Is the procedure for stimulating uterine contractions during labour followed? A survey of midwives
The practice differs when midwives use medication to stimulate contractions rather than breast stimulation. Not all midwives classified the CTG or used a checklist for oxytocin stimulation.
Background: Prolonged labour is associated with an increased risk of adverse outcomes in mother and child. The Norwegian Society for Gynaecology and Obstetrics’ maternity care manual recommends contraction stimulation interventions to prevent and accelerate slow progress. The recommendations are incorporated into the health trusts’ procedures.
Objective: To map the extent to which midwives at Oslo University Hospital follow the procedure for contraction stimulation. An overview of current practice could provide a basis for identifying challenges or areas requiring improvement.
Method: A self-administered questionnaire was distributed to midwives at the maternity ward in the period May–June 2018 (n = 160).
Results: Ninety-nine midwives responded to the questionnaire (99/160; 62 per cent). Eighty-five per cent stated that they largely perform an artificial rupture of membranes when labour is not progressing. All reported that they use non-medication methods to prevent slow progression and await active pushing when the cervix is fully dilated but the fetus head is not engaged. Fetal monitoring during oxytocin stimulation was in accordance with the procedure, but not all midwives classified the cardiotocography (CTG) when there was a change in the oxytocin dose. Few midwives (14 per cent) initiated oxytocin stimulation one hour after the rupture of membranes. The oxytocin checklist for contraction stimulation was seldom used.
Conclusion: Midwives reported that the procedure for contraction stimulation is followed in several areas, but there are challenges associated with when to initiate oxytocin stimulation, the classification of CTG when changing the oxytocin dose, and the use of a checklist.
Slow progress occurs when the cervix does not dilate quickly enough, normally less than 1 cm per hour. Causes of slow progress in childbirth include fetal presentation, anatomical conditions in the birth canal, or weak and/or short contractions (1, 2). Patient anxiety and epidural anaesthesia are also associated with slow progress (3).
Around half of all primiparous women and one-tenth of all multiparous women in Norway are stimulated with oxytocin to hasten the childbirth process (4). Slow progress can pose a danger to mother and child, especially where there are anatomical abnormalities or where the uterus is weak (5). Most Norwegian maternity clinics and maternity wards therefore have a procedure in place that stipulates time limits in cases where labour is protracted.
Contraction stimulation as an intervention
Stimulating contractions using oxytocin is one possible intervention that can be performed in cases of uterine inertia where other reasons for slow progress can be ruled out (6). When used as a medication to stimulate contractions, oxytocin is mixed in a saline solution and administered through continuous intravenous infusion.
Contraction stimulation with oxytocin is associated with risk. There is a risk of a uterus rupture, especially among multiparous women who have previously had surgery on their uterine wall (7). Stimulation with oxytocin over a protracted period significantly increases this risk. The use of oxytocin on parous women is associated with a particularly high risk of fetal asphyxia (8).
Norwegian maternity wards
Oslo University Hospital (OUH) is home to the largest maternity ward in Scandinavia, with about 10 000 births per year. Parts of the maternity ward are operated from the OUH sites at Rikshospitalet and Ullevål. In 2017, 60 per cent of the primiparous women at Rikshospitalet were given oxytocin to stimulate contractions during labour. At Ullevål, the proportion was 48 per cent.
Corresponding figures for multiparous women were 20 per cent at Rikshospitalet and 8 per cent at Ullevål (9). The variation between maternity units can generally have several explanations. It may be due to random factors, centralisation of high-risk parous women, variations in reporting practices and/or differences in the quality of the maternity units. It is often a combination of several of these factors.
Objective of the study
A procedure is in place at OUH for when to use contraction stimulation, which is recommended in the Norwegian Society of Gynaecology and Obstetrics’ maternity care guide (2014) (6). However, studies show that oxytocin is often not given in accordance with the maternity wards’ procedures – it is often given too early or too late in the process (10, 11).
