Experiences with a telemedicine service for patients with COPD: a case study
Summary
Background: Many patients live with chronic diseases such as chronic obstructive pulmonary disease (COPD). The goal is for patients to better manage the disease at home and reduce the use of healthcare services. Digital home monitoring, formerly known as remote medical monitoring, is a telemedicine service that can help improve the monitoring of the health status of patients with COPD outside hospital settings. Little is known about patients’ experiences with this service.
Objective: The objective of the study was to describe the experiences with the service from the perspective of the patients, caregivers and healthcare personnel.
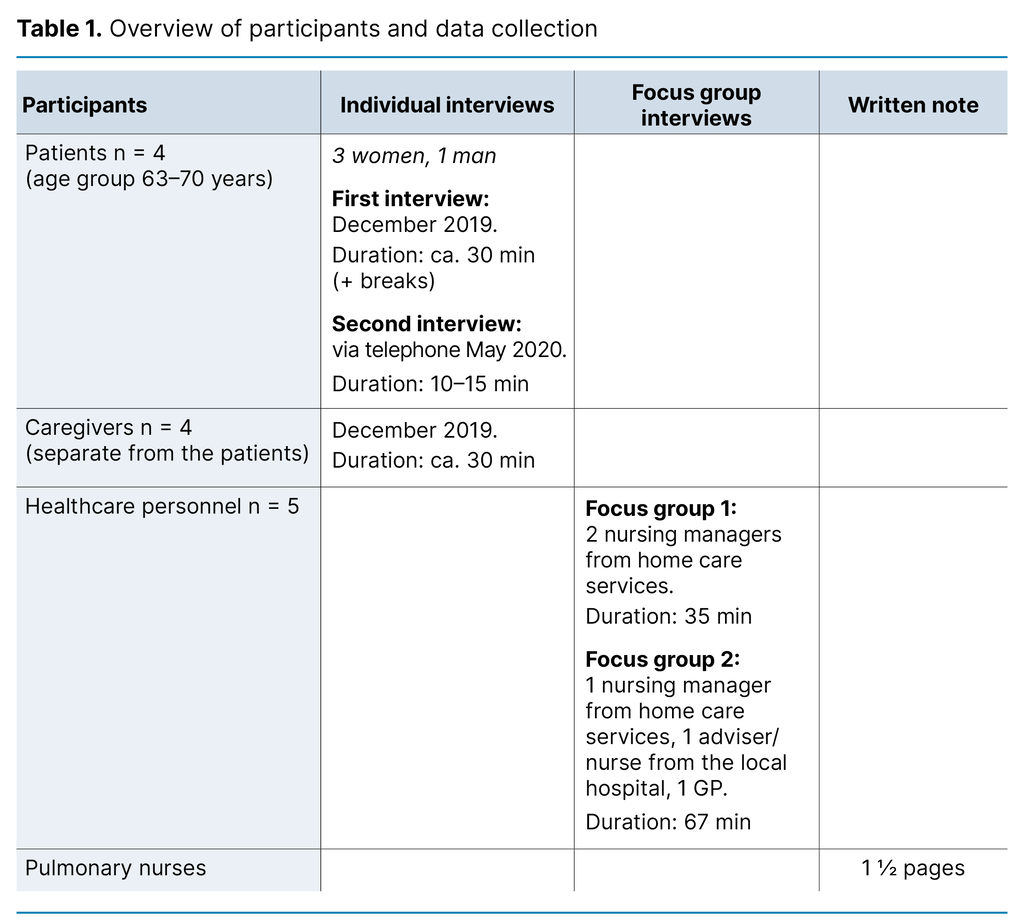
Method: We conducted a case study in a Norwegian municipality. A total of 13 participants were interviewed. Four patients and their caregivers were interviewed separately; the four patients were interviewed twice, and five of the healthcare personnel were interviewed in a focus group. We also used an evaluation note from a group of pulmonary nurses in the analysis. We performed a thematic content analysis of the data.
Results: The experiences of the participants in the study were predominantly positive. The service had provided reassurance for patients and their caregivers, and all the participants believed that the patients’ improved self-management of the disease gave them more independence, allowing them to live better with the disease. However, participants expressed that the service could have been better coordinated between the different healthcare providers.
