Ultrasound-guided peripheral venous catheterisation compared to the traditional method – a randomised controlled trial
Summary
Background: Peripheral venous catheterisation (PVC) is the most common invasive clinical procedure performed by nurses in the hospital setting. It is estimated that up to 80% of hospital patients require intravenous access. PVC can be associated with pain for the patient, particularly if multiple attempts are needed to establish intravenous access. Ultrasound is a newer method that has become increasingly used by specialised personnel, such as nurse anaesthetists, to establish intravenous access in patients with difficult vein access. More research is needed to determine whether the use of ultrasound can reduce the number of skin punctures during intravenous cannulation and whether the method is more time efficient.
Objective: The objective of the study was to compare two different methods of PVC, focusing on the number of skin punctures and time usage. The two methods used are traditional PVC and ultrasound-guided PVC (USGPVC).
Method: The design was a randomised controlled, non-blinded trial with the number of skin punctures as the primary outcome measurement and time usage as the secondary outcome measurement. The data were collected from a registration form completed by nurse anaesthetists in the relevant anaesthesiology department specifying the number of skin punctures, time usage, adult difficult intravenous access score (from the A-DIVA scale), type of catheter, location of the catheter, patients’ sex and age, which ward the patients had been admitted to, and the nurse anaesthetists’ length of service in years. The trial was conducted at Levanger Hospital.
Results: The trial included 94 patients who were to receive a PVC. Each PVC task was randomised to either USGPVC or the traditional method, with 47 PVC procedures in each group. The mean number of skin punctures was 1.30 in the USGPVC group and 1.19 in the traditional method group. There was no statistically significant difference in the number of skin punctures between the two groups (p = 0.235). In 35 of the 37 excluded PVC procedures, the reason for exclusion was that the nurse anaesthetists considered it unethical to include them in the trial, and they chose to use USGPVC. All patients that were excluded for ethical reasons had a high A-DIVA score (A-DIVA 4 and 5). The median time usage in the USGPVC group was 14.82 minutes compared to 10.15 minutes in the traditional method group. There was a statistically significant difference in time usage between the two groups, with the traditional method being faster (p = 0.001).
Conclusion: This study found no statistically significant difference in the number of skin punctures between the use of USGPVC and the traditional method for PVC in a patient group with easy to moderate vein access. However, a difference in time usage was observed between the two groups, with USGPVC taking longer. In patients with difficult vein access, the nurse anaesthetists preferred to use USGPVC.
Cite the article
Dadfar A, Rønsåsbjørg D, Torvik K, Grønning K. Ultrasound-guided peripheral venous catheterisation compared to the traditional method – a randomised controlled trial. Sykepleien Forskning. 2024;19(96834):e-96834. DOI: 10.4220/Sykepleienf.2024.96834en
Introduction
It is estimated that up to 80% of hospital patients require intravenous cannulation (1). Peripheral intravenous catheterisation (PVC) is used for a variety of interventions: medications, fluid therapies, blood transfusions and nutrition (1, 2). PVC is therefore the most common invasive clinical procedure performed by nurses in the hospital setting (3).
Previous studies have shown that possible complications, difficulties in establishing venous access and the rate of failed PVC attempts vary (4), due to factors related to the patient or catheter, as well as the skills of the person inserting the catheter (1). Patients often experience increased pain when repeated attempts are needed to establish intravenous access. The size of the catheter does not affect pain levels (5).
Research shows that although PVC is a common nursing procedure in clinical practice, the procedure is complex and can be challenging for nurses to perform (6). Nurse anaesthetists have specialised expertise in establishing intravenous access (7, 8), particularly in patients who have neither visible nor palpable veins, often referred to as ‘DIVA’ (difficult intravenous access) patients (9).
To assess the difficulty of a patient’s venous access, a validated scoring tool called the A-DIVA scale has been developed (10). The difficulty level for venous access is ranked from 0–5 based on the following variables: a history of difficult intravenous access, expected difficult intravenous access, inability to detect a dilated vein by palpating and/or visualising the extremity, and a diameter of less than 3 millimetres in the selected vein. The A-DIVA score indicates whether there is low, moderate or high risk for difficult intravenous access (10).
Two or more failed skin punctures are defined as difficult PVC. One-third of adult patients are estimated to have difficult venous access (6, 9). Failure to establish intravenous access can lead to delays in necessary treatment (11).