Clinical practice is complex and multifaceted, and an ongoing assessment based on ethical, financial and practical considerations needs to be made of which areas to prioritise for quality improvements.
The objective of this study was to provide a basis for considering whether measures to improve compliance with the procedure for contraction stimulation at OUH’s maternity ward should be given a higher priority.
Method
Design
We used self-administered questionnaires with pre-defined response categories and a 6-point Likert scale (assessment scale).
Sample
The population consisted of midwives at OUH’s maternity ward (n = 160). The maternity ward consists of three birthing units spread over two different locations. One location also has a midwife-run unit, but patients in need of medication to stimulate contractions are not treated at this unit. It is not therefore included in the study.
Sample selection procedure and data collection process
The ward manager, the midwife responsible for professional development or the midwife responsible for staff training distributed the invitation to participate in the study, including information about the survey and questionnaire, during the period June–July 2018. A two-week response deadline was set. After completing the questionnaire, respondents placed it in a dedicated post-box in the maternity ward.
The questionnaire
We developed the questionnaire based on the ward’s procedure for contraction stimulation (12) and input from skilled professionals. The questions were divided into five sections: Section 1: general characteristics, Section 2: the cervical dilation stage, Section 3: the expulsion stage, Section 4: fetal monitoring following oxytocin stimulation, and Section 5: collaboration and reporting. The questionnaire consisted of 20 questions in total.
The ward’s contraction stimulation procedure
Cervical dilation stage
If there is a lack of progress after two hours of labour, or the action line is crossed, interventions should be initiated (artificial rupture of membranes). The partogram of the electronic maternity patient record system includes an alert line and an action line. The alert line marks 1 cm per hour, and the action line is placed four hours to the right of this.
After the rupture of membranes, midwives must wait a minimum of one hour before initiating oxytocin stimulation. If the labour starts to progress, stimulation is not initiated. In order to prevent slow progress, the ward’s procedure recommends labour stimulation interventions such as one-to-one care from a midwife, changing position, urination and energy intake (12).
Expulsion stage
Active pushing can take up to two hours after full dilation of the cervix if the head is not engaged. During this time, interventions such as the artificial rupture of membranes, changing position, urination and nutritional intake should be initiated. Breast stimulation can also be attempted in cases of uterine inertia. After one to two hours with full dilation without the head engaging and where there is no urge to push, oxytocin stimulation should be considered (12).
Stimulation with oxytocin should be documented when medication is first administered and when the dose is changed. The midwife should also document indications for stimulation, frequency of contractions and classification of continuous fetal monitoring (cardiotocography (CTG) or ST analysis (STAN)).
An oxytocin checklist should be followed, and the team leader (midwife with team leader function) should be consulted before starting the oxytocin drip. The fetus should be monitored continuously using CTG/STAN when oxytocin is used to stimulate contractions (12).
Ethical considerations
The study was conducted in accordance with current guidelines on research ethics. It was approved by the Norwegian Centre for Research Data (NSD) and the Data Protection Officer at OUH, as well as the management at the hospital’s maternity ward. Everyone who participated in the study was given written information about the objective of the study and contact details for any questions. We emphasised that participation was voluntary, and by responding to the questionnaires consent was implied. All the data were treated confidentially.
Data analysis
Descriptive analyses show the frequency and percentage. The distribution of scores is shown in a histogram.
