Physical activity and health literacy in people with familial thoracic aortic aneurysm and dissection
People with genetic aortopathies should be given information on their diagnosis and support to find safe, enjoyable activities. Many also need psychosocial support.
Background: Most people with familial thoracic aortic aneurysm and dissection (FTAAD) are advised to restrict physical activity because raised blood pressure can increase the risk of acute aortic dissection due to the weakening of connective tissue in the blood vessel walls. Living with a potentially life-threatening illness such as FTAAD can often be worrying and challenging.
Objective: The objective was to generate new knowledge about the experiences and perceptions of people with FTAAD, and how they deal with the challenges they face in relation to physical activity.
Method: A cross-sectional study with a mixed methods design, and a combination of results from qualitative focus group interviews (n = 36) and a quantitative survey (n = 52). The sample consisted of people with a genetically verified diagnosis of FTAAD: Marfan syndrome, Loeys-Dietz syndrome and vascular Ehlers-Danlos syndrome.
Results: The survey showed that most participants (85%) had received advice on physical activity, with an emphasis on certain restrictions. They had modified and reduced their physical activity, and 40% were less active than recommended. Symptoms of anxiety (94%), pain (79%) and fatigue (58%) were prevalent. We found that both increasing anxiety and increasing fatigue showed a significant association with a lower level of physical activity. In the focus group interviews, many participants reported that it was difficult to put the advice into practice, resulting in a sedentary lifestyle. Finding a balance between activity that promotes good health and activity that is harmful seemed to be a challenge for many. There are strong indications that how healthcare personnel interact with and convey advice on physical activity and restricting activity to this group are key to such patients acquiring the necessary health literacy.
Conclusion: It is crucial that professionals who treat people with FTAAD are aware of the challenges they face. More knowledge about which activities and types of exercise promote good health can help such patients to establish safe activity habits, improve their health literacy and give them new life skills.
Familial thoracic aortic aneurysm and dissection (FTAAD) is the umbrella term for a group of heritable connective tissue disorders with a high risk of dilation and aneurysm or dissection in the main artery (aorta) due to weakened connective tissue (1).
The most common disorders include Loeys-Dietz syndrome (LDS), vascular Ehlers-Danlos syndrome (vEDS) and Marfan syndrome (MFS). The presence of connective tissue throughout the body means that several organ systems can be affected, including the cardiovascular system, musculoskeletal system, internal organs and the eyes. The symptoms of the different FTAAD diagnoses overlap to some degree, but can present differently and in different combinations, and can develop over time (1).
In Norway and internationally, people diagnosed with FTAAD are typically given advice on restricting physical activity and exercise. This is because raised blood pressure during physical activity can increase the risk of acute aortic dissection due to the weakening of connective tissue in the blood vessel walls. Antihypertensive medication and refraining from activity that raises the blood pressure are therefore recommended (2, 3).
The advice on physical activity is general and gives an indication of what precautions should be taken, and should therefore be adapted to the health of the individual (2). According to international guidelines, most people can participate in aerobic exercises with light to moderate intensity, such as cycling, running, swimming and dancing. They should avoid collision sports, extreme sports, static exercises, maximum endurance testing and strenuous physical activity during which they are unable to breathe and speak simultaneously (2–4).
A recently published Norwegian literature review on physical activity in FTAAD diagnoses shows that few primary studies have been conducted in this area (5). However, three international reviews (2, 6, 7) on physical activity in FTAAD patients indicated that physical activity is important for good health and for preventing a sedentary lifestyle (5).
The musculoskeletal system is often affected, typically in the form of overactive joints and skeletal malformations (1, 8), chronic pain (8, 9), and anxiety (10, 11), severe fatigue (10, 12) or reduced quality of life (11, 13). Many also face challenges at work (8, 11, 12) and have difficulty finding suitable forms of physical activity (5).
Little is known about how people with FTAAD perceive the recommendations on physical activity and how they apply the advice in practice (5). Relevant health information and health literacy are crucial for making knowledge-based decisions in the self-management of illness and physical activity (14).
Objective of the study
The objective was to form an overview of the challenges people diagnosed with FTAAD face in relation to physical activity. We also wanted to gain in-depth knowledge about their experiences with and management of the challenges in their daily life.
We posed the following research questions:
- Do people with FTAAD face challenges in relation to physical activity, and if so, what are these?
- What are the experiences with physical activity and exercising and how are they managed?
- How important are information and health literacy for how they deal with the challenges in relation to physical activity?
Method
In this mixed methods study (15, 16), we included a cross-sectional sample consisting of adults with an FTAAD diagnosis (LDS, vEDS, MFS). The focus group interviews were held first and formed the basis for the survey. We then summarised and synthesised the results.
Study protocol
The article is part of a large research project on psychosocial factors and physical activity in people with FTAAD: LDS, vEDS and MFS. The project was approved by the Regional Committees for Medical and Health Research Ethics (REC South East Norway, reference number 2017/745). All participants received written information about the study and signed an informed consent form. Participation was voluntary.
