Catheter-related bloodstream infections in infants who have undergone neonatal surgery
Summary
Background: Catheter-related bloodstream infections (CRBSI) represent a feared complication in neonates with surgically placed central venous catheters. Infections can be a tough experience for the infant and family in terms of pain, discomfort, complications, delayed infant-parent attachment and development and at worst, death. Registering treatment-related infections is an important part of quality assurance efforts, and few studies have dealt with nursing documentation of symptoms and signs of CRBSI.
Objective: The objective of the study was to identify documentation practices and examine what symptoms and clinical signs registered nurses document in a group of patients with and without CRBSI who have undergone neonatal surgery. The aim was to identify and evaluate nursing documentation, thus contributing to greater knowledge about CRBSI and its prevention, and better treatment. The study focuses on the following research question: How do registered nurses document clinical observations that raise suspicion of catheter-related bloodstream infections in infants who have undergone neonatal surgery?
Method: We conducted a pilot study with a retrospective case control design using descriptive analyses. We used a self-developed assessment chart in order to gather data from written and electronic observation forms, charts and nursing documentation in the patient documentation systems DIPS and Metavision. The sample included five infants in the CRBSI group and ten in the control group.
Results: Pulse and temperature were most frequently documented in both groups. Fever was documented in the case of three of the five infants in the CRBSI group while in the control group, fever was not documented. Clinical signs of infection were most frequently documented in the CRBSI group. Observations of the insertion site of the central venous catheter when changing dressings, and the child’s behaviour were most frequently documented in the control group.
Conclusion: The documentation of fever is the symptom that most clearly distinguishes the CRBSI group from the control group. The total number of documented registrations of clinical signs of infection is higher in the CRBSI group than in the control group. This may indicate that fever is the factor that determines which clinical signs of infection are observed and documented in the ensuing patient care pathway. A number of observations were not documented in either of the groups and what was documented can appear to be random and unsystematic.
Cite the article
Helvig E, Emblem R, Røkkum H, Ravn I. Catheter-related bloodstream infections in infants who have undergone neonatal surgery. Sykepleien Forskning. 2020;15(79952):e-79952. DOI: 10.4220/Sykepleienf.2020.79952en
Neonatal infections cause high morbidity and mortality (1), and every year 3.8 per cent of all newborn infants in Norway are treated with a shorter or longer course of antibiotics (2).
What is CRBSI?
Catheter-related bloodstream infection (CRBSI) in neonates is a tough experience for the infant and family in terms of pain and discomfort, increased risk of complications, extended hospitalisation, delayed infant-parent attachment and development, and at worst death (3). CRBSI increases the burden on the health service. Efforts to reduce CRBSI form part of quality assurance work in hospitals, and the incidence of infections is a quality indicator (3).
An important part of quality assurance efforts is that registered nurses (RNs) have the necessary skills to observe, assess and document the symptoms of catheter-related bloodstream infections (4). It is difficult to recognise the symptoms of clinical deterioration in neonates, but this is crucial in preventing a patient care pathway with a serious or fatal outcome (5).
Infection in neonates is not always detected in blood samples (6). We have been unable to find studies that examine nursing documentation when CRBSI infections are suspected, but some studies refer to inadequate documentation of observations in critically ill patients (4).
The research issue and research question
There are few early warning scoring instruments that can recognise serious illness or condition in newborn infants (7). Systemising nursing documentation of symptoms and signs can simplify the diagnosis of CRBSI, distinguish CRBSI from other infections and result in improved treatment, but will not necessarily reduce the number of infections (8).
Based on the lack of available studies dealing with the quality of nursing documentation in relation to symptoms and signs of CRBSI, we asked the following research question: How do registered nurses document clinical observations that raise suspicion of catheter-related bloodstream infections in infants who have undergone neonatal surgery?
The objective of the study
The objective of the study was to identify documentation practices with the aim of contributing to greater knowledge about CRBSI, prevention and better treatment. RNs have both a professional and legal responsibility to document nursing care and treatment in the patient record. In accordance with legislation, the documentation must include systematic recording of observations, interventions, assessments and results (9, Ch. 8).
Monitoring vital signs such as temperature, pulse, blood pressure, respiration and behaviour provides vital information about the infant’s medical status. Together with observations on the insertion site of the central venous catheter (CVC), these assessments must be documented accurately and concisely (10). Minor changes may be a sign of serious infection in infants who have undergone neonatal surgery (11).
When should CRBSI be suspected?
CRBSI should be suspected when the infant has a CVC and sepsis is identified with no other established infection status. The Centers for Disease Control and Prevention (CDC) in the USA give the following criteria for monitoring and diagnosing possible CRBSI (12, 13):
- The patient has a bacterial pathogen in one or more blood cultures where the bacterium is not related to infection elsewhere on or in the organism.