Results
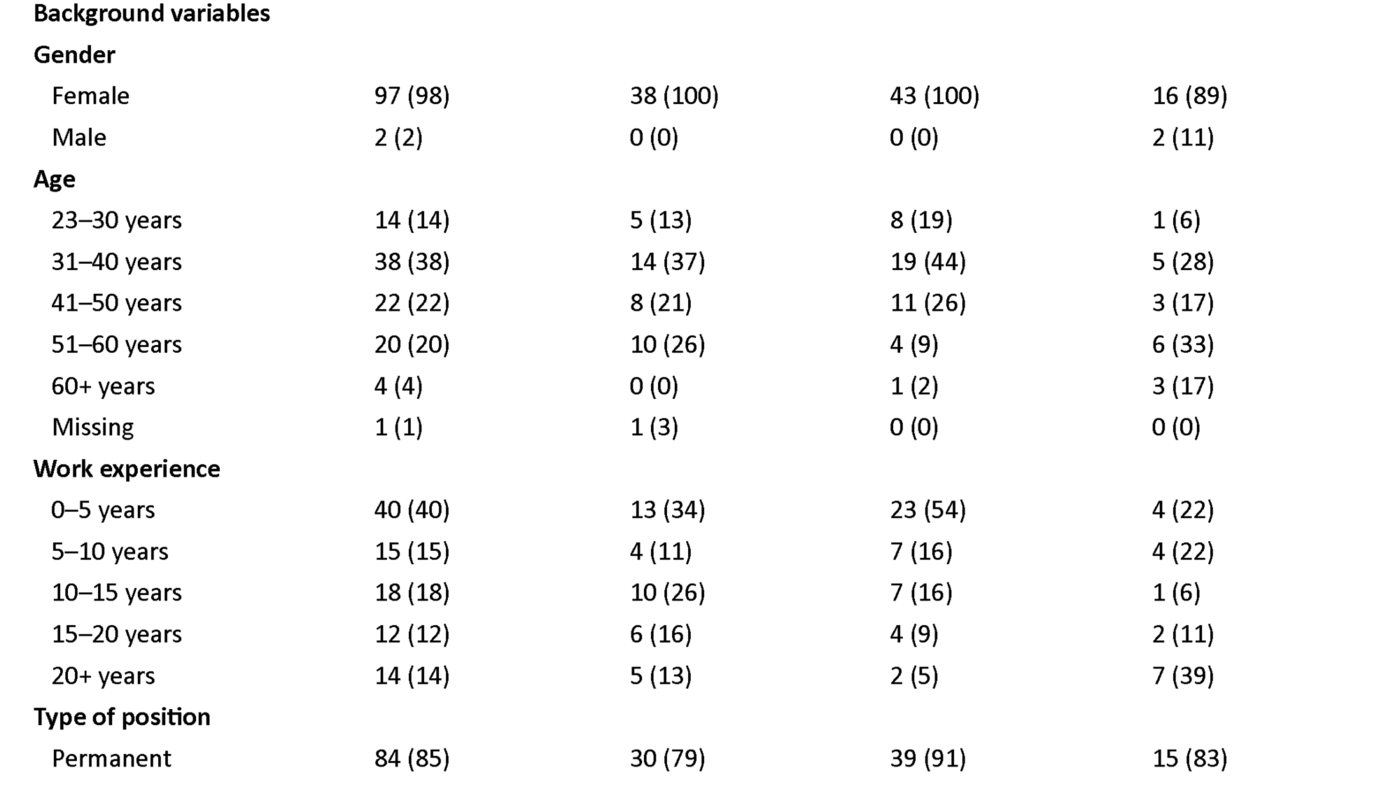
A total of 99 midwives responded to the questionnaire (99/160; 62 per cent). The study population is presented in Table 1.
Rupture of membranes and oxytocin stimulation in slow progress
Eighty-two out of 97 midwives (85 per cent; two missing answers) reported that when labour is not progressing, they perform an artificial rupture of membranes either often, very often or almost always/always (4, 5 or 6 on the Likert scale).
In response to a question on how long they wait to initiate oxytocin stimulation after the rupture of membranes when labour is not progressing, 14 of 98 midwives (14 per cent; one missing answer) responded that they start oxytocin stimulation one hour after the rupture of membranes when labour is still not progressing. Seventy-nine midwives (81 per cent) reported waiting for one to three hours, while 5 (5 per cent) reported waiting for less than one hour.
Non-medication interventions and breast stimulation
All of the midwives in the study answered questions about the extent to which they use contraction stimulation interventions such as changing position, urination and energy intake as a way of preventing slow progress. All responded that they use non-medication methods to prevent slow progress either often, very often or almost always/always (4, 5 or 6 on the Likert scale).