To establish intravenous access, there are two well-established methods: traditional PVC and ultrasound-guided PVC (USGPVC). The traditional method is based on direct visualisation and palpation of a peripheral vein. Using ultrasound makes it possible to locate a suitable vein using an ultrasound device. USGPVC has been shown to be a good alternative to the traditional method in patients with difficult venous access (12).
Several studies have also shown that USGPVC can reduce the number of skin punctures and the time required for PVC in patients with difficult venous access (13–16). If a patient is defined as having easy venous access (low A-DIVA score), the traditional method is considered the most effective method (16).
Several international studies comparing USGPVC with the traditional method for PVC in adult patients have shown that USGPVC reduces the number of skin punctures in patients with difficult venous access (17, 18). None of the aforementioned studies were conducted in Norway. In hospitals in this country, nurse anaesthetists are often called on to establish intravenous access. This occurs when nurses in surgical and medical wards assess the patient as having difficult venous access.
Objective of the study
The objective of this study was therefore to investigate whether USGPVC results in fewer skin punctures than the traditional method when nurse anaesthetists are called on to establish intravenous access in patients in surgical and medical wards. We also wanted to examine whether there is a difference in time usage between traditional PVC and USGPVC. We therefore formulated a hypothesis related to our primary outcome measurement, which was the number of skin punctures, and a hypothesis for our secondary outcome measurement, which was time usage:
- There is a difference in the number of skin punctures between traditional PVC and USGPVC.
- There is a difference in time usage between traditional PVC and USGPVC.
Method
Design and setting
This study has a pragmatic, randomised controlled two-arm study design and was conducted in accordance with the CONSORT Statement for Randomised Trials of Nonpharmacologic Treatments (19).
The study was carried out between June and September 2022 at a local hospital in Central Norway, which serves approximately 74 555 inhabitants over the age of 18. The practice at the hospital in the study is that ward nurses call on nurse anaesthetists from the anaesthesiology department for assistance in establishing intravenous access in patients with difficult venous access.
Over the course of one year, the nurse anaesthetists at the hospital were involved in 1658 PVC procedures in other departments. The hospital has 153 beds, distributed between medical and surgical wards.
Before the study commenced, all nurse anaesthetists undertook training in USGPVC. The training programme consisted of one hour of theory and practical guidance, training in the A-DIVA scale, practising with ultrasound on a vein phantom, and a minimum of one USGPVC on a patient under supervision.
Sample
The inclusion criteria in our study were: 1) nurse anaesthetists who had completed training in USGPVC, and 2) adult patients over 18 years old who the nurses in the hospital’s surgical and medical wards assessed as having difficult venous access.
The exclusion criteria in the study were nurse anaesthetists who had not completed training in USGPVC and patients who were critically ill or in isolation for an infectious disease. We also excluded patients who it was deemed unethical to include after the nurse anaesthetists had gone through the A-DIVA scoring assessment.
The study participants who were nurse anaesthetists were recruited by the first and second authors. Nurse anaesthetists who met the inclusion criteria were given written and oral information about the purpose of the study and informed that participation was voluntary. Those who wished to participate in the study gave written consent.
The patients in the study were recruited by the nurse anaesthetists who were called on to establish venous access. It was the nurse anaesthetists who informed the patients about the study and its objective. They also indicated that participation was voluntary and that there would be no negative consequences for the patients if they chose not to participate. Patients who wanted to participate gave oral consent in accordance with the recommendations from the Regional Committee for Medical and Health Research Ethics (REK).
Intervention group
PVK procedures that were randomised to the intervention group were conducted using USGPVC.
Control group
In the control group, the traditional method for PVC was used, involving visualisation and palpation of the vein.
Randomisation
The randomisation was carried out by having the nurse anaesthetists draw a sealed, opaque envelope from the anaesthesiology department when they were called from a medical or surgical ward to carry out PVC on a patient. The envelopes contained information about which method should be used – USGPVC or the traditional method. They also contained a registration form that the nurse anaesthetists were to fill out after completing the PVC procedure.
All envelopes were filled, sealed and then mixed up by one of the researchers. The second researcher then numbered all the envelopes from 1 to 100. These two processes were conducted independently of each other. The nurse anaesthetists were instructed to take the envelope with the lowest number when they were allocated a PVC procedure. The envelope was not opened until the patient had been informed about the study and had given oral consent to participate and had undergone the A-DIVA scoring assessment.
