Nurses’ experiences of working on a ward with an infection outbreak
Summary
Background: Outbreaks of resistant bacteria are a growing challenge in the health service, and nurses play a crucial role in managing them. However, there is a lack of knowledge about nurses’ experiences of working in outbreak scenarios.
Objective: To explore nurses’ experiences of working on a ward with a protracted outbreak of extended-spectrum beta-lactamase–producing Klebsiella pneumoniae.
Method: We used a two-phase approach, starting with an initial quantitative survey to identify relevant topics for subsequent qualitative focus group interviews. The focus group interviews were transcribed and analysed in line with Braun and Clarke’s thematic analysis.
Results: Sixteen nurses participated in three focus group interviews. Five main themes emerged from the interviews: 1) Lasting feeling of uncertainty and guilt, 2) Loss of participation in decision-making and motivation, 3) Feeling of stigmatisation and shame, 4) Reduced quality of patient care, and 5) Positive working environment as a protection mechanism.
Conclusion: The findings show that the outbreak led to a loss of motivation and professional autonomy. The study highlights the need for strategies and action plans that also safeguard the health and well-being of frontline nurses during an infection outbreak.
Cite the article
Dahl K, Vidnes T, Meyer K, Lønning K, Wahl A, Andersen M. Nurses’ experiences of working on a ward with an infection outbreak. Sykepleien Forskning. 2025;20(100048):e-100048. DOI: 10.4220/Sykepleienf.2025.100048en
Introduction
Antibiotic resistance is now one of the greatest challenges for modern medicine and is described by the World Health Organization (WHO) as a threat to global health (1). In Norway, the prevalence of resistant bacteria has traditionally been low compared with many other countries; however, infection outbreaks are an increasing threat in the Norwegian health service (2).
In its report on outbreaks of infectious diseases, the Norwegian Institute of Public Health reported that 23 outbreaks of resistant bacteria were recorded in Norwegian institutions in 2023. The number of actual cases is likely underreported (3).
An outbreak is defined as two or more cases of the same disease suspected to have a common source, or when more cases occur than expected in a specific time period and area (3, p. 6).
When resistant bacteria are detected in hospitals, extensive infection control measures and significant resources are required to limit their spread. This not only puts pressure on the institution’s resources but also affects the daily work of frontline nurses (4, 5).
Since the COVID-19 pandemic, numerous studies have been published on nurses’ management of the epidemic. However, local outbreaks of resistant bacteria differ from larger pandemics in that they are often confined to individual wards or institutions. This creates a different dynamic and particular challenges for the staff (6, 7).
Very little is known about nurses’ experiences during such local outbreaks, despite the fact that these situations are often protracted and challenging. Previous studies have primarily focused on organisational and medical aspects of outbreak management, while healthcare personnel’s experiences and psychosocial burden have received less attention (6, 7).
Low job satisfaction and high staff turnover are currently a challenge. When nurses leave the profession, valuable expertise is lost, which affects patient safety and the quality of health care (8–10).
Particularly demanding work situations, such as protracted outbreaks, can exacerbate these challenges. Given nurses’ central role on the frontline during an outbreak, it is crucial to explore their experiences in order to prepare for and manage future outbreaks. This insight is particularly important for supporting nurses and retaining them in clinical practice.
Objective of the study
The objective of the study was to examine nurses’ experiences of working on a surgical ward during a protracted outbreak of extended-spectrum beta-lactamase (ESBL)–producing Klebsiella pneumoniae (ESBL-Kp). ESBL are enzymes that are resistant to most beta-lactam antibiotics, including penicillin, cephalosporin and the monobactam aztreonam (11).
Transmission occurs through direct or indirect faecal–oral contact (12). Patients admitted to hospitals with ESBL need to be isolated (11). This requires increased resources and has several negative consequences for the carrier of the bacteria, including higher mortality, negative emotions, limited interaction with family, stigmatisation and reduced quality of health care (13–16).
Method
The study aimed to address the following research question: What were nurses’ experiences of working during a protracted outbreak of ESBL-Kp?
To explore different experiences, we used a two-phase approach, starting with a questionnaire survey. The results of this survey formed the basis for an interview guide for qualitative focus group interviews (17). This article presents the results from the focus group interviews.
Context
The study was conducted in a highly specialised surgical ward at a university hospital in Norway. From June 2019 to January 2021, more than 60 patients were infected with ESBL-Kp. Approximately one-third of the patients developed clinical infections, mainly urinary tract infections. Some progressed to sepsis and had prolonged hospital stays.