Sixty per cent of the midwives stated that they use breast stimulation during the expulsion stage either rarely, very occasionally or sometimes (1, 2 or 3 on the Likert scale).
Active pushing in the expulsion stage
All midwives answered the question on how long they await active pushing if the cervix is dilated 10 cm but the head is not engaged. Eighty-seven midwives (88 per cent) responded that they wait two hours for active pushing. Four midwives (4 per cent) stated that they wait for one hour, and seven (7 per cent) wait for three hours. One midwife (1 per cent) reported waiting for four hours.
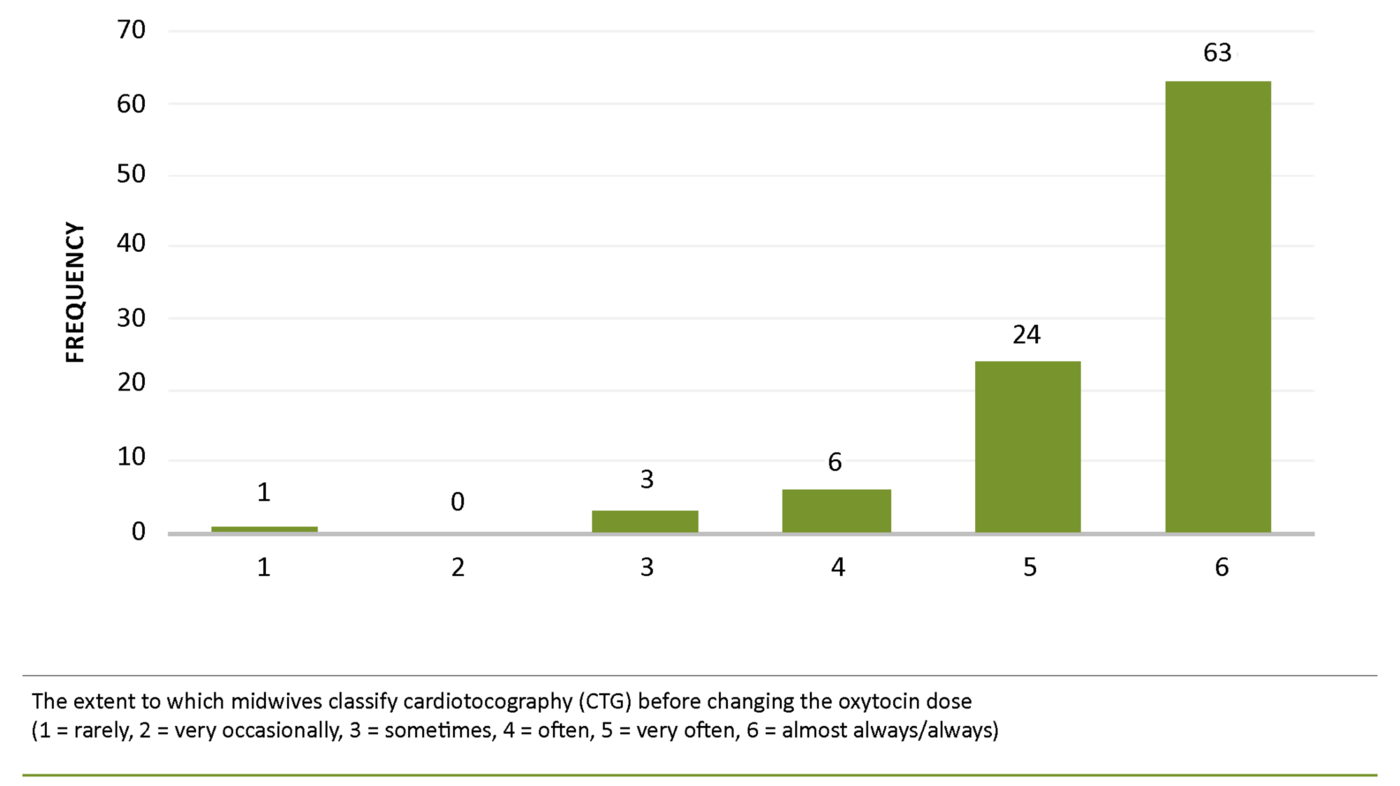
Fetal monitoring and classification of CTG
Ninety-seven midwives (2 missing answers) reported that they use continuous fetal monitoring when the woman is stimulated with oxytocin, either very often or almost always/always (5 or 6 on the Likert scale). The majority (69 per cent) stated that they classified CTG before changing the oxytocin dose almost always/always (6 on the Likert scale) (Figure 1).