- The patient exhibits at least one of the following clinical findings: fever (>38.0 °C), shivering (hypothermia) and abnormally low blood pressure (hypotension).
- In addition to the criteria given above, patients <1 year have one or more of the following signs or symptoms: fever, chills, apnoea or bradycardia.
Method
Design
The study had a retrospective, descriptive case control design, where we charted the documentation of symptoms and signs in infants with and without catheter-related bloodstream infections who have undergone neonatal surgery.
Sample
The study was conducted in one ward and two intensive care units at a hospital with a multi-regional function in neonatal surgery. The study is part of a larger quality study investigating the prevalence of CRBSI after neonatal surgery in infants diagnosed with gastroschisis, omphalocele, congenital diaphragmatic hernia, and duodenal atresia (see Fact box) in the period 1 January 2014–1 July 2016.
The time frame and population were the same in both studies. There were individual differences in the severity of the illness, and the nurse-patient ratio and the number of specialist RNs in the departments in question varied. A common feature of the newborn infants in the study was that they often required long-term parenteral nutrition and drugs via a CVC (14, 15).
In the prevalence study, five children were shown to have a catheter-related bloodstream infection according to CDC’s criteria (13). These five children constituted the CRBSI group in the study. The control group consisted of ten patients who were matched and selected according to the following identical criteria:
- Same diagnosis, gender and central venous catheter
The following criteria were intended to be as identical as possible:
- Gestational age, birth weight and the number of days with a central venous catheter
Data collection