It took one year from the onset of the outbreak for ESBL-Kp to be identified in the biofilm formed in the drainpipes of toilets, showers and sinks. Ruling out other sources of infection and eradicating ESBL-Kp took approximately two years.
At the time of the interviews, no new cases had been reported in the preceding four months, and a few weeks later the outbreak was considered over. During the data collection period, 51 nurses and 5 administrative nurses were working on the ward.
All six authors of this article are nurses with research competence. The first and second authors worked on the ward as clinical nurses during the outbreak but were not study participants.
Recruitment and enrolment
We recruited participants using convenience sampling and invited all nurses on the ward to participate. Administrative staff were not invited, as their duties differed significantly from the rest of the staff. Prior to the study, the study’s aim, methodology and data protection measures were explained both orally and via individual emails.
A questionnaire and an invitation to participate in focus group interviews were sent in an electronic link via email and SMS. Participants for the focus group interviews contacted the first author, who assigned them to groups based on the duty roster.
The interviews were conducted between day and evening shifts to allow as many nurses as possible to participate. Nurses who participated in their free time were allowed to register this as work hours. Enrolment and data collection took place in May and June 2021.
Development of the interview guide and conducting focus group interviews
Due to the limited literature on healthcare personnel’s experiences during infection outbreaks, we developed a questionnaire to guide the discussion topics in the focus group interviews. The questionnaire was developed based on discussions with the nurses on the ward and among the article’s authors. It covered the themes of working environment, patient care, management’s handling of the outbreak and psychosocial health. There was also the option to provide free-text responses.
Forty-two of the 51 nurses completed the questionnaire. The results were reviewed to select relevant topics for the interview guide. Responses that revealed challenges or disagreement were included in the interview guide. For example, 74% disagreed with the statement, ‘I think it is acceptable that I have been given new tasks due to the ESBL outbreak’. This was therefore included as a topic in the focus group interviews. The interview guide consisted of the same four main themes as the questionnaire (Appendix 1 – only in Norwegian).
We opted for focus group interviews because they are well suited to capturing experiences and attitudes in an environment where many people interact. This method also generates rich and detailed data through discussion (18).
According to Malterud (18), five to eight participants per group creates the best possible dynamic in discussions. Two of the focus groups in the study had five participants, and one had six. Three focus group interviews were conducted at the hospital by external researchers. One was conducted by a single moderator. In the other two, a secretary also participated. The interviews lasted approximately one and a half hours.
Analysis
The interview data were analysed using Braun and Clarke’s six-step thematic analysis (19). The analysis involved continuous comparison and movement between the entire dataset, the coded data excerpts and the themes that formed the results. To familiarise ourselves with the data, all authors read the transcribed material independently.
The first author carried out the initial coding, which was then discussed by all authors. We subsequently developed broader themes that described the participants’ experiences during the outbreak. The codes and themes were discussed several times in order to reach consensus on the main themes. This ongoing discussion ensured consistency and coherence in the analysis, thereby increasing the trustworthiness of the results (20).
Interview participants were given the opportunity to read and comment on the results and the article. To ensure rigor in both the research process and the reporting of results, we followed the COREQ criteria for reporting qualitative research (21).
Ethics
The study was approved by the hospital’s data protection officer (reference number 21/10569). Participants completed the questionnaire anonymously so that they could not be identified, thus ensuring confidentiality. The questionnaire did not ask for participants’ sex or exact age. Completion of the questionnaire was considered consent to participate.
Because the nurses in the ward knew us, two external researchers conducted the focus group interviews. At the start of each interview, the moderator emphasised that all discussions were confidential and should not be shared outside the group. Participants signed an informed consent form prior to the interviews.
An external secretary, who had no prior knowledge of the nurses or the ward, transcribed the interviews and removed identifiable information, such as dialects and names. All data were stored on the hospital’s secure server for sensitive data. The recordings were deleted after transcription.
Results
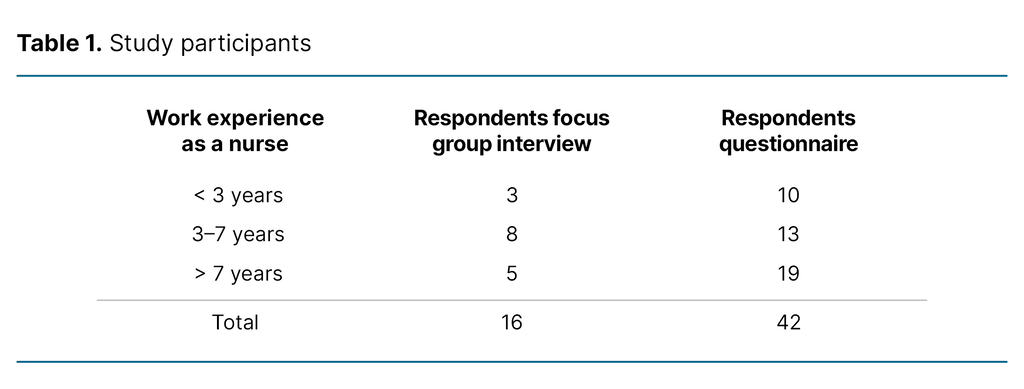
Sixteen nurses participated in the three focus group interviews (Table 1).