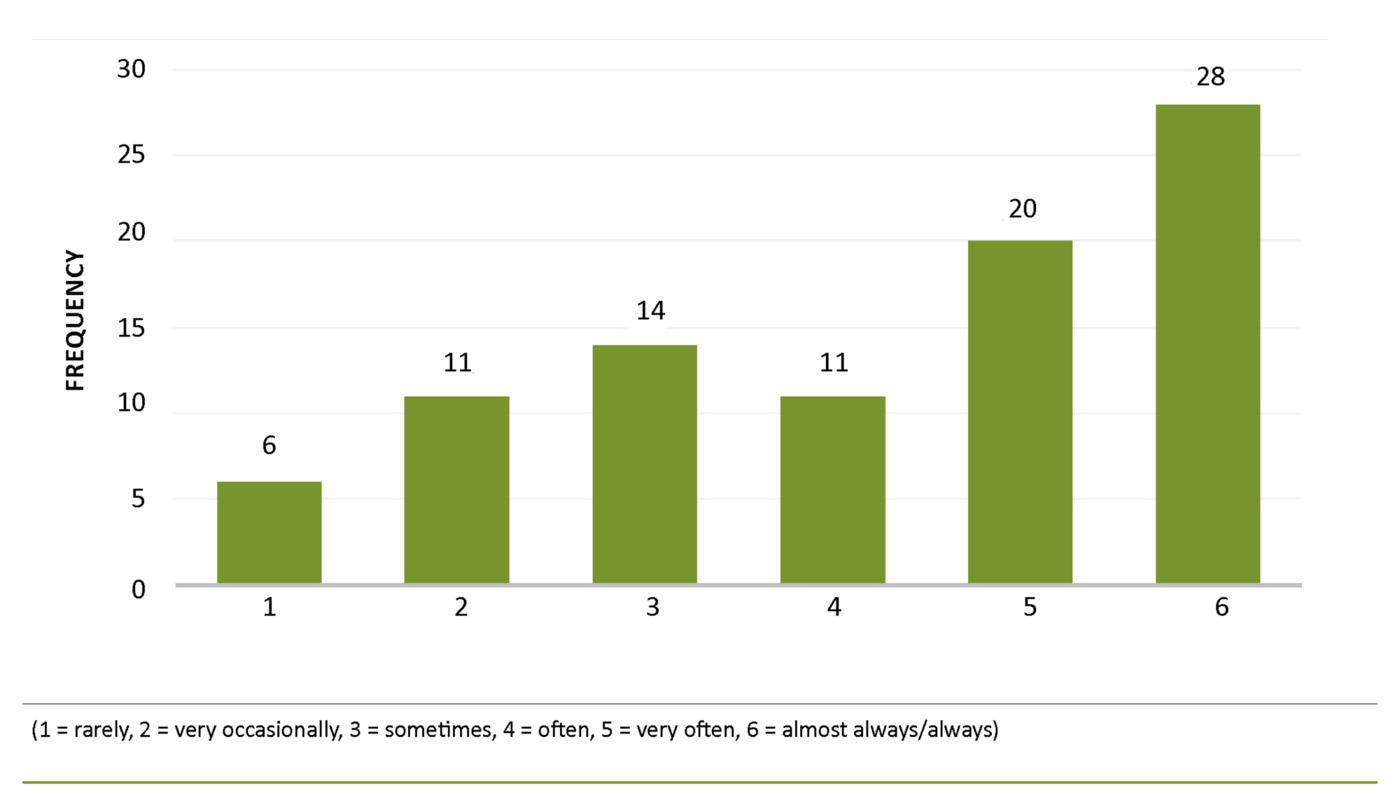
Oxytocin checklist and interaction with colleagues
About one-third of the midwives (34 per cent; 9 missing answers) reported that they use a checklist for oxytocin stimulation either rarely, very occasionally or sometimes (1, 2 or 3 on the Likert scale) (Figure 2). The question on how often the midwife conferred with a midwife with a team leader function or a doctor prior to starting the oxytocin drip was answered by 92 midwives (7 missing answers).