Service user involvement in the project
A reference group consisting of three service user representatives, Kari Anne Hove Sørli, Roald Sørmoe and Elin Schau, was appointed. This group was involved in the entire research process, ethical considerations and drafting of the protocol, questionnaire and interview guide.
The reference group actively contributed to the analysis and combining of results, and was involved in the discussion about the article’s structure, content and design. We held several in-person and remote meetings and also communicated via email. As researchers, we found service user representatives’ involvement to be very beneficial, as they expanded our understanding, provided new perspectives and assured the quality of our analyses and presentation of results.
Participants
In connection with two service user meetings in 2017 and 2018, we conducted focus group interviews of adults diagnosed with FTAAD. A total of 36 people participated (LDS = 11, vEDS = 11, MFS = 14).
In the autumn of 2018, we sent the questionnaire to all adults over the age of 18 with LDS and vEDS (n = 70). A total of 52 people responded (response rate of 74%) – 34 with LDS and 18 with vEDS completed the questionnaire and signed the informed consent form.
We did not survey people with MFS because a similar survey had recently been conducted (9–11). Only one participant (LDS) in the focus group interviews did not answer the questionnaire.
Qualitative data
We developed a semi-structured interview guide based on our clinical experiences, research and collaboration with the reference group. The participants were divided into six focus groups: two for each diagnosis (five to seven participants).
Our emphasis was on heterogeneity in age, sex, education and employment within each focus group. The objective was to generate new knowledge about the participants’ experiences with and perspectives on physical activity and restrictions on activity. In addition to the first authors, six other people were involved as moderators and co-moderators in the focus groups.
Both these and the first authors are professionals with many years of clinical and/or research experience with the diagnostic categories. All had completed an internal training programme on focus group interviews, with a focus on interview techniques, group communication and pre-understanding.
The focus group interviews were audiotaped and lasted between 2 and 2.5 hours. The first authors transcribed the interviews and analysed them using systematic text condensation, based on Giorgi’s phenomenological analysis, which is well-suited to focus group interviews (17).
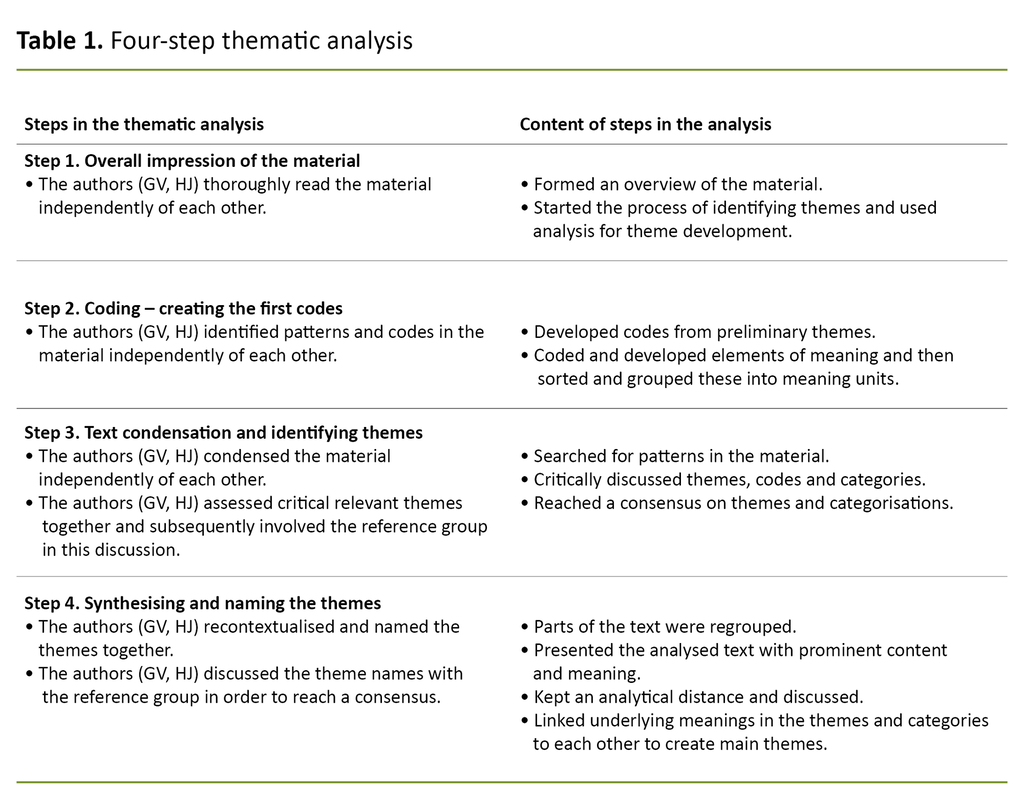
We used a four-step thematic analysis: 1) overall impression of the material, 2) coding, 3) text condensation, and 4) synthesising (see Table 1). The first authors carried out the initial analyses independently of each other. Interpretations and disagreements were then discussed with the reference group, which was also involved in the further analysis. We followed the recommended consolidated criteria for reporting qualitative research, COREQ (18).