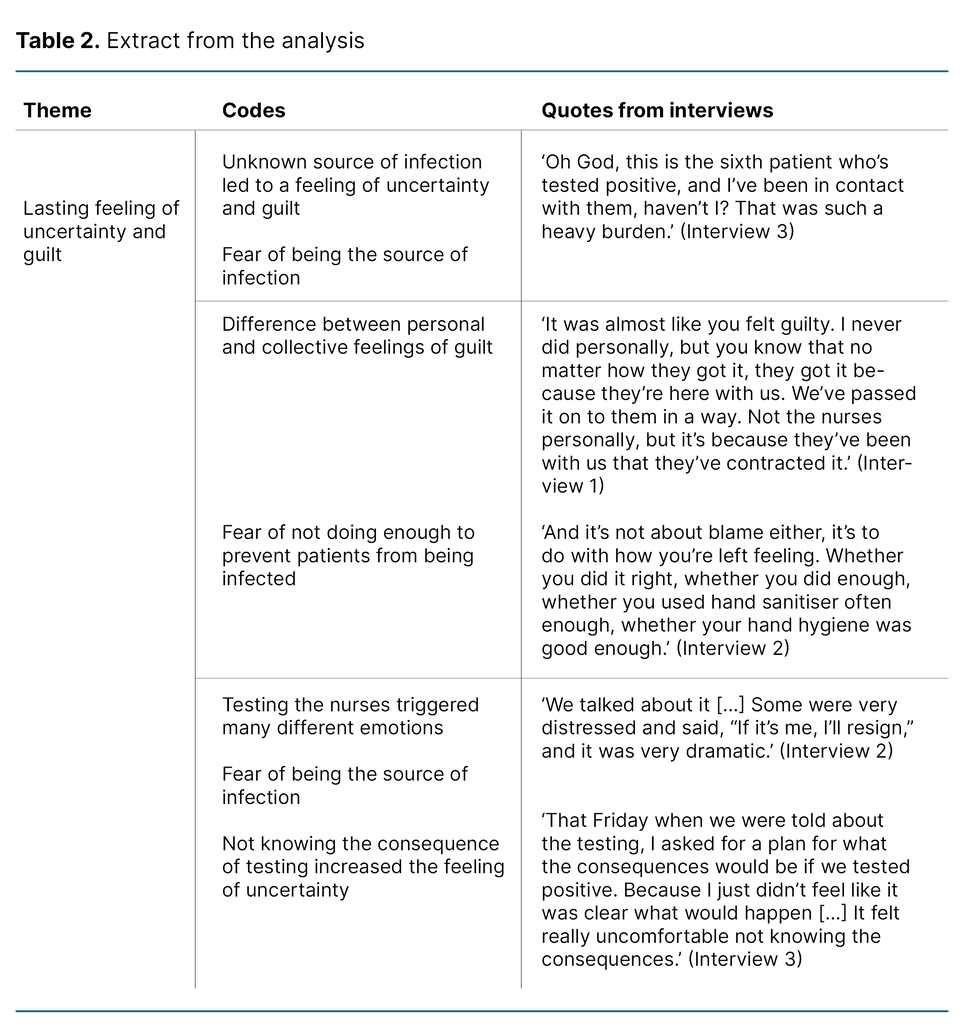
Five main themes emerged from the analysis of the focus group interviews (Table 2):
- Lasting feeling of uncertainty and guilt
- Loss of participation in decision-making and motivation
- Feeling of stigmatisation and shame
- Reduced quality of patient care
- Positive working environment as a protection mechanism
Lasting feeling of uncertainty and guilt
The nurses spent considerable time and effort trying to identify the source of the ESBL outbreak. They discussed various theories about its cause and tried to find commonalities among the patients who tested positive for ESBL-Kp. Their inability to pinpoint the source led to a lasting feeling of uncertainty, which they found extremely challenging:
‘There were so many unanswered questions; we never really got any answers because there simply weren’t any. So you have to kind of live in that ignorance.’ (Interview 2)
The participants were not worried about contracting ESBL-Kp themselves, but they feared transmitting it to patients, i.e. causing rather than preventing infection. When patients tested positive for ESBL-Kp it left the nurses with both a collective and a personal feeling of guilt. Even when some believed they were not the source, they still felt guilty because the patients were infected on their ward:
‘It’s potentially deadly for them, so you sit there thinking, have I passed on something to a patient that could kill them?’ (Interview 3)
In the search for the cause of the outbreak, it was decided that all nurses should be tested for ESBL-Kp. This had not been done previously, and many of the nurses described feeling uncertain about the consequences of testing positive. They were, for example, afraid of losing their jobs or being reassigned elsewhere.