Conclusion: In order for digital home monitoring to contribute to reassurance, self-management and independence for patients with COPD, it is important that the service is tailored to the individual patient, such that they perceive it as safe and useful. There is a need for role clarification between the specialist health service, primary health care and telemedicine services. How the service is to be continued and funded should be clarified so that patients and caregivers can optimise their use of the service.
Cite the article
Leirvik Å, Bjørsland B, Nakrem S. Experiences with a telemedicine service for patients with COPD: a case study. Sykepleien Forskning. 2023;18(94164):e-94164. DOI: 10.4220/Sykepleienf.2023.94164en
Introduction
Patients with chronic obstructive pulmonary disease (COPD) face a severe symptom burden (1) and frequent hospitalisation (2). Preventive measures aim to enable the patient to manage their disease, thereby reducing morbidity and the uptake of health services (3). With digital monitoring, patients can be more closely monitored, and this can be done outside the hospital setting (4).
Digital home monitoring, formerly known as remote medical monitoring, is a telemedicine service in which healthcare personnel assess the patient’s health status remotely and provide guidance, medical advice and care in the patient’s own home (5, 6). This method of monitoring helps the patient feel more in control, which in turn can contribute to better self-management of the disease (7). The shift towards greater follow-up by the primary healthcare service and through digital services is rooted in, inter alia, Report no. 26 to the Storting (2014–2015) (8) and Report no. 29 to the Storting (2012–2013) (9).
Telemedicine interventions appear to have particularly positive effects for the most severely affected COPD patients (10). However, there is no difference in resource utilisation between digital home monitoring and traditional healthcare services for people with COPD, especially for the specialist health service in isolation (11). A systematic literature review by Cochrane nevertheless showed that a multicomponent intervention could reduce the number of hospital admissions, even though telemonitoring also made little difference in this study (12).
Most patients have a positive attitude towards telemedicine (13). Telemedicine leads to strong personal relationships being established between patients with COPD and nurses through dialogue, good care and follow-up. Telemonitoring can promote active patient participation in treatment and help to empower the individual patient (3, 7). For patients’ caregivers, this can reduce their worry and make them feel reassured that the telemedicine service helps the patient manage the disease and treatment (7, 14).
It has been demonstrated that telemedicine can sometimes be considered an inadequate form of care when the health service uses the technology in a way that does not address the patient’s individual needs (15). Informatics and technology are part of nurses’ core expertise and are standard in modern care. In digital monitoring, nurses need to be aware of how technology affects the relationship between the nurse and the patient. Nursing interventions involving technology require nurses to be reflective (16).
The article is based on a municipal pilot project that was initiated by the local primary health service and the local hospital. The collaboration with the local hospital aimed to reach the target group that could benefit most from the service. More knowledge is needed about the experiences of patients with COPD and their caregivers with digital home monitoring, compared to the experiences of healthcare personnel with the service.
Objective of the study
The objective of the study was therefore to explore the experiences with the telemedicine pilot project in the municipality – digital home monitoring – from the perspective of patients, their caregivers and the healthcare personnel.
Method
The study is designed as a case study in one municipality. The case study method allows researchers to examine a ‘case’ in detail, i.e. delving deeply into a complex phenomenon within its natural context (17). The objective of our study was to describe and gain a comprehensive understanding of the telemedicine service from several perspectives. We therefore considered a case study with qualitative interviews to be appropriate.
The COVID-19 pandemic arrived in Norway during the pilot project. As a result, participants’ experiences with the telemedicine service during the pandemic are included in the case study.
Description of the case
The telemedicine service in the municipality was initiated in May–June 2019 as a pilot project for 20 patients over a period of six months. The patients were recruited by the local hospital. The inclusion criteria were, among other things, COPD stage 3 or 4, the ability to use a mobile phone and some experience with digital services. The service utilised a 24-hour telemedicine monitoring centre (TMC) with specially trained nurses located elsewhere in Norway.
