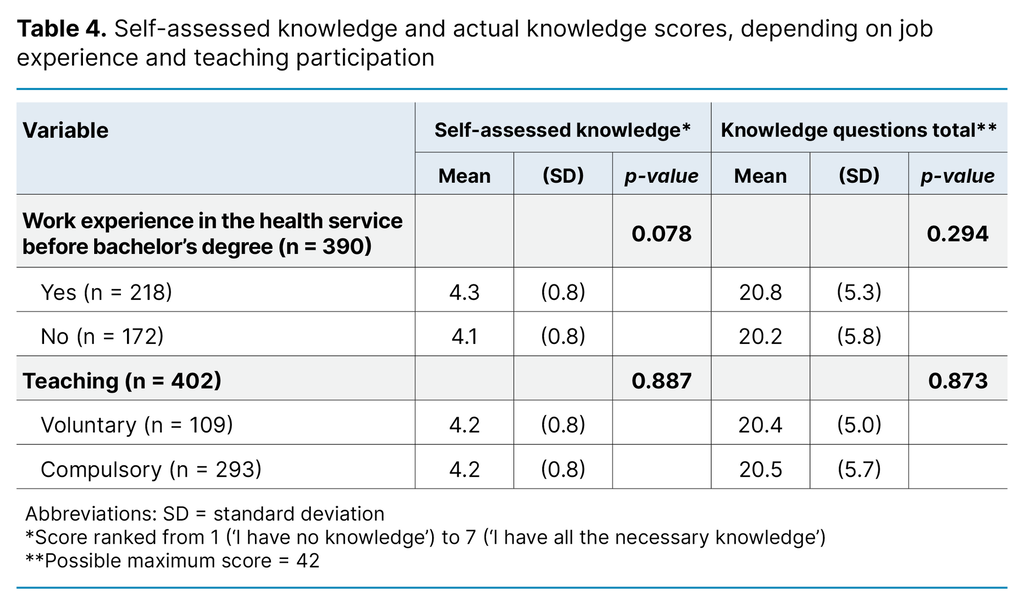
Bivariate correlation analysis showed a correlation between actual knowledge level and self-assessed knowledge level (correlation coefficient (R2) 0.238; p < 0.001). The higher the students scored on actual knowledge, the higher their self-assessed knowledge. Previous work experience in the health service before starting their bachelor’s degree and whether the teaching was voluntary or compulsory had no impact on either self-assessed knowledge or actual knowledge level (Table 4).
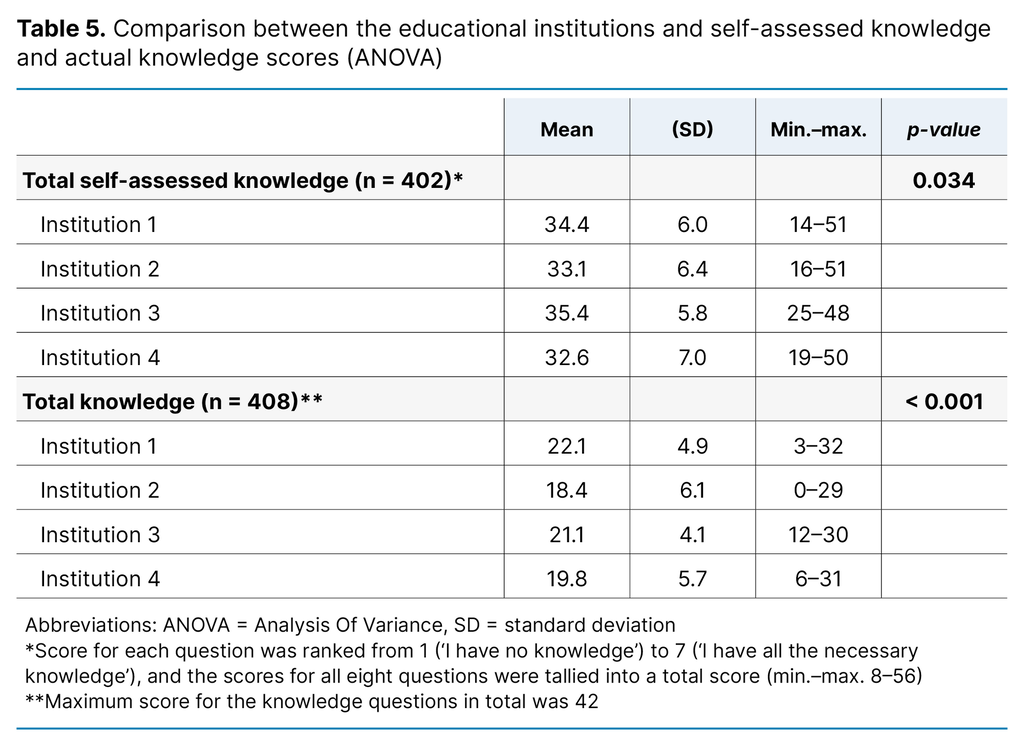
Furthermore, there was a difference in students’ self-assessed knowledge at the various institutions (p < 0.034), and in the total score for knowledge questions (p < 0.001) (Table 5).