Most of the midwives (90 per cent) stated that they confer with a midwife with a team leader function or a doctor prior to starting oxytocin stimulation either often, very often or almost always/always (4, 5 or 6 on the Likert scale).
Discussion
The study shows that midwives report following with the ward’s procedure for contraction stimulation in several areas, but that there are challenges associated with when to initiate oxytocin stimulation, the classification of CTG when changing the oxytocin dose, and the use of a checklist for oxytocin stimulation.
Use of non-medication interventions and rupture of membranes
The study showed that all midwives largely use non-medication interventions such as changing position, urination and energy intake to prevent slow progress in the dilation stage, while only 40 per cent use breast stimulation to the same extent as a contraction stimulation intervention during the expulsion stage. The results may indicate that the midwives choose to use medication to stimulate contractions in the expulsion stage rather than breast stimulation.
The preference to use medication to stimulate contractions in labour rather than non-medicinal interventions may be due to differences in culture, attitudes and habits among staff (13). Care should be taken when transferring monitoring and interventions to births that are not generally considered to be complicated (14).
The majority of midwives (85 per cent) reported that they perform an artificial rupture of membranes when labour has not progressed for two hours, or if the action line is crossed. A smaller proportion (15 per cent) stated that they do not perform this intervention in line with the ward’s procedure for contraction stimulation. This may indicate that the midwives do not agree with the recommendation or are not familiar with it.
Non-compliance with procedures increases the risk of adverse events. In the period from 1 July 2012 to the end of 2013, the Norwegian Directorate of Health’s reporting system for adverse events received 692 reports of incidents that had occurred in connection with pregnancy, childbirth and postnatal care in the specialist health service. The majority of events (226) were related to non-compliance with guidelines, procedures or manuals (15).
Oxytocin stimulation and fetal monitoring
Fetal monitoring during oxytocin stimulation was reported to be in accordance with the procedure for contraction stimulation. The Norwegian Directorate of Health’s manual on safe childbirth services stipulates quality assurance requirements for intrapartum care in Norway (14).
According to the requirements, all birthing units that accept at-risk women must have advanced fetal monitoring equipment that includes fetal monitoring in the form of CTG with scalp blood testing or ST analysis. It is important that the midwife ensures that both the parous woman and the fetus are properly monitored during labour (16).
Most midwives reported that they classify CTG when changing the oxytocin dose. Nevertheless, a few do not. Classifying CTG is important documentation and part of the patient record. The patient record is intended to serve as a tool for healthcare personnel and should also ensure transparency for patients and the regulatory authority in terms of the health care provided.
The patient record is also important when other therapists need to know what treatment the patient has received. The patient record should therefore provide a comprehensive picture of the health care provided and show any assessments that form the basis for treatment and interventions.
Oxytocin checklist and interaction
One in three midwives reported that they rarely or sometimes used oxytocin stimulation checklists. Checklists are used to structure the healthcare personnel’s approach to the patient through a set of standardised questions and to ensure compliance with the procedure. The ward’s oxytocin stimulation checklist is currently available as an appendix to the procedure in the e-handbook on the health trust’s intranet page (12).