Data collection
We collected data using the registration form developed for this study. The data included the number of skin punctures, time usage, A-DIVA scores, type of catheter, location of the catheter, patients’ sex and age, the patient’s ward, and the nurse anaesthetists’ length of service. The A-DIVA score was ranked from low (0-1), moderate (2-3) or high (4-5) risk for difficult venous access.
Primary outcome measurement
The primary outcome measurement of the study was the number of skin punctures that the nurses anaesthetists needed to establish venous access. This is a recognised outcome measurement that has been used in similar studies (14–16).
Secondary outcome measurement
The secondary outcome measurement in the study was time usage, including preparation time in the anaesthesiology department when retrieving equipment, going to and from the ward, the actual location of the catheter and tidying up afterwards.
Sample size
The sample size (20) was calculated based on the primary outcome measurement, which was the number of skin punctures, with a test power of 90% and a significance level of 5% (14–16).
From the aforementioned studies, the results of the number of successful skin punctures on the first attempt in patients assessed as having difficult venous access were combined. The calculated sample size was n = 46 in each group. To account for potential exclusions from the study, such as PVC procedures with registration forms that were incorrectly filled in or incomplete, we included 50 PVC procedures in each group.
Statistical analyses
We analysed the data using the statistical software SPSS, version 27 (21). A one-sample t-test was employed to investigate whether there was a difference in the number of skin punctures (primary outcome measurement) between the intervention group and the control group. We employed Mann-Whitney’s U test to examine whether there was a difference in time usage between the intervention group and the control groups (secondary outcome measurement) since the data were not normally distributed (20). If the p-value was less than 0.05, we considered the difference between the groups to be statistically significant.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki (22). The study has been approved by the Regional Committee for Medical and Health Research Ethics (REK), reference number 455676, and by the Data Access Committee (DAC) at the local hospital, reference number 2022/2331 – 17683/2022. Parts of the study were funded through research grants from Nord-Trøndelag Hospital Trust. All participants were informed about the objective of the study. The patients gave oral consent to participate in accordance with the decision from REK, while the nurse anaesthetists gave written consent.
Results
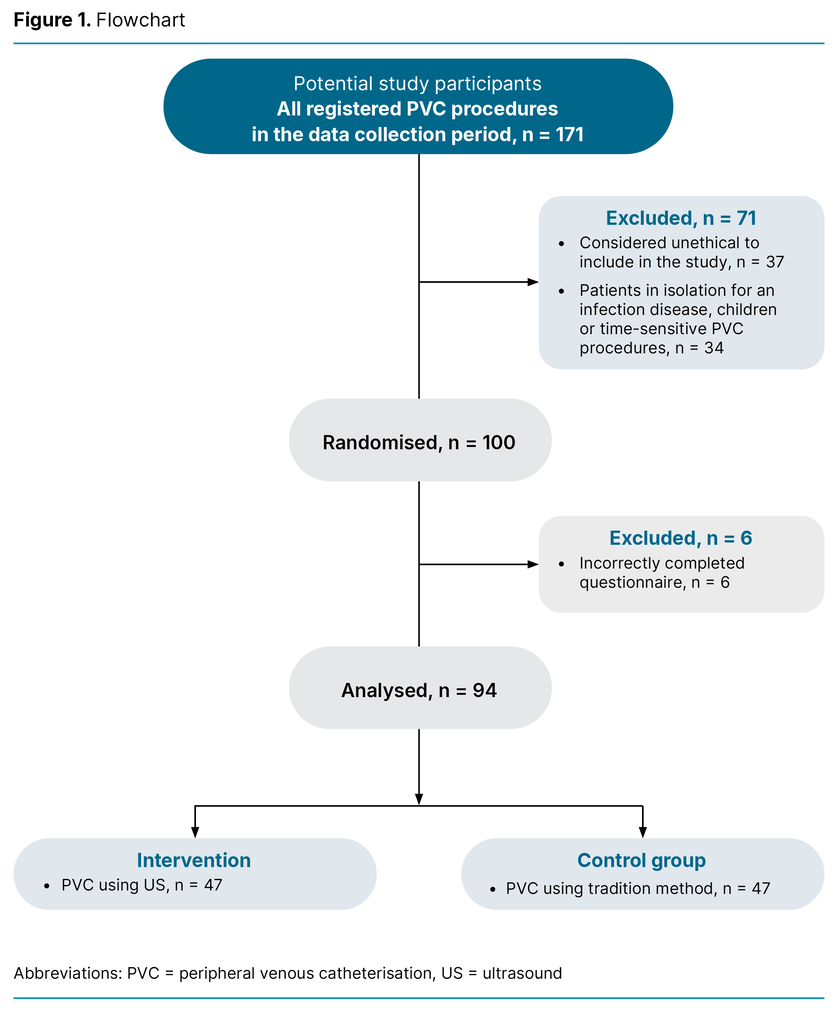
A total of 20 out of a possible 29 nurse anaesthetists participated in the study, and 171 PVC procedures were registered during the study period. Of these, 71 were excluded (Figure 1), either because the nurse anaesthetists deemed it unethical to include the patient in the study, or due to the procedure involving children or patients in isolation for an infectious disease, or time-sensitive PVC procedures.