Quantitative data
Based on the results from the focus group interviews and in collaboration with the reference group, we devised a study-specific questionnaire consisting of questions about demographic and medical factors. We also included the following validated instruments:
- Fatigue Severity Scale (FSS) – a widely used instrument that measures the impact of fatigue. A 9-item questionnaire with a 0–7 point scale (19).
- Standardised Nordic Questionnaire – including a question that detects the existence of chronic pain lasting more than three months (Yes/No) (20).
- The Hospital Anxiety and Depression Scale (HADS) – a widely used instrument that measures symptoms of anxiety (HADS-A) and depression (HADS-D), with seven items for each scale, and a 0–3 point scale (21).
The instruments have been translated to Norwegian and validated for use in the Norwegian setting (22–24).
We also included a further six questions on physical activity and exercise from the HUNT survey (25).
We used descriptive statistics to present demographic, clinical and validated data from the questionnaire. In the analysis of associations between different variables, we used bivariate analysis and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (26).
Combining the data
The two sub-studies were first analysed individually, then using a mixed methods approach (16), with the main emphasis on analysing, integrating and synthesising the results from the sub-studies. The aim of synthesising the data from the sub-studies was to provide a broader and more in-depth understanding of the participants’ experiences with and management of challenges they faced in relation to physical activity.
We used the themes that emerged in the analysis of the focus groups as a starting point, and collocated the results from the sub-studies. We indicated which sub-study the results originated from.
Results
The participants
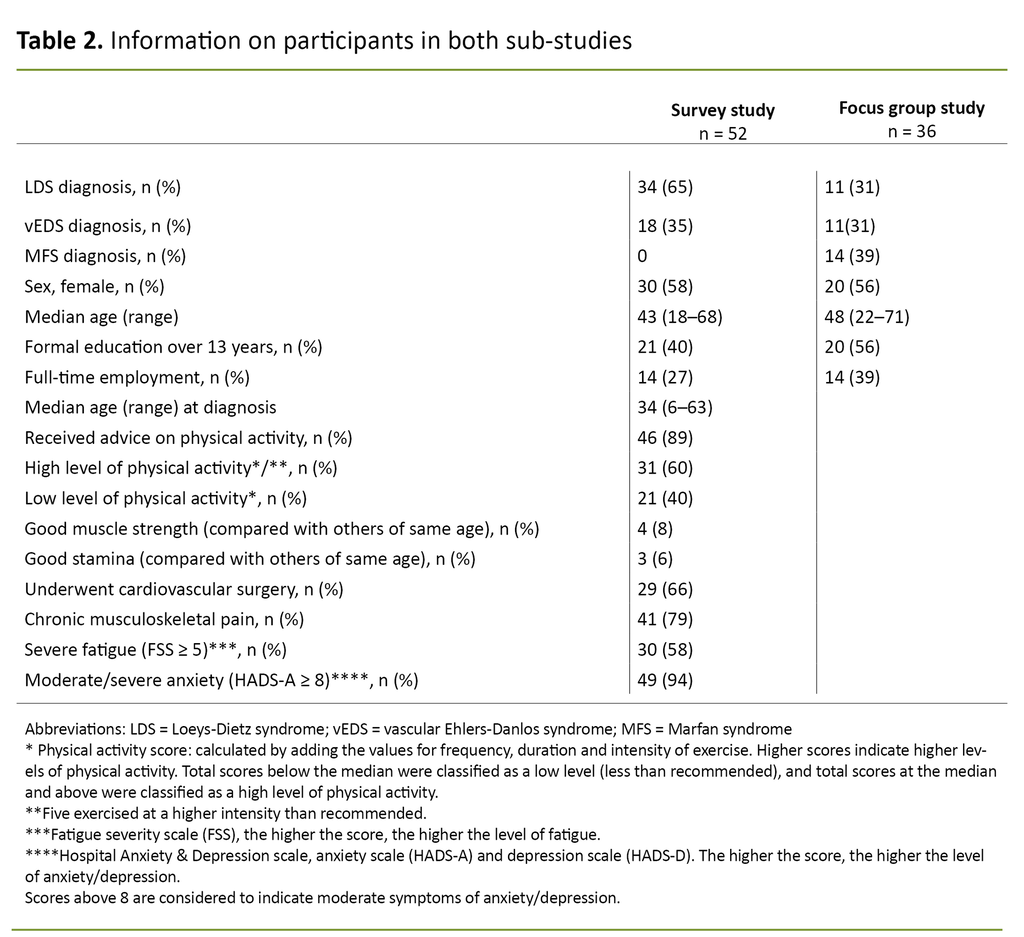
Table 2 gives an overview of the participants in both sub-studies. A relatively high proportion had more than 13 years of education, and relatively few worked full-time.