The report to the Storting Én innbygger – én journal (One inhabitant – one patient record) (17) states that decision-making aids for healthcare personnel, such as checklists, should be included in the patient record system to help the healthcare personnel make the right decisions.
Research in the USA shows that the use of such systems improves patient safety (18). Developing user support aids in the maternity patient record system could help improve compliance with the procedure and produce statistics for use in considering further interventions.
The majority of the midwives reported that they confer with a midwife with a team leader function or a doctor prior to initiating oxytocin stimulation. Staff planning should be organised according to the personnel’s qualifications, and staff should collaborate with other healthcare personnel when necessary (16). National guidelines recommend that care for women with normal labour should be provided by a midwife (19).
The midwife can independently monitor and guide the birth if it progresses without complications. If this is not the case, the midwife should interact with the doctor, either by keeping him or her informed or asking them to go to the delivery room to assess the patient. It is good practice for the midwife to work with the obstetrician where stimulation interventions have been used, or where there are other risk factors.
Weaknesses of the study
We used self-administered questionnaires to collect the data. Respondents may have perceived questions about behaviour as threatening in that they felt checks were being made to establish whether they follow the provedure or not. Their answers may therefore show a bias towards aligning with the procedure, which may lead to over-reporting (20).
In addition, we recognise that it may have been useful to add more response options and give the respondents the opportunity to elaborate on their answers. It is also possible that some of the terms used in the questionnaires are not well enough defined to function as a precise response alternative. These are methodology weaknesses that have probably affected the results.
The non-response rate in the survey was 38 per cent. There were major differences in the midwives’ interest in the study and the theme. Some showed considerable interest, while others showed little or no interest.
It is reasonable to assume that this variation in interest is also reflected in the sample, and thus also in the results. We nevertheless believe that the study provides a basis for evaluating measures to improve compliance with the procedure for contraction stimulation at OUH’s maternity ward.
Conclusion
The survey has shown that the midwives report that they follow the ward’s procedure for contraction stimulation in several areas, but that there are challenges associated with when to initiate oxytocin stimulation following the rupture of membranes, the classification of CTG when changing the oxytocin dose, and the use of a checklist for oxytocin stimulation.
The results are self-reported, and the reported compliance with the maternity ward’s procedure for contraction stimulation may be overestimated. Nevertheless, we believe that the results provide an important basis for prioritising areas for further work in relation to compliance with the procedure.
Mari Elisenberg and Marthe Regine Staubo are both first authors.
References
1. Cheng YW, Hopkins LM, Caughey AB. How long is too long: Does a prolonged second stage of labor in nulliparous women affect maternal and neonatal outcomes? Am J Obstet Gynecol. 2004;191(3):933–8.
2. Rossen J, Okland I, Nilsen OB, Eggebo TM. Is there an increase of postpartum hemorrhage, and is severe hemorrhage associated with more frequent use of obstetric interventions? Acta Obstet Gynecol Scand. 2010;89(10):1248–55.
3. Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A. Epidural versus non-epidural or no analgesia for pain management in labour. The Cochrane Database of Systematic Reviews. 2018;5:Cd000331.
4. Folkehelseinstituttet. Statistikkbanken for Medisinsk fødselsregister (MFR). Oslo; 2019. Available at: http://statistikkbank.fhi.no/mfr/(downloaded 12.11.2018).
5. Bugg GJ, Siddiqui F, Thornton JG. Oxytocin versus no treatment or delayed treatment for slow progress in the first stage of spontaneous labour. The Cochrane Database of Systematic Reviews. 2013(6):Cd007123.
6. Eggebø TM, Rossen J, Ellingsen L, Heide HC, Muneer S, Westad S. Stimulering av rier. In: Norsk gynekologisk forening, ed. Veileder i fødselshjelp. Oslo; 2014. Available at: https://legeforeningen.no/Fagmed/Norsk-gynekologisk-forening/Veiledere/Veileder-i-fodselshjelp-2014/Stimulering-av-rier/(downloaded 30.09.2019).