This uncertainty triggered a wide range of emotions. Some expressed anxiety, psychological stress and frustration, while others accepted the testing without letting it affect them emotionally. The prospect of testing positive was troubling as no treatment was available for those who did:
‘There were widely differing opinions on that. Some took it very personally and became upset, you know, anxious. It was a wide range of emotions. And others were like, okay, well, let’s get tested then. But I remember that period [...] it was pretty chaotic. There were a lot of emotions.’ (Interview 2)
For most participants, the lasting feeling of uncertainty had a considerable impact on their working day. Some described it as all-consuming. A few participants also explained how the uncertainty and feeling of guilt affected their everyday lives outside of work.
Loss of participation in decision-making and motivation
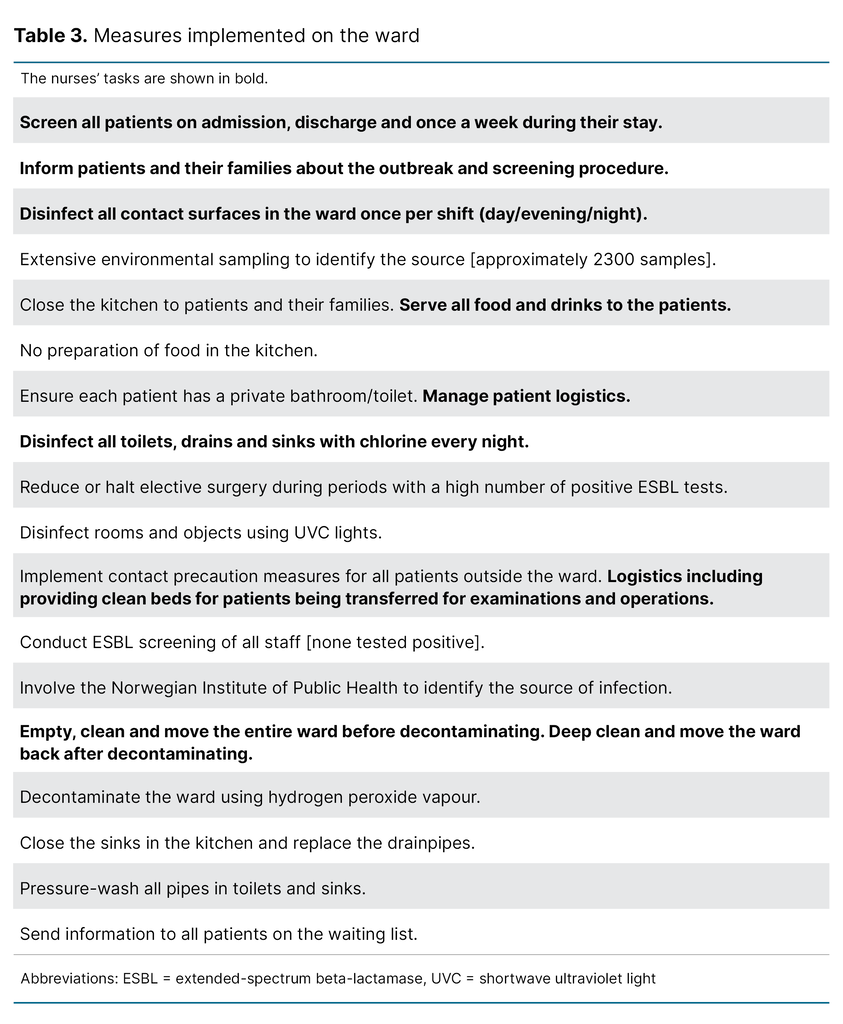
As the source of the outbreak was unknown and there was no overarching plan for managing it, a number of new tasks were introduced, both to identify the cause and to prevent the spread of ESBL-Kp. However, none of the measures were effective, resulting in a constant stream of new tasks and an increased workload (Table 3).