Data collection was carried out in spring 2017. Since there were no suitable validated forms available, we used a self-developed chart to map the relevant data. The chart was based on the clinical infection signs mentioned in points 2 and 3 of the CDC’s criteria list. Point 1 is not relevant for this study.
The following data were obtained from written and electronic observation forms, charts and nursing documentation in the patient documentation systems DIPS and Metavision:
- Background data: diagnosis, gender, birth weight and gestational age
- Clinical infection signs, with registration of the highest abnormal value: temperature, pulse, blood pressure, apnoea, respiratory frequency, chills
- Clinical nursing observations of the infant’s behaviour: restless, poorly, irritable, content, other
- Total frequency of documented care of the CVC over two weeks
- Description of the insertion site of the CVC at the most recently documented change of dressing in a two-week period: bleeding/blood seepage, moisture, redness, lack of reaction (no sign of infection), removal, other
The following reference values are used in the assessment chart (Appendix 1):
Fever is defined as a documented temperature over 38.0 °C (16). Bradycardia is defined as a documented pulse below 80 BPM, and tachycardia as a documented pulse over 160 BPM (17, 18). Blood pressure has a normal systolic reading of 80 (60–100) and a diastolic reading of 45 (35–55), and hypotension is defined as being lower than the lowest normal range (17).
Respiratory frequency has a normal range of 25–66/min, tachypnoea is defined as a respiratory frequency higher than the normal resting heart rate (18). Apnoea is respiratory cessation for longer than 20 seconds (19).
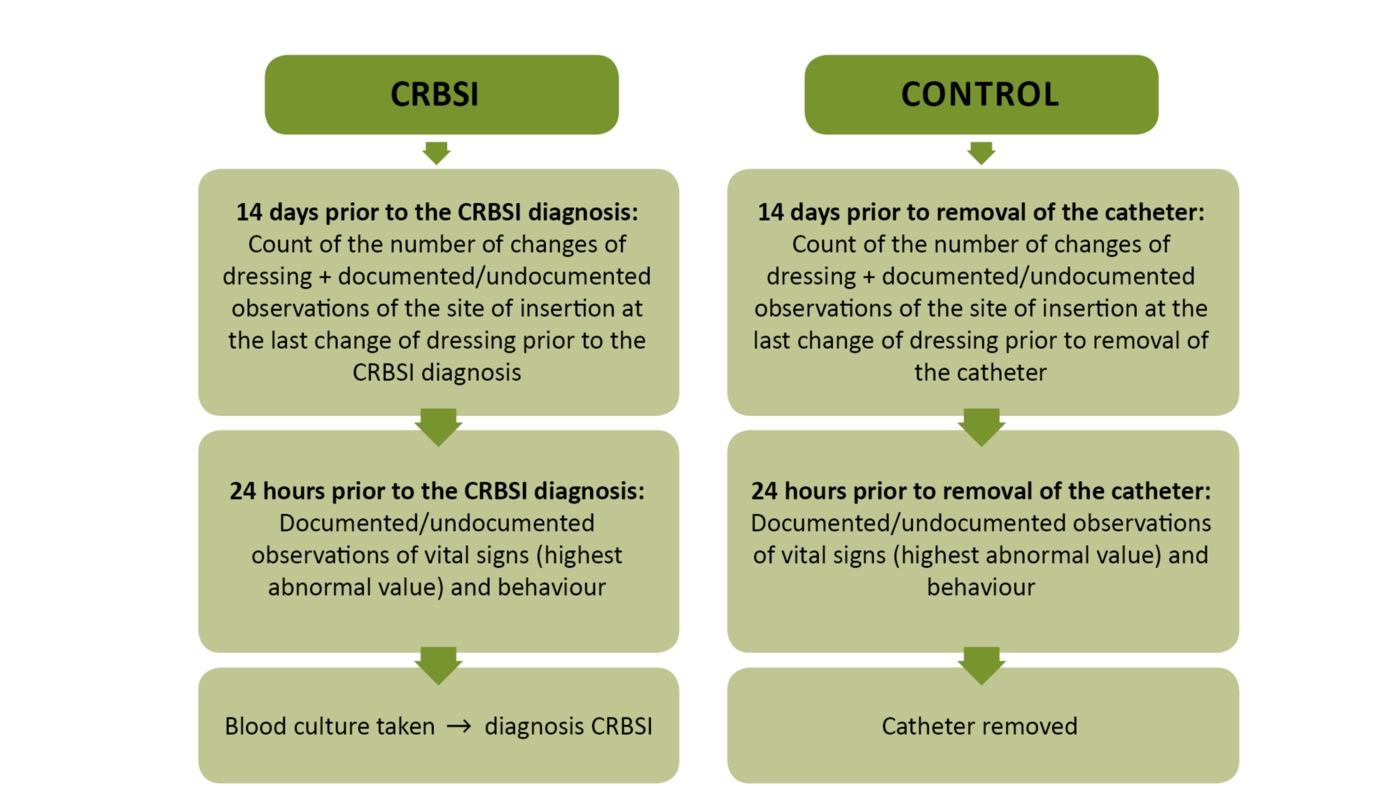