Through the technical equipment, nurses could monitor the patient’s health status, conduct digital consultations with the patient, receive real-time measurements and intervene at an early stage to prevent exacerbation. At the relevant TMC, symptom assessment was performed using a custom-designed algorithm based on daily recordings of oxygen saturation and pulse via spirometry and pulse oximeter, as well as the patient’s self-reported health status. If the real-time measurements deviated from the normal range, the nurse at the TMC contacted the patient by phone.
The initial ten patients included in the pilot project, along with staff from home care services in the municipality, participated in a training day with the TMC. The patients were given the necessary equipment. A ‘telemedicine group’ was established in home care services to provide technical training to the remaining patients throughout the autumn of 2019.
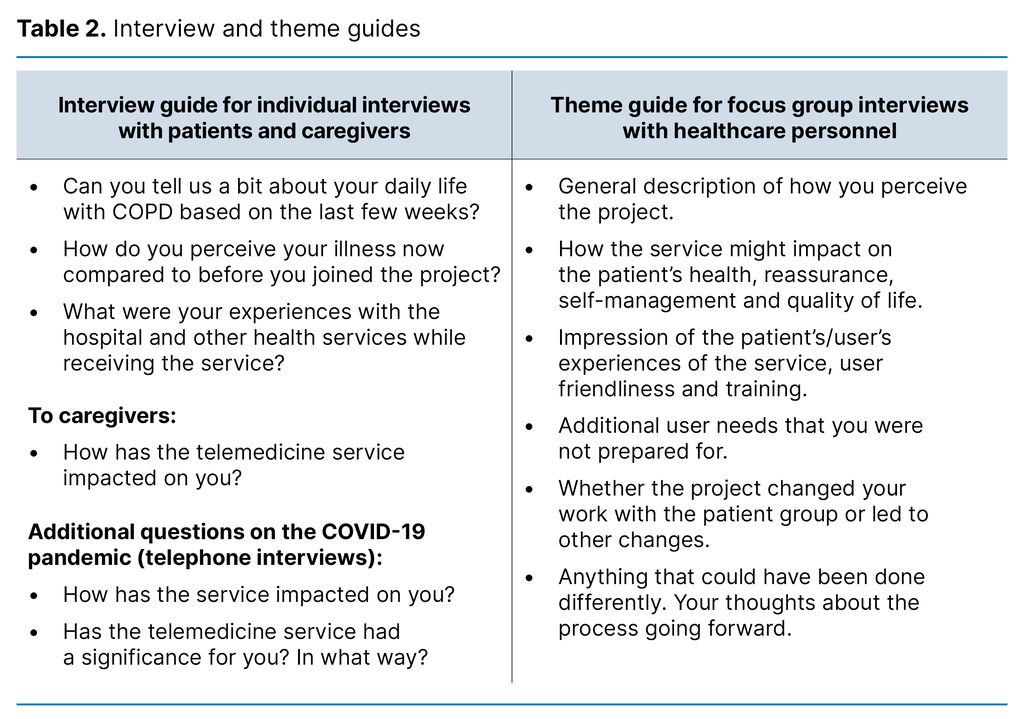
Data collection and sample
To study the case and shed light on the theme from several perspectives, we used four different data sources (Table 1). We devised an interview guide for patient and caregiver interviews and a theme guide for the focus group interviews (18, 19) (Table 2). The interview and theme guides were based on research literature on the topic of the study, as well as the researchers’ clinical and research experience.
The first ten patients who were recruited to the pilot project, and thus had the most experience, received an information letter along with a consent form and were informed that they would be contacted by phone. Patients not residing with a caregiver were excluded since caregivers were to be included in the sample. For patients and caregivers, we conducted individual interviews in their own homes. Patients and their caregivers were interviewed on the same day but in separate rooms. We made audio recordings of the interviews, which were subsequently transcribed by the second author.
Healthcare personnel affiliated with and with experience from the pilot project were invited to participate in a focus group interview. Nurses from the TMC were not included as they also monitored patients in other municipalities that already had an established telemedicine service. Nor were they directly associated with the pilot project.