Synthesising the quantitative and qualitative data
The findings from the sub-studies are grouped under four main themes originating from the qualitative analysis: 1) Life change – receiving a potentially life-threatening diagnosis, 2) Interaction with healthcare personnel – receiving advice on restricting activity, 3) Finding a balance – putting the advice into practice, and 4) How to manage it – wishes for the future.
Life change – receiving a potentially life-threatening diagnosis
The mean age at diagnosis was 34 years (see Table 2). In the focus groups interviews, it emerged that the diagnosis led to changes in a number of areas of life. The changes included restrictions on physical activity, recommended use of medication for hypertension and regular medical check-ups. They were also afraid of aortic complications and that other family members would be diagnosed. Many described a sense of grief because the absence of a curative treatment meant that they could never return to ‘normal life’.
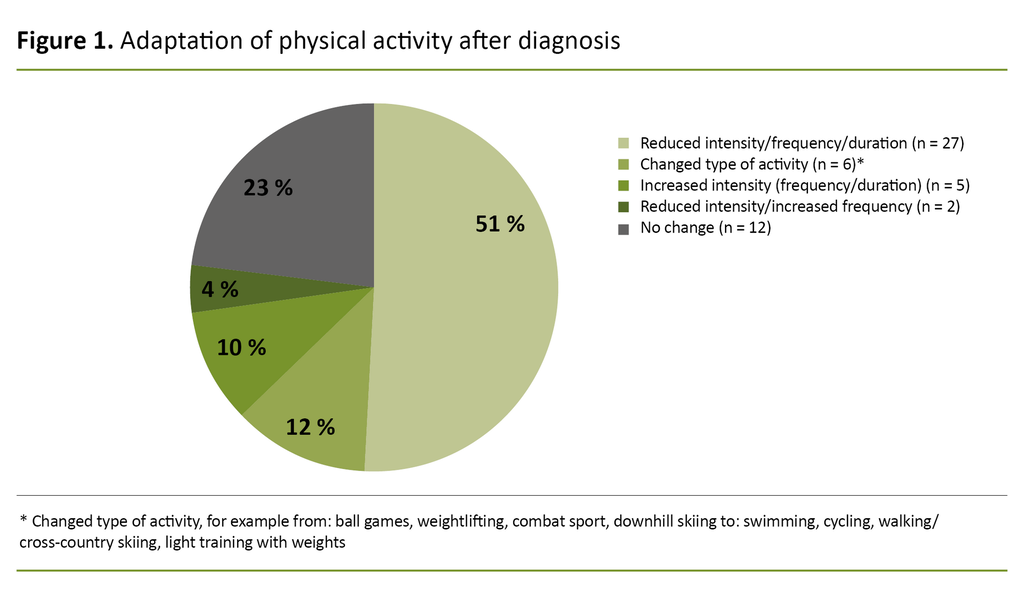
51% reduced their physical activity after receiving the diagnosis
Results from the survey showed that 51% reduced their physical activity after receiving the diagnosis (see Figure 1). The proportion of participants who were physically active on a daily basis fell from 39% before receiving the diagnosis to 17% after receiving the diagnosis and being advised to comply with specific restrictions on physical activity.
In the focus group interviews, many described how they had to change their perception of ‘exercising’. What they previously had considered to be good for their health could now be harmful.
This was particularly difficult for the young adults who had recently been diagnosed: ‘The contrast was huge for me. I used to do high-intensity training almost daily and loved to compete. It was fantastic to get my heart rate up, train hard and feel in good shape. I never thought it could harm my body’ (young man with vEDS).
Interaction with healthcare personnel – receiving advice on restricting activity
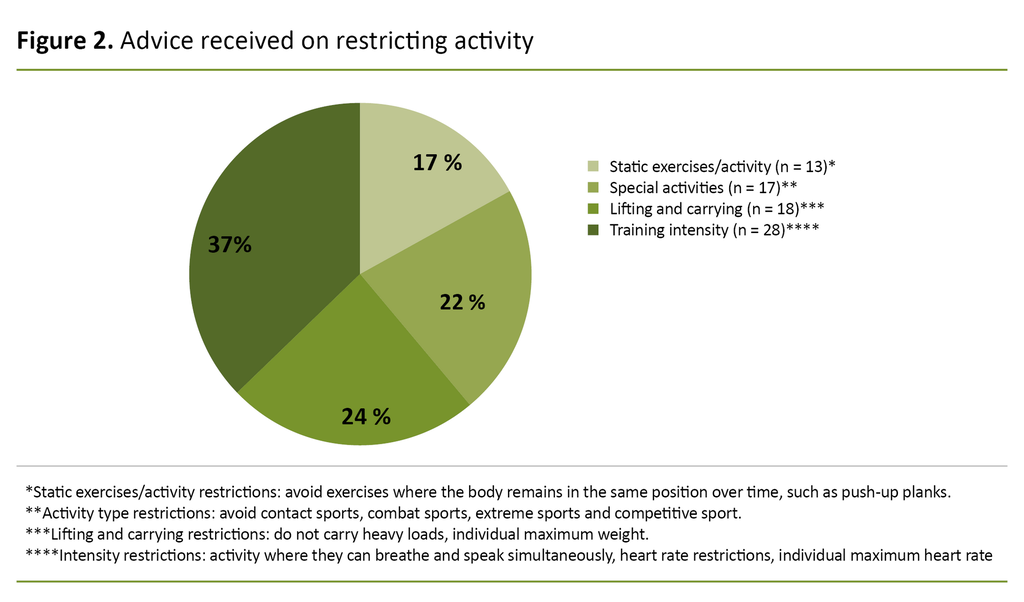
A total of 89% of the survey participants had received advice on restricting physical activity following diagnosis (see Table 2). The restrictions related to training intensity (37%), lifting or carrying (24%), static exercises (17%) and certain types of physical activity, such as collision sports, extreme sports or competitive sport (22%) (see Figure 2).