Patient data, excluding background data, were obtained for a 14-day period in the patient care pathway (Figure 1). For the CRBSI group, this represented 14 days prior to the detection of infection in the blood cultures. In the control group, this represented the 14 days previous to the removal of the catheter. The period of time was chosen to permit observation of early symptoms of infection, and to identify documentation of at least one change of dressing and observation of the insertion site of the CVC.
The most abnormal clinical infection signs were registered in the 24 hours prior to
- detected infection in the blood culture in the CRBSI group
- removal of the central venous catheter in the control group
Analysis
We performed descriptive analyses using the mean, percentage and standard deviation with IBM SPSS 23. The results were not tested for significance because the samples were small.
Approval
The study is a quality study, approved by the hospital’s data protection officer (Appendix 2 [in Norwegian]).
Results
Background data
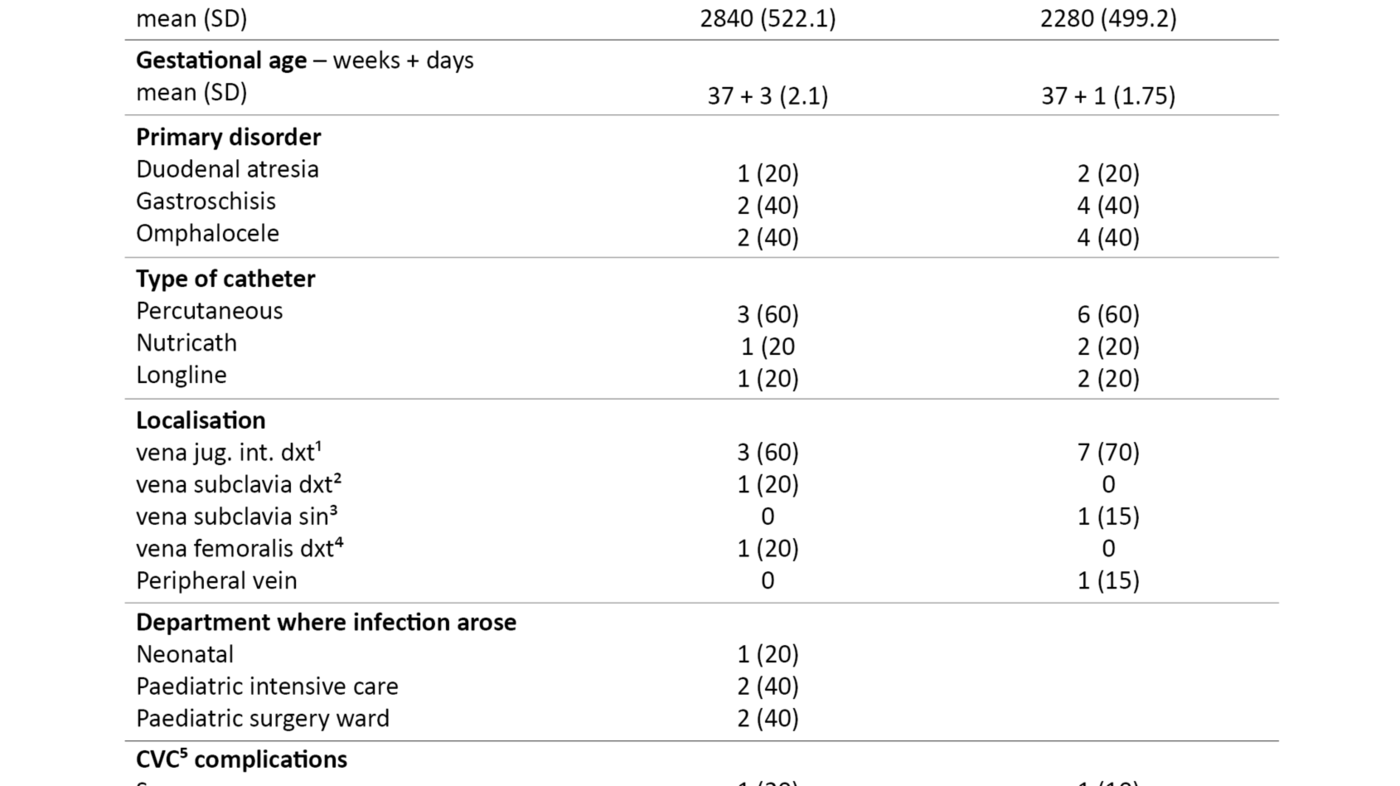
Background data are presented in Table 1. There is a preponderance of boys in both groups. The average weight was 2840 grams in the CRBSI group and 2280 grams in the control group. Infants in the CRBSI group had, on average, a CVC for 26 days while the control group had a CVC for 16 days on average.
Clinical signs of infection
Temperature
Temperature was documented for all infants in the CRBSI group (Table 2). More than half the group had a temperature measured at over 38° C. There was no documentation of temperature for two infants in the control group, while the remaining children were documented as afebrile.
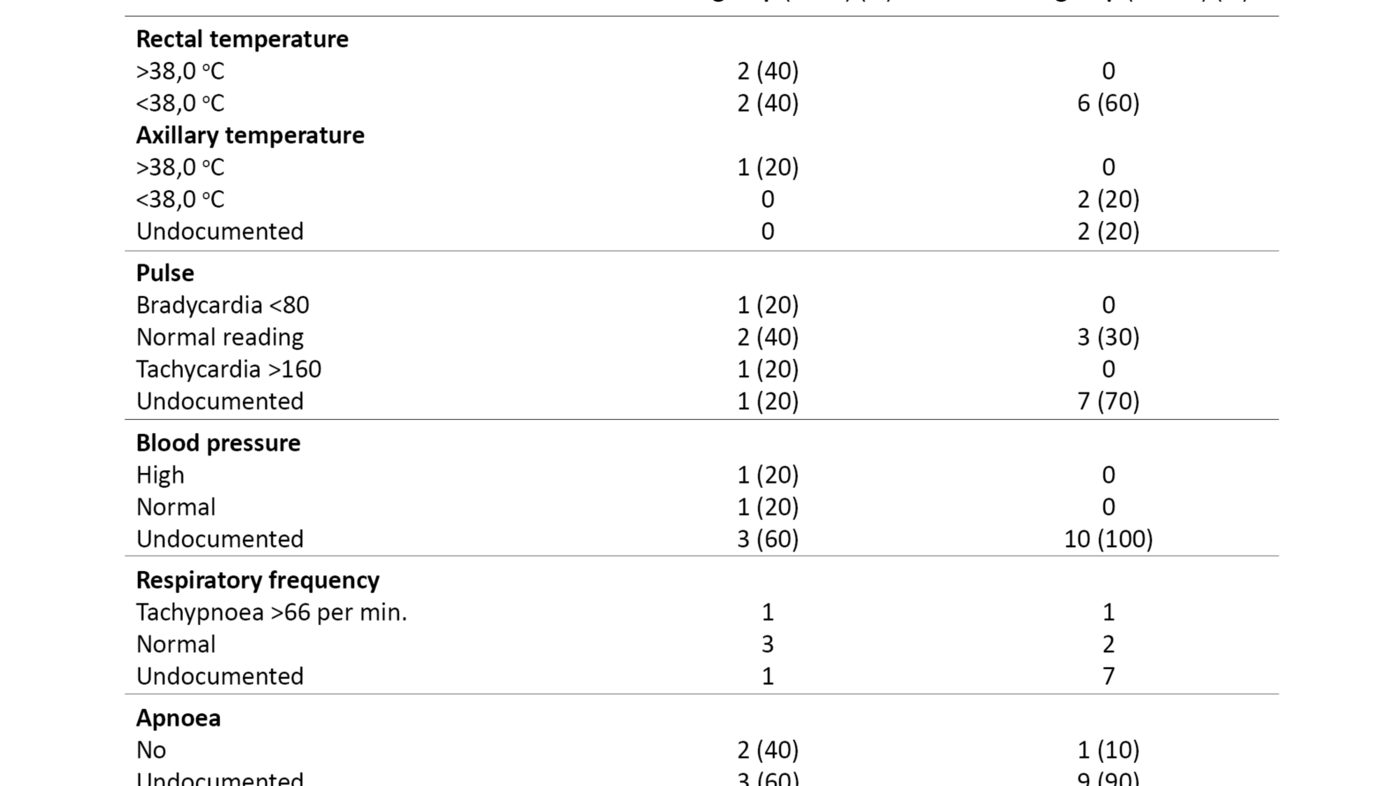
Pulse
In the CRBSI group, pulse was documented for four of the five infants. One case was documented as bradycardia and one as tachycardia. Pulse was documented in three out of ten infants in the control group, and all three were within the normal range. Pulse was not documented in seven of the infants in the control group.