Due to the pandemic restrictions on the number of people who could gather, the focus groups were divided into two. The first author recorded the interviews and transcribed them. She also served as the moderator in the focus group interviews. The pulmonary nurses from the local hospital were unable to participate. Instead, they provided a written evaluation note based on a general question about their own experiences with the pilot project. The note described the overall experience of the pulmonary nurses, without naming specific patients or conveying other sensitive information.
Analysis
We employed thematic content analysis, initially of the data from the various sources and subsequently for the entire dataset (18, 19). The note from the pulmonary nurses was reviewed and used in the analysis process to compare the experiences from the interviews and identify contrasts and contradictions.
The dataset was read through several times to form an overall impression. We then reflected on and discussed these impressions with a view to identifying themes that represented the interviewees’ experiences with the telemedicine service. Meaning units and codes were identified.
The first and second authors conducted the initial analysis, comparing and systemising sub-themes. All authors then met to discuss codes, sub-themes and themes until a consensus was reached on the main findings. Finally, we selected quotes to illustrate the findings (Table 3).

Research ethics
Research involving vulnerable patients requires the researcher to be cautious in their approach to the patients and their caregivers. The interviews with the patients and caregivers were conducted by a researcher who is a nurse and has experience with the patient group. The researcher was aware of this vulnerability and was able to use her experience to make allowances for the participants throughout the interview, giving them sufficient time and ensuring their well-being.
The project was conducted in accordance with applicable regulations and with the approval of the Norwegian Centre for Research Data (NSD) (project number 53693, reference code 995988) and the Regional Committee for Medical and Health Research Ethics (REK) (reference number 2016/2310, amendment notification). We obtained written informed consent from the patients, caregivers and healthcare personnel at the start of the interviews and verbal consent in the telephone interviews.
Results
The main finding from the case study was that the participants’ experiences were predominantly positive. The service had provided reassurance for the patients and their caregivers. All participants believed that the service improved patients’ self-management, allowing them to live better and more independently with the disease.
Some challenges were reported. For instance, participants expressed that the service could have been better coordinated between the different healthcare providers. The healthcare personnel mentioned that there was uncertainty about how the telemedicine service should be organised going forward. Three themes emerged, and these are presented below.
Greater sense of reassurance for the patients and their caregivers
All the patients reported feeling short of breath, tired and experiencing a high heart rate, but that the monitoring gave them reassurance and peace of mind. They believed it was better to be at home than in the hospital, and this had a positive effect on their well-being and activity. One patient described how active the disease had been in the past, with frequent hospitalisation. For one patient, the disease was stable enough that they could still work every day but felt reassured by the telemedicine service and the daily measurements.
The patients mentioned that a telemedicine nurse promptly identified any changes and contacted them by telephone to offer guidance. The nurse would call daily when the patient had breathing difficulties. The pulmonary nurses explained that patients they met at check-ups at the outpatient clinic expressed a strong sense of reassurance knowing that they would be contacted if the measurements they submitted indicated any issues. They no longer had to rely solely on their own health assessments.
Through the evaluations every three months from the TMC, the healthcare personnel in the municipality received positive feedback that the service was working well for the patients. One participant in the focus group interviews shared the same view: ‘My overall impression is that they feel much more reassured. One of them hasn’t been hospitalised since last summer when he was admitted with pneumonia.’
All of the patients’ caregivers also felt more reassured. They said that being the patient’s caregiver was challenging, even though the patient had had COPD for a long time, as the disease was steadily getting worse. One caregiver said they felt anxious when the patient became short of breath but believed they were well supported: ‘They call almost every day. She [the telemedicine nurse] was the one who sent her to the doctor when she was admitted to the hospital.’ This provided relief for the caregivers, as they no longer felt sole responsibility for supporting the patient.
In the telephone interviews, the patients were asked about their experiences during the COVID-19 pandemic. All had been worried about their own health and stayed home a lot and practised social distancing. However, they felt reassured by the telemedicine monitoring during this period. Two patients had trouble breathing. In consultation with the telemedicine service, they received cortisone medication without being hospitalised.