Most participants in the focus groups also confirmed that they had received advice on restricting activity. One challenge was that the recommendations tended to focus on limitations as opposed to possibilities: ‘It’s difficult to take everything in when you’re in shock. I felt overwhelmed, depressed and confused. I wish the healthcare personnel had had more time. I felt like I had so many unanswered questions when I left’ (a middle-aged woman with LDS).
The participants’ interaction with healthcare personnel seemed to be pivotal to how they dealt with physical activity and exercise. Many felt it was important that the information was adapted to their situation, and that they be given the opportunity to test out physical activity and time to ask questions. They expressed that they needed help to find the right level of activity.
There are strong indications that healthcare personnel can play an important role in improving the health literacy of this patient group through tailored information and support to find enjoyable physical activities.
Finding a balance – putting the advice into practice
Almost half of the survey participants reported that their stamina and muscle strength was poorer than that of their peers. Only 8% reported ‘good’ muscle strength, and 6% reported ‘good’ stamina (Table 2).
A large majority (77%) had changed their physical activity habits (Figure 1), 40% exercised less than recommended (low activity level), and about 10% exercised at a higher intensity than recommended (Table 2).
It was difficult to remain motivated over time when it had little effect.
In the focus group interviews, it emerged that most participants were motivated to exercise, but it was difficult to remain motivated over time when it had little effect. The young adults in particular were concerned with ‘building muscle’, which could be incompatible with the recommendation to exercise at a moderate level. Some chose to ignore the advice and exercised harder than recommended, while others stopped exercising: ‘What’s the point when I can’t exercise in the same way as my friends, I’m always left out and different’ (young man with LDS).
Others described problems with staying motivated and maintaining continuity in activity due to repeated interruptions because of pain, fatigue, hospital stays for operations and convalescence.
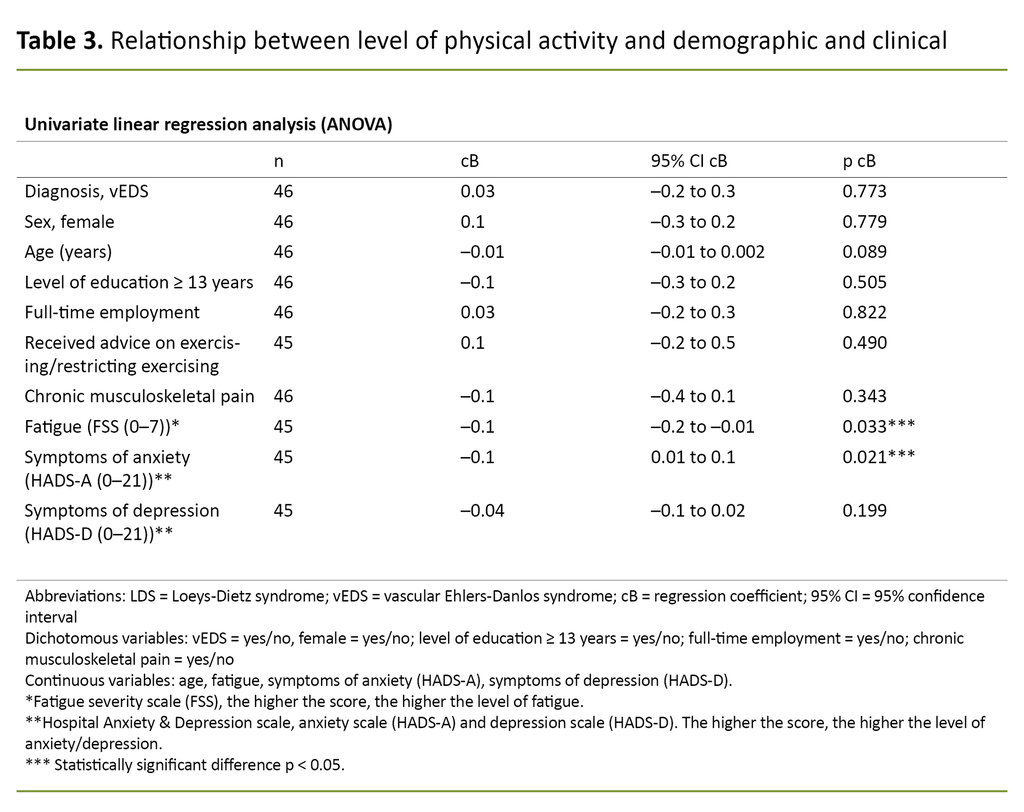
The survey showed that the majority suffered chronic pain (79%) and fatigue (58%) (Table 2). Severe fatigue was significantly correlated with lower levels of physical activity (Table 3).