Blood pressure
Blood pressure was documented for two of the five infants in the CRBSI group, one of whom was registered as having hypertension. None of the infants in the group had documented hypotension. Blood pressure was not documented for any of the infants in the control group.
Respiratory frequency
Respiratory frequency was documented for four out of five infants in the CRBSI group, one of whom had tachypnoea. Respiratory frequency was documented for three out of ten patients in the control group. One of the infants in this group had also tachypnoea. There was no documentation of apnoea, shivering or chills in either of the groups.
Changes of dressing and findings at the insertion site
At least one change of dressing was documented for all infants in the CRBSI group, but observations of the insertion site were only documented for two of the five infants. In one case, redness at the insertion site of the CVC was recorded, and the catheter was removed. In the case of the other child, the insertion site was described as showing no reaction.
In the control group, at least one change of dressing was documented for all infants. The insertion site of the CVC was described in the case of eight out of 10 infants – seven were documented as showing no reaction while one exhibited bleeding/blood seepage. The catheter had been removed in the case of one infant, but this was not described.
The frequency of dressing changes in a two-week period was 1.8 (≈ 2) on average in both groups.
Clinical observations of behaviour
In the CRBSI group, observations of behaviour were only documented for one patient who was described as content/satisfied. In the control group, behaviour was documented for all infants, five of whom were described as content/satisfied while four were described as restless and one as poorly.
Discussion
This pilot study investigated how RNs document clinical signs of infection that lead to suspicion of CRBSI in infants with and without infections who have undergone neonatal surgery. In both groups, pulse and temperature were documented most frequently. Clinical signs of infection were most frequently documented in the CRBSI group while observations of the insertion site of central venous catheters when changing dressings and the infant’s behaviour were most frequently documented in the control group.
Clinical signs of infection
Temperature
Temperature was documented for all infants in the CRBSI group. Fever is often the first and sometimes the only clinical sign arousing suspicion of infection in infants under three months of age (1, 3, 11, 16, 17). Temperature was documented for eight of the patients in the control group but none of them had a fever.
The high number of documented temperature measurements in both groups may indicate that such measurement denotes good routines at all the three departments in this study. Research also shows that neonates can have serious infections without fever. The fact that only three out of five infants in the CRBSI group had documented fever prior to the time of diagnosis may thus be a finding that concurs with the literature (1, 3, 16, 17).
Pulse
The pulse was documented for four of the infants in the CRBSI group, and bradycardia was diagnosed in one case and tachycardia in one case. The findings are supported by the literature, where both bradycardia and tachycardia are mentioned as symptoms of sepsis (1, 11, 20). In the medical literature we find that tachycardia is an early indication of sepsis in infants, since they have the ability to increase pulse rhythm in order to compensate for the fall in blood pressure (11, 16, 20).
The pulse was documented for only three infants in the control group, one of whom had tachycardia with no obvious cause. Overall, the percentage of documented pulse registrations was higher in the CRBSI group than in the control group, which may indicate that the infants in the CRBSI group were assessed as being sicker.
Blood pressure
Blood pressure was only documented for two out of five infants in the CRBSI group, and none of the infants had documented hypotension. According to the literature (1, 11, 17, 20), a fall in blood pressure is a late sign of sepsis in young children. The time of blood pressure registration varies by up to 24 hours prior to the CRBSI diagnosis.
The registration times may have been too early to detect hypotension. At the same time, when blood pressure was documented for fewer than half of the infants, it is difficult to draw any conclusions about blood pressure in the CRBSI group.
No blood pressure measurements were documented in the control group. One explanation may be that infants in the control group were not perceived as being ill. Nevertheless, this does not explain the failure to document the blood pressure of two infants in the CRBSI group. Poor routines and/or a lack of knowledge about the importance of documenting blood pressure may be a contributory factor (6).