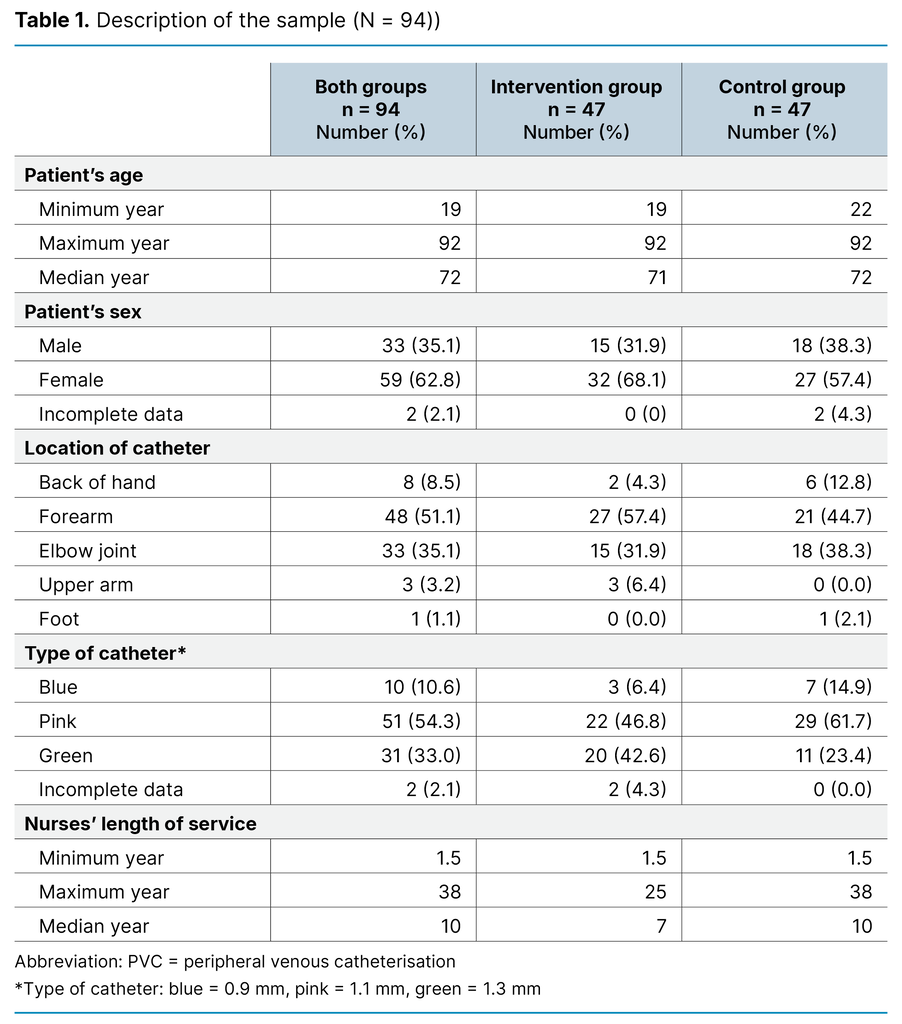
The results show that the majority of the patients included were women (62.8%). The median age of the patients was 72 years, with a range spanning from 19 to 92 years. Most of the catheters were pink (1.1 mm), and the most common location was the forearm (Table 1). The analyses also indicated that the patients included had a mean A-DIVA score of 2.16, indicating a low to moderate risk for difficult venous access (9).