Self-management, independence and quality of life
Several participants felt that their self-management of the disease improved when using the telemedicine service. One patient expressed that her medication was better and that she could make adjustments herself. Another had started exercising twice a week with others. This patient mastered tasks more effectively by breaking them down, and now had the confidence to shower on their own. Another became more adept at recognising symptoms and felt able to rest occasionally.
Another example, according to the nurses in the municipality, involved a patient whose condition worsened and who received treatment relatively quickly from the TMC nurses. The patient indicated that she normally had to wait a bit longer. The pulmonary nurses confirmed this: ‘Some patients had been slow to contact a doctor when their condition worsened. This problem has now been identified, enabling them to start treatment more promptly.’
The healthcare personnel told how the patients, in general, now had more freedom to do things, such as visit their cabins, which could improve their quality of life despite having a serious chronic illness. Another of the healthcare personnel said the following: ‘This is fantastic for the users’ quality of life. Also for their caregivers, not having to be so afraid for the loved one they live with, who is basically very ill.’ There had been very few challenges for participants in relation to handling the technical equipment. The healthcare personnel from home care services had therefore had little contact with the patients.
One nurse said that one of the 20 other patients reported to the project organisers that ‘having to report in every day made him feel very tied down’. He felt stable and chose to withdraw from the study. It was important that the patients and their caregivers perceived the benefit of sharing health data in the form of daily measurements with the health service as greater than the burden. The caregivers also believed that the telemedicine monitoring improved the patients’ quality of life. One was pleased that the patient wanted to join an exercise group run by the local authority when encouraged to do so by the pilot project staff.
The healthcare personnel reported that several patients had started exercising and were more socially and physically active: ‘Because they receive telemedicine monitoring and are in constant contact with the nurses, they have the confidence to engage in earnest. There has been almost no drop-out in the exercise group.’ Nor had the pandemic situation led to drop-outs, even though infection control measures sometimes required them to keep exercising at home, with remote guidance from healthcare personnel.
Challenges of the service
Even though all participants were predominantly positive about the telemedicine service, some challenges emerged in relation to various individual needs. Several patients wanted additional information about their illness. For example, one of them frequently experienced anxiety with palpitations but had never learned breathing and relaxation techniques. This patient had searched for information about COPD on the internet, but this made them feel anxious.
Another patient still smoked daily but wanted help to stop. Caregivers also expressed a need for more information. One was concerned that both they and the patient might lose access to the service if the patient did not stop smoking.
It also emerged that there might be a need for role clarification among the various actors, both internally and externally, such as determining who should be the contact person in home care services for the TMC and defining the roles of the general practitioner (GP) and pulmonary nurses. One caregiver believed that neither the GP nor the nurses in the municipality followed up on the patient to any significant extent.
The pulmonary nurses also said they missed being able to communicate with the others in the health service when patients were identified through the TMC as having worsening conditions, and, for example, were put on a course of antibiotics: ‘The patient had an appointment for a check-up during or right after the treatment, so the check-up was too soon after the course of antibiotics. The appointment would have been postponed if we had known about this.’
Only a few of the patients initially used home care services. However, the healthcare personnel told of patients who no longer needed healthcare services, or that the need was delayed: ‘Even though we don’t have any statistics, we see fewer hospital admissions. There are certainly some long-term financial gains to be made here.’
Documenting effects and gains, however, is challenging. The local authority currently bears the costs, but when calculating the effects of the service, it is not the municipality that benefits initially, with one local authority manager commenting as follows: ‘It is often the hospital that notices fewer admissions [...]’.
As patients with COPD get worse, they tend to require considerable support from home care services. However, working out whether the telemedicine service actually reduces the need for services is challenging. The healthcare personnel in the focus groups hoped that home care services could be put in place before the need arises for more extensive interventions.
Discussion
The findings indicate that all participant groups mainly had positive experiences, and that there were few challenges related to the technical implementation of the pilot project. Patients and caregivers perceived the service as an extra reassurance and support, which helped with management of the disease. However, there were some challenges with the service in relation to meeting individual needs for information about living with COPD. This also applies to the division of roles and responsibilities in the event of the service being continued.