Hypotension is a late, but vital finding in the case of sepsis (1, 20), and measuring the blood pressure is an important parameter to follow up in the case of newborn infants receiving intensive care. The study raises suspicion that the measurement and documentation of the blood pressure of newborn infants receiving intensive care is not satisfactory in the departments.
Respiratory frequency
Respiratory frequency was documented for four out of five infants in the CRBSI group. None of the group had documented apnoea, but one infant had tachypnoea. Tachypnoea may be a random finding but in combination with an elevated temperature, it may be an early symptom of infection (1, 11, 20).
Respiratory frequency was documented for three out of ten patients in the control group. The documented respiratory measurements in only seven out of 15 patients may indicate that current routines for documenting respiration are unsystematic and deficient, and that symptoms of sepsis are unspecific (1).
No infants in either of the groups had documented chills or were perceived to be chilly or cold. Hypothermia is unspecific and has poor predictive value in neonates (21), and chills are highly unusual in infants (22).
Change of dressings
The fact that at least one change of dressing was documented for the entire sample can indicate that changing dressings and documenting this is routinely carried out in all three departments. The frequency of the change of dressing is identical in both groups and corresponds to approximately one dressing change per week.
The researchers in a systematic review study (23) examined studies on the frequency of dressing changes. They were unable to conclude that there was either an increased or reduced risk of CRBSI if dressings covering the insertion site were changed every second to fifth day, or every fifth to fifteenth day. Nor did they find clear differences in terms of skin injury and irritation (23).
An international guideline recommends changing dressings no less frequently than every seventh day if the dressing is dry and there are no skin reactions (24). Oslo University Hospital’s evidence-based guideline for adults makes the same recommendation (15).
Observations made when dressings are changed
In the CRBSI group, there were few documented observations of the insertion site. Redness was described at one insertion site and the catheter was removed at the same time, probably because the redness was regarded as a sign of infection. Inflammation, redness and pus from and around the insertion site may be a sign of infection but does not necessarily mean that there is an infection (12).
In one study (16), Smitherman et al. claimed that visible signs related to the insertion site are seldom linked to catheter-related bloodstream infection, and this may be one of the reasons that these symptoms are not included in the CDC’s criteria. Nevertheless, it is difficult to draw conclusions about why there are few documented observations of the insertion site in the CRBSI group.
In the control group, the observation ‘no reaction’ was frequently documented when dressings were changed. We can assume that changes of dressing, care of the insertion site and documentation of observations are routine procedures in all wards. On the other hand, these were not consistently documented in both groups.
The explanation for observations of the insertion site being more frequently documented in the control group than in the CRBSI group, may be that the RNs had less time available to document the CRBSI group, with sicker patients, or that they had inadequate knowledge and/or too low staffing levels (5, 25). Experience shows that dressing changes are not prioritised when a patient’s general condition deteriorates.
Clinical observations linked to the infant’s behaviour
Only one infant in the CRBSI group had a documented description of behaviour corresponding to the criteria in the assessment chart. The description ‘content/satisfied’ was somewhat surprising. This finding indicates that symptoms in infants may be unspecific (1) and do not correspond with the criteria used in the assessment chart. But conclusions cannot be drawn on the basis of one single finding.
One child was described in the free-text field as ‘sensitive to touch’, an expression that can be interpreted as meaning irritable as well as being a sign of pain (17, 20). The context is important in understanding the expression. One explanation may be that the infant wakes easily when touched, but this study gives no clear answer.
Since signs and symptoms of sepsis in neonates can be subtle and unspecific, it is important to identify the risk factors for sepsis and always suspect sepsis when a child deviates from his/her normal activity and behaviour patterns, for instance when being fed. Irritability, restlessness and apathy are mentioned several times in the literature as clinical signs of sepsis and/or a reduced general condition (1, 20, 24).
Half of the infants in the control group were described as restless or poorly, and one explanation may be that such behaviour is an expression and result of stomach cramps, wind problems, hunger and regurgitation. These observations are normal post-operative symptoms in relation to the diagnoses of the children in this study and can be explained by a period of somewhat reduced peristalsis in the intestines following abdominal surgery (14).
On the other hand, vomiting or regurgitation, reduced appetite and a taut or distended abdomen are also symptoms indicating sepsis (21). For that reason, they must form an important part of the systematic nursing documentation.
Strengths and weaknesses
A weakness of the study is that we did not use a validated assessment chart (26). Prior to the study, we conducted a limited study to test the design, text formulation, applicability, measurement times and quality of the variables in order to design a chart that was simple and logical to use when collecting data (26). The assessment chart was adjusted, and we collected all data for the study and reviewed the data twice at a one-month interval. The assessments gave the same results.