For the measured knowledge level, there was no difference between the different age groups. ANOVA comparisons of self-assessed knowledge (p = 0.017) across the different age groups indicated that this increased with age. The oldest group’s self-assessed knowledge was the highest (mean: 35.47; standard deviation [SD] 6.79), while the youngest group’s was the lowest (mean: 33.04; SD 5.85).
Only 53 (institution 3) of the 410 students were second-year students. There was no difference between second-year and third-year students in the total score for actual knowledge and self-assessed knowledge.
Discussion
In this study, nursing students scored low on the knowledge questions and rated their own knowledge of antibiotic resistance, appropriate antibiotic use and infection control as low. There was therefore concordance between self-assessed knowledge and actual knowledge.
Self-assessed knowledge and nursing role
A high proportion of students in the study rated their own knowledge as low. Furthermore, the students believed they are in a position to influence antibiotic use. This finding is consistent with a British study, which demonstrates that nursing students believe they have a role to play in antibiotic stewardship but are unsure how they can contribute (23). Similar results were found in a Norwegian study, which showed that nurses have some understanding of antibiotic stewardship but feel uncertain about their role and responsibilities in this area (29).
Basic nursing care entails vital antibiotic stewardship tasks. Nurses are therefore a pivotal and critical occupational group in antibiotic stewardship (13). Raising students’ awareness of their role through practical training and education is crucial as it empowers them to positively impact antibiotic use, contributing to the prevention of resistance development. There is also evidence that nurses have considerable power and authority in medical decisions and can positively impact prescribing doctors’ choices in relation to the prevention of antibiotic resistance (30). However, this requires nurses to have the necessary knowledge and experience and to know how to use this to positively impact antibiotic treatment (30).
The nursing students in this study indicated that they lacked knowledge on these areas. Since all the students had practical experience in both primary and specialist health care, it may be that they had not acquired enough knowledge on the topic during their clinical placements. This suggests a need for more emphasis in nursing education to prepare and raise awareness of the nurse’s role in antibiotic stewardship. This could help expedite nursing students’ competence enhancement and make them feel more confident in their role in relation to rational and appropriate antibiotic use in future professional practice.
Nursing students’ knowledge levels
On average, the students had less than 50% correct answers across all six competency areas, indicating a general knowledge deficit in relation to antibiotic resistance and use. The topics with the lowest scores were knowledge about antibiotic consumption, urinary tract infection and asymptomatic bacteriuria. Understanding consumption can help raise awareness among students that elevated usage can lead to increased resistance (7, 8), thereby motivating them to contribute to change.
A recent study shows that urinary tract infections account for a large proportion of antibiotic use in the older population. Furthermore, the basis for treatment is often precarious, as non-specific symptoms are frequently attributed to a urinary tract infection, even in the absence of specific symptoms from the urinary tract (31). The study also showed that antibiotic consumption in nursing homes could be halved without compromising patient safety, and that teaching materials help to enhance students’ knowledge and reduce unnecessary antibiotic use. Incorporating additional content about urinary tract infections into the curriculum has considerable clinical relevance as nurses possess the ability to exert influence through infection prevention, symptom assessment and diagnostic testing, which in turn can impact on the prescription of antibiotics.
Occupational competence is vital for providing professionally responsible nursing care (32). The knowledge deficit in relation to antibiotic use could impede the delivery of responsible nursing care in the field. These findings are consistent with results from other international studies (12, 23, 33) that have identified similar knowledge gaps, underscoring the importance of raising healthcare personnel’s awareness and enhancing their engagement in addressing these issues (24). There is also other evidence that they need more education and knowledge (12, 23).
All the students in the study had completed all or part of their clinical placement in a hospital setting or in primary care and probably had some knowledge of antibiotics and antibiotic resistance at the time of completing the questionnaire. This could explain why there was no difference between second-year (n = 53) and third-year (n = 357) students in terms of either self-assessed knowledge or actual knowledge.