This finding was also confirmed in the focus groups, and was a trigger for them entering a downward spiral with reduced physical activity, increased fatigue and pain: ‘Repeated interruptions due to pain and surgery make me weary: having to constantly start over and over again isn’t easy’ (middle-aged lady with LDS).
The survey showed that 94% had symptoms of anxiety and 77% had symptoms of depression (Table 2). Higher anxiety levels were also associated with lower levels of physical activity (Table 3).
The participants in the focus groups described their concern about whether they were exercising properly.
The participants in the focus groups described their concern about whether they were exercising properly. Constantly being on the lookout for signals from their body, palpitations, chest pains and irregular heartbeats made them feel uneasy and anxious.
For some, it was paradoxical that they avoided physical activity because of the fear of medical complications, while also being aware that physical activity was good for their health: ‘I have to exercise, it’s important for my body, but I also know that it can be dangerous. In fact, I feel anxious at times, and having to listen to my body all the time is exhausting, and often makes me want to skip exercising because it’s a constant reminder that I’m different’ (young man with LDS).
How to manage it – wishes for the future
The survey showed that only 9 out of 52 people reported being given the opportunity to explore new physical activity habits within a safe framework during in-patient rehabilitation. A total of 32% (n = 16) reported a need for rehabilitation with psychosocial support and tailored advice on physical activity.
In the focus groups, the participants were concerned with personal responsibility, but at the same time expressed a need for psychological and practical support from professionals. They wanted concrete advice, help to find out which exercises would promote good health, and help to master their anxiety in relation to exercising.
The participants were particularly interested in the possibility of interdisciplinary rehabilitation in connection with the diagnosis, after surgery and in periods with considerable pain and fatigue: ‘I wish there was a support system and someone who could tell me what is safe and what works well. I need someone who understands my situation and can help me feel safe’ (a young woman with vEDS).
Discussion
The study shows that people with FTAAD face major challenges in relation to physical activity. There are strong indications that the interaction with healthcare personnel and the way they convey advice on physical activity and restricting activity impacts on how the group acquires the necessary health literacy.
Despite researchers’ and clinicians’ awareness of the major challenges faced by those with FTAAD in terms of physical activity, empirical research is limited (2, 5–7). There is agreement that people with FTAAD should be physically active and advised to exercise regularly at a light to moderate pace (2, 5–7), but our study shows that many reduce their activity level and exercise less than recommended.
Uncertainty impacts on the advice from healthcare personnel
Although the disorders are genetic, most of our study participants were diagnosed in adulthood, with a mean age of 34 years for people with LDS and vEDS, and 22 years for MFS (12). The diagnosis came as a shock for many – changing their lifestyle in adulthood was a challenge, and they struggled to put the advice on physical activity into practice.
Most had received information about the condition and advice on physical activity. Nevertheless, they were concerned that the recommendations mainly focused on limitations as opposed to possibilities. Uncertainty about the association between raised blood pressure during physical exercise and aortic complications can impact on the advice given by healthcare personnel, according to Braverman et al. (3).
According to Cheng et al. (2), the lack of evidence-based knowledge makes advising patients with FTAAD about lifestyle changes and restricting physical activity challenging for healthcare personnel. Many participants described how they were anxious about physical activity, and how it was difficult to find a balance between what was good for their health and what was harmful. This dilemma has also been described in other studies (27).
Lack of concrete advice can lead to inactivity
The degree of anxiety and fatigue seemed to be negatively associated with the participants’ level of physical activity. Uncertainty and lack of concrete advice can lead to inactivity and negative consequences, such as muscle atrophy, joint stiffness, poor fitness, increased pain and fatigue, as well as reduced psychosocial functioning (28).
Uncertainty and lack of concrete advice can lead to inactivity.
Jensen et al. (7) have a strong focus on the importance of improving health literacy among people with FTAAD, and believe that they should be given realistic and practical information about the benefits as well as health risks of physical activity. Research shows that improving patients’ health literacy gives them a greater sense of security, more control and a better quality of life (14).
Many need help to recognise possibilities
In our study, many participants needed more nuanced information and help to recognise possibilities, not just limitations. Fugelli and Ingstad (29) emphasise the importance of ‘happy health’ in health-promoting work, as opposed to information characterised by a negative perspective with warnings and risks.
We therefore assume that receiving concrete, realistic and optimistic information shortly after being diagnosed with FTAAD can reduce anxiety, both in relation to physical activity and poorer health status.