The sample is small, and therefore no significance tests have been carried out. The results cannot be generalised to apply to nursing documentation for infants who have undergone neonatal surgery at other hospitals. Nevertheless, we must stress that the patients with CRBSI (n = 5) represent the total number of patients with this diagnosis who were admitted to the hospital in question within the time frame of the study.
Few symptoms and signs indicating that the child was in the process of developing or had developed CRBSI were documented in the sample as a whole, which may raise suspicion of underreporting. One explanation may be that the symptoms in neonates can be diffuse, vague and unspecific (1, 11, 21).
Another explanation may be that documentation was forgotten or not carried out because the RNs had inadequate knowledge about the symptoms of sepsis and did not suspect infection (4). The nursing documentation only reflects what was documented and not necessarily what was observed and performed. The documentation depends on the individual, clinical knowledge, the surroundings and the organisation (27).
Errors and delays may arise in the period from the measurement of vital signs until they are actually documented. One reason may be that these are recorded on paper before being documented electronically at the end of the shift. Other reasons may be the lack of available computers and interruptions on the part of patients, relatives or colleagues and collaborating partners (28). Another key question is whether the RN is required to document observations that are within the normal range.
A third reason may be that the time of measurement affects the results because we have looked for symptoms that may perhaps appear later in the patient care pathway. Despite these weaknesses, the study suggests that there is potential for improvement regarding both observations of newborn infants who have undergone surgery and nursing documentation.
Conclusion
Fever is seen as the finding that most clearly distinguishes the CRBSI group from the control group, and elevated temperature is the clinical sign of infection that is documented for most infants in both groups. The total number of documented registrations of clinical signs of infection is higher in the CRBSI group than in the control group. The most important anomalies appear to be the inadequate documentation of observations of respiration and blood pressure measurements.
Findings in the study indicate that inadequate documentation can be explained by poor documentation practices. A big workload and too little knowledge about sepsis may also be one explanation but is not assessed in this study. The conclusion is that a number of observations are not documented in either group, and that what was documented can appear to be random and unsystematic.
Proposals for further research and work
A Swedish study (29) has shown an increase in the documentation of signs and symptoms when using standardised electronic nursing plans and recommended treatment plans. A standardised scoring instrument for sick neonates such as the Newborn Early Warning Trigger and Track (7, 30), and the recommended nursing plan for observations and care of CVCs can constitute good aids for observing, assessing, monitoring and documenting early symptoms and signs that arouse suspicion of CRBSI.
A new prospective study covering a longer period should be conducted in order to acquire fresh knowledge and optimise treatment and documentation practices.
References
1. Shane A, Sánchez P, Stoll B. Neonatal Sepsis. Lancet. 2017;390(10104):1770–80.
2. Moen A, Rønnestad A, Stensvold HJ, Uleberg B, Olsen F, Byhring HS. Norsk nyfødtmedisinsk helseatlas. En analyse av innleggelser og behandling av barn i nyfødtavdelinger i Norge for årene 2009–2014. Bodø: Senter for klinisk dokumentasjon og evaluering (SKDE), Norsk Nyfødtmedisinsk Kvalitetsregister; 2016. Report 5/2016. Available at: https://helseatlas.no/sites/default/files/norsk_nyfodtmedisinsk_helseatlas_rapport_0.pdf (downloaded 06.12.2019).
3. Chessyre E, Goff Z, Bowen A, Carapetis J. The prevention, diagnosis and management of central venous line infections in children. Journal of Infection. 2015;71:S59–75.
4. Cardona-Morell M, Prgomet M, Lake R, Harrison R, Long J, Westbrook J, et al. Vital signs monitoring and nurse–patient interaction: A qualitative observational study of hospital practice. International Journal of Nursing Studies. 2016;56:9–16.
5. Tume LN, Sefton G, Arrowsmith P. Teaching paediatric ward teams to recognise and manage the deteriorating child. Nursing in critical care. 2014;19(4):196–203. DOI: 10.1111/nicc.12050
6. Brown, J. Meader, N. Cleminson J. McGuire, W. C-reactive protein for diagnosing late-onset in newborn infants. Cochrane Database of Systematic Reviews. 2019;1:CD012126.
7. Mortensen N, Augustsson, JH, Ulriksen J, Hinna UT, Schmölzer GM, Solevåg AL. Early warning- and track and trigger systems for newborn infants: a review. Journal of Child Health Care. 2017;21(1):112–20.
8. Littles C, Nguyen K, Rowe T, Johnston P, Brassel K. Symptom word documentation: a novel approach to identifying and managing hospital-acquired infections. American Journal of Infection Control. 2016;44(11):1424–25.
9. Lov 2. juli 1999 nr. 64 om helsepersonell m.v. (helsepersonelloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-64 (downloaded 01.15.2019).