Earlier research emphasises the need to better incorporate knowledge about antibiotics and antibiotic resistance into the existing nursing curriculum (12, 23, 33). Such knowledge could provide recently qualified nurses with a solid foundation for utilising their position and nursing influence to prevent and reduce antibiotic resistance (23).
The results of the study therefore suggest that a stronger focus is needed on this topic in the Norwegian bachelor’s degree in nursing to better prepare students for the crucial role they will assume in promoting appropriate antibiotic use and antibiotic stewardship.
Self-assessed knowledge and correlation with actual knowledge
The results showed that the higher the students scored on knowledge, the higher they rated their own knowledge. This finding suggests that the level of actual knowledge impacts on the students’ self-confidence and self-assessed knowledge level. The finding is therefore not consistent with other research, which has demonstrated that students may have a tendency to overestimate themselves and their own skills (34).
Realistic self-assessments of future nurses’ level of competence will boost the quality of nursing care and patient safety. In this sense, these findings from the Norwegian context are reassuring.
Institution a contributing factor in knowledge level
There were differences between the educational institutions in terms of self-assessed knowledge level and actual knowledge level. However, the differences were too small to be considered of any practical significance. The institutions adhere to the same regulations in order to ensure a uniform academic standard throughout Norway (11). The results can thus be interpreted to mean that the focus on antibiotic use and antibiotic resistance needs to be strengthened across all educational institutions.
To the best of our knowledge, none of the educational institutions’ learning outcomes in the academic year 2019/2020 were directly related to antibiotic resistance, use or stewardship, which may partly explain the results of our study. This finding is supported by international literature, which shows that few educational institutions have incorporated this topic into their curriculum (22). This highlights the need for more content on this in the curriculum in order to boost nurses’ competence levels (12).
The regulations on national guidelines for nursing education, which came into effect in the academic year 2020 (11), emphasise that candidates shall have knowledge of antibiotic use and the development of resistance. The focus on this in nursing education has therefore been strengthened in Norway. Consequently, the results from our study can be used to investigate whether there is a difference in the knowledge levels of nursing students before and after the introduction of the regulations at the educational institutions in this study.
Strengths and limitations
The large sample (n = 410) and high response rate (85.4%) strengthen the internal validity of the study and may represent high quality in the statistical analyses and potential to generalise the results (25). The absence of power calculations beforehand, however, represents a weakness of the study. Another weakness is that the sample only consisted of educational institutions from south-east and south-west Norway, which may affect the generalisability to other regions. However, the fact that all institutions in Norway adhere to the same regulatory framework may increase generalisability (11). A third weakness is the use of a non-validated questionnaire due to our inability to find validated questionnaires on the topic that could address our research questions. This weakness poses a threat to validity, as it may have resulted in the questions not measuring what was intended (25).
Furthermore, the educational institutions have considerable autonomy to determine the exact content of the education, and it is therefore uncertain how much the participants were taught about the topic in their studies. We are also uncertain about whether the questionnaire captures the knowledge level of nursing students in Norway in relation to antibiotic use and resistance.
A fourth weakness is that some questions in the questionnaire had multiple correct answers, making the statistical analyses challenging. If the questionnaire is to be used in other studies, it should be refined based on the findings from this study.
The questionnaire was developed with input from experts and pilot-tested by nursing students, which is a strength of the study.
Conclusion
The results show that nursing students have insufficient knowledge about antibiotic resistance and appropriate antibiotic use, and that they also rate their own knowledge and competence as low. There was no correlation between age, previous work experience, voluntary or compulsory teaching and knowledge level. The findings therefore support the need to strengthen the focus on knowledge about antibiotics and antibiotic stewardship, as described in the new regulations for nursing education (11).
Improving teaching on the topic can help ensure that future nurses have the understanding, knowledge and awareness necessary to contribute to appropriate antibiotic use and thus have a real impact. It could give newly qualified nurses a better foundation for utilising their position and nursing influence to actively contribute to interdisciplinary efforts to prevent and limit antibiotic resistance. In doing so, they can maintain patient safety (20) and help ensure the efficacy of antibiotics in the future.
In order to investigate whether strengthening the focus on the topic actually leads to change, a similar study can be conducted to see if the knowledge level has improved since increasing the content on antibiotic resistance and use in the curriculum at many institutions. Prior to any new study, the questionnaire should be further developed based on our experience from this study, and consideration should be given to using validated instruments from other studies in a Norwegian context (12).
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge









Comments