Greater sense of reassurance for the patients and their caregivers
The patients described a varying symptom burden and said that the follow-up with the telemedicine nurses gave both them and their caregivers more reassurance. This finding is in line with other studies showing that patients receive emotional support for the burden of living with COPD. The studies also show that the follow-up can be regarded as a lifeline, where patients quickly receive guidance and advice when needed (6, 14), even though telemedicine may not always be sufficient to detect early signs of periodic exacerbation of the condition (20).
Caregivers reported that telemedical monitoring gave them peace of mind in the event of changes to measurements. They found that the monitoring gave them a sense of relief and considered it crucial, as caregivers of this patient group often face substantial stress (21).
All patients experienced heightened concerns about their own health during the COVID-19 pandemic. They nevertheless felt reassured knowing they would be contacted if there were any issues with the measurements, as also found in another study (22). A report from the Norwegian Board of Health Supervision stated that 92 per cent of local authorities reported a reduction in the home care services provision for patients during the pandemic (23).
However, several local authorities found that some changes implemented as a result of the pandemic, such as digital services, were positive, and they wanted to maintain them. The fact that there were few technical challenges in the pilot project may indicate that it was relatively easy to use, which could be crucial for whether older patients will use home monitoring or not.
Self-management, independence and quality of life
Having someone in the background gave the patients confidence to undertake activities they had previously been hesitant about. This helped their self-management of the disease, as also found in other studies (24). The service resulted in patients in the pilot project exercising more and continuing to exercise from home during the pandemic. Better insight and understanding of the patient’s own health condition has previously been shown to be important for their sense of reassurance (25).
The interaction between patients, caregivers and healthcare personnel can be perceived as motivating, guiding and supportive, and can be associated with hope (26) – something of great importance in chronic conditions such as COPD. Digital home monitoring can thus be a valuable supplement to the healthcare services for these patients, as it improves understanding and self-management of the disease (8).
Studies show the importance of individual guidance from healthcare personnel for the prompt treatment of exacerbations. Systematic follow-up through self-management plans is also essential for promoting the patient’s self-management and reducing the symptom burden and hospitalisation (27).
The healthcare personnel confirmed that they perceived the telemedicine service as positive for the patients and their caregivers. Technology can serve as a supplement, contributing to better interaction between the healthcare services and caregivers. The use of technology can free up resources in the care service which can then be diverted to direct patient-centred work (15).
Challenges of the service
The healthcare personnel expressed that the service could have been better coordinated between the different healthcare providers. Home care services personnel are open to adopting different technologies to improve standards and optimise resource use (28); however, introducing telemedicine as a permanent service in primary care poses various challenges (29).
In its final report, the Norwegian Directorate of Health recommends that local authorities adopt digital home monitoring but seek collaboration within the healthcare community at the outset (5). Experiences from Sweden also suggest that there is a need for a clearer organisation and division of responsibilities between the different levels of the health service (30).
Strengths and weaknesses of the study
Drawing general conclusions based on a study of only one case can be challenging, even though case studies can improve the understanding of complex problems within a specific context (17). One of the strengths of our study is the various types of data that were collected to shed light on the case from different perspectives.
Our sample of patients for in-depth interview was random, with the first four who agreed to participate being selected. A larger sample would have strengthened the study (18), but the strength of information was partially compensated for by the inclusion of perspectives of caregivers and healthcare personnel.
Restrictions on the number of people who could gather during the pandemic resulted in two focus group interviews being held with two and three participants, respectively. To achieve an effective exchange of experiences, the ideal would have been to combine the focus groups into one interview with five participants (19). Nevertheless, the strategic sample of information-rich participants enabled interaction between the participants, allowing for experiences to be illuminated from different perspectives.
Conclusion
The experiences of the patients, caregivers and healthcare personnel with the telemedicine service in this municipal pilot project were predominantly positive. The service had provided them with reassurance and improved their self-management, which was crucial, as both the patients and their caregivers experienced less anxiety and worry, even during the COVID-19 pandemic. However, individual patient needs could have been better addressed.
There is room for improvement in terms of clarifying roles and responsibilities among the specialist health service, primary health care and the telemedicine services. It is important to clarify how the service should be continued in consultation with patients, caregivers and healthcare personnel.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge








Comments