10. Mok WQ, Wang W, Liaw SY. Vital signs monitoring to detect patient deterioration: an integrative literature review. International Journal of Nursing Practice. 2015;21(suppl. 2):91–8.
11. Roberts K, Coffin S. Immunology and infectious disorders In: Hazinski MF, ed. Nursing care of the critically ill child. St. Louis, Missouri: Elsevier Mosby; 2013. s. 851–65.
12. Calderwood MS. Intravascular non-hemodialysisi catheter-related infection: clinical manifestations and diagnosis. Uptodate. October 2019. Available at: https://www.uptodate.com/contents/diagnosis-of-intravascular-catheter-related-infections (downloaded 06.12.2019).
13. Wolf J, Curtis N, Worth L, Flynn PM. Central line-associated bloodstream infection in children: an update on treatment. The Pediatric Infectious Disease Journal. 2013;32(8):905–10.
14. Christofferson R, Lackgren G, Stenberg A. Grottes barnkirurgi och barnurologi. Lund: Studentlitteratur; 2015.
15. Dorph E, Salomonsen A, Olin W, Moe SH, Eide BT. Sentralt venekateter (SVK) – stell, bruk og håndtering, komplikasjoner med tiltak, voksne. Oslo: Oslo universitetssykehus; 2017. Available at: https://www.helsebiblioteket.no/fagprosedyrer/ferdige/sentralt-venekateter-svk-stell-og-bruk-av-tunnelert-og-ikke-tunnelert-kateter-hos-voksne (downloaded 13.05.2019).
16. Smitherman HF, Macias CG. Febrile infant (younger than 90 days of age): definition of fever. Uptodate. April 2019. Available at: https://www.uptodate.com/contents/febrile-infant-younger-than-90-days-of-age-definition-of-fever?search=febrile-infant-younger-than-90-days-%20of-age-definition-of-fever&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 (downloaded 15.01.2019).
17. Markestad T. Klinisk pediatri. 3rd ed. Bergen: Fagbokforlaget; 2016.
18. Silva JN. Bradycardia in children. Uptodate. August 2018. Available at: https://www.uptodate.com/contents/bradycardia-in-children?source=search_result&search=bradycardia%20in%20newborn&selectedTitle=1~150 (downloaded 08.01.2019).
19. Martin R. Pathogenesis, clinical manifestations, and diagnosis of apnea of prematurity. Uptodate. May 2018. Available at: https://www.uptodate.com/contents/pathogenesis-clinical-manifestations-and-diagnosis-of-apnea-of-prematurity?search=apnea&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 (downloaded 12.05.2019).
20. Edwards MS. Clinical features, evaluation, and diagnosis of sepsis in term and late preterm infants. Uptodate. April 2019. Available at: https://www.uptodate.com/contents/clinical-features-evaluation-and-diagnosis-of-sepsis-in-term-and-late-preterm-infants (downloaded 10.05.2019).
21. Holme H, Bhatt R, Koumettou K, Griffin MA, Winckworth LC. Retrospective evaluation of a new neonatal trigger score. Pediatrics. 2013;131(3):e837–42.
22. Store medisinske leksikon. Feber hos barn. Available at: https://sml.snl.no/feber (downloaded 13.05.2019).
23. Gavin NC, Webster J, Chan RJ, Rickard CM. Frequency of dressing changes for central venous access devices on catheter-related infections. Cochrane Database of Systematic Reviews. 2016;2:CD009213.
24. O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Guidelines for the prevention of intravascular catheter-related infections. Clinical Infectious Disease. 2011;52(9):e162–93.
25. Küng E, Waldhör T, Rittenschober-Böhm J, Berger A, Wisgrill L. Increased workload is associated with bloodstream infections in very low birthweight infants. Scientific Reports. 2019;9:article no. 6331.
26. Polit DF, Beck CT. Nursing research. 10th ed. Philadelphia, PA: Wolters Kluwer Health; 2017.
27. Tørnvall E, Jansson I. Preliminery evidence for the usefullness of standardized nursing terminiologies in different fields of application: a literature rewiev. International Journal of Nursing Knowledge. 2017;28(2):109–19.
28. Stokowski LA. Electronic nursing documentation: charting new territory. Medscape. September 2013. Available at: https://www.medscape.com/viewarticle/810573_8 (downloaded 20.05.2019).
29. Thoroddsen A, Ehnfors M, Ehrenberg A. Content and completeness of care plans after implementation of standardized nursing terminologies and computerized records. Computers Informatics Nursing. 2011;29(10):599–607.
30. Hjertaas TH, Solevåg A. Verktøy kan gjenkjenne alvorlig sykdom hos barn tidlig. Sykepleien. 2017;105(61904):(e-61904). DOI: 10.4220/Sykepleiens.2017.61904
Comments