People with these disorders should be offered closer follow-up in periods when they are trying to find new ways to cope and new activity habits, and trying to adapt their levels of physical activity. This can help them to understand, evaluate and apply the health advice they receive, thereby improving their health literacy.
Professionals such as nurses and other healthcare personnel play an important role in motivating and helping people with FTAAD to cope with living with a potentially life-threatening illness (5, 10, 30).
Strengths and limitations of the study
The fact that all participants had received a clinical diagnosis of FTAAD and that all regional health authorities in Norway were represented was a strength of the study. The results from the sub-studies support each other and provide complementary knowledge about the challenges faced by people with FTAAD.
In the survey, we used measuring instruments that have been validated for the Norwegian setting, and the focus group interviews were conducted by experienced professionals and researchers. We have strived to be transparent and have described in-depth the basic methodology in previously published articles (11, 30).
The sample size was small, and the results must therefore be interpreted with caution. We believe that the study provides important knowledge about the challenges and experiences among people with FTAAD in relation to physical activity and coping with daily life.
Conclusion
The study shows that 40% of the participants are less physically active than recommended despite most of them receiving advice on physical activity. Many reported high levels of anxiety, pain and fatigue that impacted on physical activity. It is important that people with FTAAD receive tailored information about their condition as well as support to find enjoyable activities.
The recommendations should not only focus on limitations, but also possibilities and opportunities for testing out recommended exercises in practice. Many therefore need closer follow-up and motivation, tailored adaptations and psychosocial support to find health-promoting activities.
We would like to extend special thanks to Kari Anne Hove Sørli, Roald Sørmoe and Elin Schau for the crucial and inspiring collaboration. Their contributions have helped to assure the quality of the content in the article and has given us as first authors and researchers a deeper and better understanding of the problem. We would also like to thank the TRS National Resource Centre for Rare Disorders for allowing us to carry out the project. Thanks also go to all the participants in the focus group interviews and the survey.
The knowledge about these groups shall remain up-to-date on the website of the TRS National Resource Centre for Rare Disorders (5). Healthcare personnel in the primary and specialist health services are encouraged to contact the centre if necessary.
First authorship is shared in this article.
The authors declare no conflicts of interest.
References
1. Meester JAN, Verstraeten A, Schepers D, Van Laer L, Loyes BL. Differences in manifestations of Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome. Ann Cardiothorac Surg. 2017;6(6):582–94. DOI: 10.21037/acs.2017.11.03
2. Cheng A, Owens D. Marfan syndrome, inherited aortopathies and exercise: What is the right answer? Postgrad Med J. 2016;50(2):100–4. DOI: 10.1136/heartjnl-2014-306440
3. Braverman AC, Harris KM, Kovacs RJ, Maron BJ. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 7: aortic diseases, including Marfan syndrome: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiology. 2015;66(21):2398–405. DOI: 10.1161/CIR.0000000000000243
4. Sunnaas sykehus. Fysisk funksjon, aktivitet og trening ved Marfans syndrom [Internet]. Bjørnemyr: Sunnaas sykehus; 27.11.2017 [updated 07.07.2020, cited 10.09.2021]. Available at: https://www.sunnaas.no/fag-og-forskning/kompetansesentre-og-tjenester/trs-kompetansesenter-for-sjeldne-diagnoser/sjeldne-diagnoser/marfans-syndrom/fysisk-funksjon-aktivitet-og-trening-ved-marfans-syndrom
5. Velvin G, Johansen H. En oversiktsartikkel om fysisk aktivitet og trening for personer med familiære thorakale aortaaneurismer og aortadisseksjoner. Fysioterapeuten. 01.12.2021. Available at: https://www.fysioterapeuten.no/fagfellevurdert-fysioterapi-hjerte-og-karsykdommer/fysisk-aktivitet-og-trening-for-personer-med-familiaere-thorakale-aortaaneurismer-og-aortadisseksjoner-en-oversiktsartikkel/138124 (downloaded 10.01.2022).