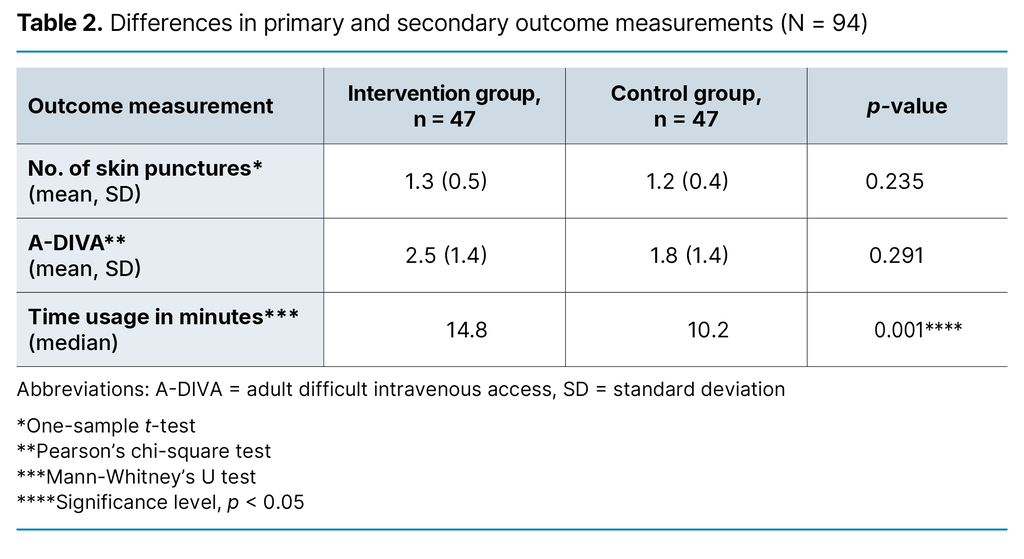
The analyses examining the differences between the intervention group and the control group are presented in Table 2. The t-test showed no statistically significant difference in the number of skin punctures between the groups, with an average of 1.3 and 1.2 skin punctures per patient in the intervention group and control group, respectively (p = 0.235).
There was also no statistically significant difference in the A-DIVA score based on the difficulty of venous access for patients in the intervention group (A-DIVA 2.5) and the control group (A-DIVA 1.8) (p = 0.291). However, Mann-Whitney’s U test indicated a statistically significant difference in time usage between the two groups, with USGPVC taking longer, at 14.82 minutes, compared to the traditional method, which took 10.15 minutes (p = 0.001).
Discussion
The objective of this study was primarily to investigate whether the use of USGPVC results in fewer skin punctures than the traditional method when nurse anaesthetists are called on to establish intravenous access for patients in surgical and medical wards. However, no statistically significant difference was found in the number of skin punctures between USGPVC and the traditional method.
Our findings align with another study (16), which shows that USGPVC is not a more suitable method for patients with defined simple venous access, i.e. an A-DIVA score between 0 and 3 (10). Furthermore, we found that USGPVC took longer to perform than the traditional method.
It also transpired that the venous access for patients in our study had a low to moderate A-DIVA score. Based on the findings in this study, the traditional method of PVC rather than USGPVC should be used for patients with simple venous access. The traditional method takes less time and is just as effective as USGPVC.
Several factors were involved in the calculation of time usage, making it difficult to compare our study with other studies. These factors included physical distances within the hospital, preparation of equipment, the nurse anaesthetists’ level of experience in using ultrasound, and the patient’s condition.
Findings from our study are consistent with results from other studies (23, 24) showing that nurse anaesthetists spend a significant amount of time performing PVC procedures in other departments. This finding is important in terms of ensuring optimal use of hospital resources. If ward nurses are given additional training and more opportunities to practise PVCs, it may result in fewer painful procedures and subsequent complications for patients with genuinely difficult venous access.
Additionally, nurse anaesthetists could make better use of their expertise (6). The results in this study may indicate that the nurses in the wards did not feel confident enough to perform PVC, even though the venous access for the patients, per definition, had a low to moderate A-DIVA score.
Strengths and weaknesses of the study
The study was conducted at a local hospital where the practice is that ward nurses can call on nurse anaesthetists for assistance in establishing intravenous access if they assess the patient as having difficult venous access. We therefore assumed that our sample of patients would have difficult venous access, as the ward nurses had assessed them as having such. However, this assumption turned out to be incorrect, as the sample’s mean A-DIVA score of 2.16 corresponds to a low to moderate risk of difficult venous access (10).