7. Vilchez G, Nazeer S, Kumar K, Warren M, Dai J, Sokol RJ. Contemporary epidemiology and novel predictors of uterine rupture: a nationwide population-based study. Arch Gynecol Obstet. 2017;296(5):869–75.
8. Berglund S, Pettersson H, Cnattingius S, Grunewald C. How often is a low Apgar score the result of substandard care during labour? BJOG. 2010;117(8):968–78.
9. Helsedirektoratet. Kvalitetsindikatorer. Ristimulering under fødsel. Oslo; 2017. Available at: https://helsenorge.no/Kvalitetsindikatorer/graviditet-og-fodsel/ristimulering-under-fodsel(downloaded 11.11.2018).
10. Bernitz S, Oian P, Rolland R, Sandvik L, Blix E. Oxytocin and dystocia as risk factors for adverse birth outcomes: a cohort of low-risk nulliparous women. Midwifery. 2014;30(3):364–70.
11. Gaudernack LC, Froslie KF, Michelsen TM, Voldner N, Lukasse M. De-medicalization of birth by reducing the use of oksytocinoxytocin for augmentation among first-time mothers – a prospective intervention study. BMC Pregnancy Childbirth. 2018;18(1):76.
12. Oslo universitetssykehus. Stimulering av rier. Oslo; 2015. Available at: https://ehandboken.ous-hf.no/document/59148/fields/23(downloaded 11.11.2018).
13. Hollowell J, Li Y, Malouf R, Buchanan J. Women's birth place preferences in the United Kingdom: a systematic review and narrative synthesis of the quantitative literature. BMC Pregnancy Childbirth. 2016;16(1):213.
14. Helsedirektoratet. Et trygt fødetilbud – kvalitetskrav til fødselsomsorgen. Oslo; 2010. IS-1877. Available at: https://www.helsedirektoratet.no/produkter?letter=DEF&tema=nasjonal_veileder (downloaded 11.11.2018).
15. Saastad E, Kirschner R, Flesland, Ø. Uønskede hendelser under svangerskap, fødsel og barseltid Oslo: Folkehelseinstituttet, Nasjonalt kunnskapssenter for helsetjenesten; 2014. Læringsnotat fra Meldeordningen. Available at: https://www.helsedirektoratet.no/laeringsnotat/uonskede-hendelser-under-svangerskap-fodsel-og-barseltid/U%C3%B8nskede%20hendelser%20under%20svangerskap,%20f%C3%B8dsel%20og%20barseltid.pdf/_/attachment/inline/e03e838b-592c-486c-bf62-fc6db8dd61d3:00b812223562e34e786c6522cae7649a68c41b34/U%C3%B8nskede%20hendelser%20under%20svangerskap,%20f%C3%B8dsel%20og%20barseltid.pdf(downloaded 30.09.2019).
16. Lov 2. juli 1990 nr. 64 om helsepersonell m.v. (helsepersonelloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-64(downloaded 11.11.2018).
17. Meld. St. 9 (2012–2013). Én innbygger – én journal. Oslo: Helse- og omsorgsdepartementet; 2013.
18. Wolfstadt JI, Gurwitz JH, Field TS, Lee M, Kalkar S, Wu W, et al. The effect of computerized physician order entry with clinical decision support on the rates of adverse drug events: a systematic review. J Gen Intern Med. 2008;23(4):451–8.
19. Helsedirektoratet. Utviklingsstrategi for jordmortjenesten. Tjenestekvalitet og kapasitet. Oslo; 2010. IS-1815. Available at: https://www.helsedirektoratet.no/om-oss/om-nettstedet/innholdet-er-arkivert(downloaded 11.11.2018).
20. Ringdal K. Enhet og mangfold: samfunnsvitenskapelig forskning og kvantitativ metode. 4. ed. Bergen: Fagbokforlaget; 2018.









Comments