6. Thijssen CGE, Bons LR, Gokalp AL, Kimmenade RRJ, Mokhles MM, Pelliccia A, et al. Exercise and sports participation in patients with thoracic aortic disease: a review. Expert Rev Cardiovasc Ther. 2019;17(4):251–66. DOI: 10.1080/14779072.2019.1585807
7. Jensen TL, Tran P, Kjaer M. Marfan syndrome and exercise: a literature review. Trans Sports Med. 2020;3(6):526–35. DOI: 10.1002/tsm2.185
8. Johansen H, Velvin G, Lidal I. Adults with Loeys-Dietz syndrome and vascular Ehlers-Danlos syndrome: a cross-sectional study of health burden perspectives. Am J Med Genet A. 2020;182(1):137–45. DOI: 10.1002/ajmg.a.61396
9. Velvin G, Bathen T, Rand-Hendriksen S, Geirdal AØ. Systematic review of chronic pain in persons with Marfan syndrome. Clin Genet. 2016;89(6):64–58. DOI: 10.1111/cge.12699
10. Johansen H, Velvin G, Lidal I. Adults with Loeys-Dietz syndrome and vascular Ehlers-Danlos syndrome: a cross-sectional study of patient experiences with physical activity. Disabil Rehabil. 11.09.2020. DOI: 10.1080/09638288.2020.1815874
11. Velvin G, Bathen T. Rand-Hendriksen S, Geirdal AØ. Systematic review of the psychosocial aspects of living with Marfan syndrome. Clin Genet. 2015;87(2):109–16. DOI: 10.1111/cge.12422
12. Velvin G, Bathen T, Rand-Hendriksen S, Geirdal AØ. Work participation in adults with Marfan syndrome: demographic characteristics, MFS related health symptoms, chronic pain, and fatigue. Am J Med Genet A. 2015;167(12):3082–90. DOI: 10.1002/ajmg.a.37370
13. Johansen H, Velvin G, Fugl-Meyer K, Lidal IB. Adults with Loeys-Dietz syndrome and vascular Ehlers-Danlos syndrome: a cross-sectional study of life satisfaction. J Rehabil Med. 2021;53(11):jrm00239. DOI: 10.2340/jrm.v53.572
14. Helse- og omsorgsdepartementet. Strategi for å øke helsekompetansen i befolkningen 2019–2023. Available at: https://www.regjeringen.no/contentassets/97bb7d5c2dbf46be91c9df38a4c94183/strategi-helsekompetanse-uu.pdf (downloaded 31.03.2022).
15. Røykenes K. Metodetriangulering – et metodisk minefelt eller en berikelse av fenomener. Sykepleien Forskning. 2008;3(4):224–6. DOI: 10.4220/sykepleienf.2008.0081
16. Gutterman TC, Fetters MD, Creswell JW. Integrating quantitative and qualitative results in health science mixed methods research through joint display. Ann Fam Med. 2015;13(6):554–61. DOI: 10.1370/afm.1865
17. Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Pub Health. 2012;40(8):795–805. DOI: 10.1177/1403494812465030
18. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Intern J Qual Health Care. 2007;19(6):349–57. DOI: 10.1093/intqhc/mzm042
19. Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–3. DOI: 10.1001/archneur.1989.00520460115022
20. Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233–7. DOI: 10.1016/0003-6870(87)90010-X
21. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. DOI: 10.1111/j.1600-0447.1983.tb09716.x
22. Lerdal A, Wahl A, Rustoen T, Hanestad BR, Moum T. Fatigue in the general population: a translation and test of the psychometric properties of the Norwegian version of the fatigue severity scale. Scan J Public Health. 2005;33(2):123–30. DOI: 10.1080/14034940410028406
23. Svebak S, Hagen K, Zwart JA. One-year prevalence of chronic musculoskeletal pain in a large adult Norwegian county population: relations with age and gender – The HUNT study. J Musculoskelet Pain. 2006;14:21–28. DOI: 10.1300/J094v14n01_04
24. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. DOI: 10.1016/S0022-3999(01)00296-3
25. HUNT Forskningssenter (Helseundersøkelsen i Nord-Trøndelag). HUNT Databank. HUNT3 Fitness Project. Questionnaire – NT3FitnQ20 2019. Available at: https://hunt-db.medisin.ntnu.no/hunt-db/#/studypart/189 (downloaded 15.02.2020).
26. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. DOI: 10.2471/BLT.07.045120
27. Brunes A, Augestad LB, Gudmundsdottir SL. Personality, physical activity, and symptoms of anxiety and depression: the HUNT study. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):745–56. DOI: 10.1007/s00127-012-0594-6
28. Helsedirektoratet. Anbefalinger om kosthold, ernæring og fysisk aktivitet. Oslo: Helsedirektoratet; u.å. Rapport IS-2170. Available at: https://www.helsedirektoratet.no/rapporter/anbefalinger-om-kosthold-ernaering-og-fysisk-aktivitet/Anbefalinger%20om%20kosthold%20ern%C3%A6ring%20og%20fysisk%20aktivitet.pdf/_/attachment/inline/2f5d80b2-e0f7-4071-a2e5-3b080f99d37d:2aed64b5b986acd14764b3aa7fba3f3c48547d2d/Anbefalinger%20om%20kosthold%20ern%C3%A6ring%20og%20fysisk%20aktivitet.pdf (downloaded 10.09.2021).
29. Fugelli P, Ingstad B. Helse – slik folk ser det. Tidsskr Nor Lægeforen. 2001;121:3600–4. Available at: https://tidsskriftet.no/2001/12/tema-helse-og-kultur/helse-slik-folk-ser-det (downloaded 11.11.2021).
30. Velvin G, Johansen H, Vardeberg K, Fugl-Meyer KS, Wilhelmsen JE, Lidal IB. Physical exercise for people with hereditable thoracic aortic disease. A study of patient perspectives. Disabil Rehabil. 2021:43(17): 2464–71. DOI: 10.1080/09638288.2019.1703145










Comments