There is therefore a need for further research on how nurses assess the difficulty of venous access as well as their own skills and competence in performing PVC. Studies should also be carried to explore whether the traditional method or USGPVC is better suited when patients have a high A-DIVA score. A potential risk in the latter study is that patients could be subjected to multiple skin punctures during PVC.
The design of the study is one of its strengths (20). We used simple randomisation, which means that all PVC procedures had an equal chance of being assigned to the control group (traditional method) or the intervention group (USGPVC), resulting in comparable groups. This randomisation therefore strengthens the validity of the study, as the groups being compared are nearly identical, allowing us to determine whether the traditional method, which is the current standard, or USGPVC is the most suitable method.
However, one of the weaknesses of all randomised controlled trials is that they are conducted under controlled and standardised conditions, which do not necessarily reflect clinical practice (25). Nevertheless, this study was designed and carried out in a way that closely mirrors everyday practice in the hospital. Ward nurses can contact nurse anaesthetists when they need assistance with PVC. We therefore consider the results of this study to have high practical and clinical utility.
Another potential weakness of this study is that the nurse anaesthetists excluded a relatively large number of patients due to high A-DIVA scores and ethical considerations. This resulted in the patients in this sample having venous access that was defined as ‘simple/moderate’, i.e. an A-DIVA score between 0 and 3, and not difficult venous access according to A-DIVA. We discussed this exclusion criterion with REK before the study began and, in consultation with REK, determined that such a criterion was necessary to avoid causing unnecessary discomfort and pain to the patients.
Unfortunately, the data collected did not include detailed information on why patients were excluded, but many nurse anaesthetists commented on the registration form that they felt it was irresponsible not to be able to choose the method they believed was best when patients had a high A-DIVA score.
In 35 of the 37 excluded cases with a high A-DIVA score, the nurse anaesthetists chose to use USGPVC. This indicates that the clinical assessments of nurse anaesthetists align with research in the field, which shows that USGPVC is the best method for patients with very difficult venous access (14–17).
Another weakness of the study was the reliance of one of the inclusion criteria on the nurses’ subjective assessment of difficult venous access, without using a validated scoring tool. The results show that the nurses’ subjective assessment was an insufficient measure of ‘difficult venous access’, and meant we were unable to study USGPVC in patients with a validated score for difficult venous access.
For future studies on the use of USGPVC and the traditional method, researchers should therefore consider defining the inclusion criterion for ‘difficult venous access’ as A-DIVA ≥ 4 (10), in order to investigate whether USGPVC is more effective than the traditional method in patients with a high A-DIVA score.
The nurse anaesthetists in our study had extensive experience and training in traditional PVC, but their level of experience in using USGPVC varied. Some of the nurse anaesthetists had only received the training necessary to take part in this study, while others had been using USGPVC for several years.
In order to protect the privacy of the study participants, we did not collect data on the nurse anaesthetists’ level of experience. The department is relatively small and transparent. However, on average, the nurse anaesthetists in this study had less practical experience and training in using USGPVC, i.e. fewer hours, compared to nurse anaesthetists in other studies (14–16), where both the experience level required and the success rate were higher.
Implications for practice
The results in this study show that the traditional method for PVC is just as effective as USGPVC in patients with easy to moderately difficult venous access (A-DIVA score 0–3). The traditional method was also quicker to perform and is therefore recommended for patients with a low A-DIVA score.
Although the sample in our study did not exhibit ‘difficult venous access’, meaning that we were unable to definitively state that USGPVC is best suited for a high A-DIVA score, other studies have shown this (14–16). Discussion is therefore needed on whether training in USGPVC should be mandatory for nurse anaesthetist students, as using ultrasound for PVC can entail fewer skin punctures and less pain for patients with difficult venous access.
Consideration should also be given to whether undergraduate nursing students should be given more training in PVC. Furthermore, efforts should be made to ensure that ward nurses also have the opportunity to practise PVC (6).
Conclusion
This randomised controlled trial found no statistically significant difference in the number of skin punctures between USGPVC and the traditional method. However, the findings indicate that when patients have difficult venous access, nurse anaesthetists prefer to use ultrasound for PVC.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge









Comments