The participants described how they were allowed to suggest new measures but had little influence over the existing ones. Participants in all three focus group interviews discussed how their work was dominated by tasks they felt they were overqualified for, such as serving food and cleaning. This made them feel devalued as nurses. The lack of opportunity to participate in decision-making, coupled with ineffective measures that were mostly unrelated to nursing, left them feeling frustrated and demotivated:
‘Is it our water dispenser? Is it the coffee machine? Where is it coming from? Those were the kinds of thoughts running through our heads, and we became more and more desperate. And so did the infection control team and management, ultimately resorting to a bunch of awful measures and such like, and we just didn’t understand why we couldn’t get the outbreak under control, at all levels.’ (Interview 3)
‘Everyone has times when they’re a bit fed up of their job – that’s normal – but for an entire ward to feel that way at the same time, that’s scary. And that’s what happened. We were all a bit deflated in terms of job satisfaction and everything else, and it wasn’t good.’ (Interview 2)
Feeling of stigmatisation and shame
In all the interviews, the participants described how the nurses felt they were stigmatised by healthcare personnel outside the ward. The efforts to prevent the spread of infection went unnoticed by other wards and the participants feared that outsiders thought they were not doing enough to manage the outbreak.
The participants described encounters with healthcare personnel who questioned their competence as nurses, were suspicious, and levelled indirect accusations at them. This led to feelings of shame and a reduced sense of professional pride:
‘I’ve worked here a long, long time, and I’ve always been so proud of working here! […] But at that point I wasn’t proud to work here. I felt we were seen as a dirty ward. And you could hear it – don’t you nurses up there understand about hygiene? So it changed the way I thought about myself and the ward.’ (Interview 3)
Patients were also stigmatised. The nurses described how healthcare personnel from other wards working alongside them lacked knowledge about how to handle the patients or the staff from the ward:
‘And when we went with the patients for surgery, they just stood there and didn’t even greet the patients.’ (Interview 2)
Seven months into the outbreak, the health service was also hit by the COVID-19 pandemic. The nurses described how the ESBL-Kp outbreak was associated with more shame and stigma than COVID-19. COVID-19 affected everyone, whereas the ESBL-Kp outbreak was only in their ward.
The participants discussed how ESBL-Kp can intensify the stigma, as the bacteria colonise the intestines and are transmitted through faeces. Motivation was also different: COVID-19 was a common enemy, while ESBL-Kp was a problem solely for their ward:
‘It [COVID-19] affected everyone! The whole world! Every ward in the hospital. I think what was so problematic with ESBL was that it was with us, we were the troublesome ward, in a way.’ (Interview 3)
Reduced quality of patient care
The ESBL-Kp outbreak also had negative consequences for patients and resulted in a reduced quality of care. Outside the ward, all patients were treated under contact precautions, even those who tested negative for ESBL. All patients in the ward were last on the list for operations and examinations. Participants described how, in some cases, patients did not receive postoperative monitoring in the intensive care or postoperative unit because there were insufficient resources to manage contact precautions:
‘So I said, “I’m not taking him back to the ward, at the end of the corridor in an isolation room on a Saturday night.” They said that PO [the postoperative unit] can’t take him because he’s contagious […] It was really unfair to the patient, he should have been in PO. And that’s just one of many cases.’ (Interview 1)
With the source of the outbreak unknown, the nurses found it difficult to provide patients with balanced and sufficient information about the outbreak, the risk of transmission and potential complications of ESBL-Kp. The lack of standardised information was challenging, particularly when patients received different information that they then discussed.
One year after the outbreak, all patients were provided with written information prior to admission to hospital. This information was useful, and the nurses found that patients were better prepared for the situation upon arrival at the ward. The participants felt that patients were able to give informed consent to treatment, despite the outbreak:
‘I remember it was a bit uncomfortable in admissions trying to explain it before they had received the [information] sheet, because I didn’t really know what to say. And many asked, “What happens if I get it?”, because they could potentially develop sepsis and become seriously ill, but you can’t really say that. I found that very difficult.’ (Interview 1)
Positive working environment as a protection mechanism
At the onset of the outbreak, the ward had a team of experienced nurses. As a consequence of the outbreak, followed by COVID-19, several of the nurses considered moving to another workplace. Increasing workload, tedious tasks, fewer patients and greater disparities in patient care affected the nurses’ motivation for their work.
However, certain mechanisms were crucial in helping them cope with the situation. In all three interviews, the participants emphasised the protective role of the positive working environment that had been in place before the outbreak. The nurses valued the opportunity to share experiences, frustrations and concerns, and highlighted the importance of discussing these with colleagues, since friends and family could not understand what they were going through:
‘It was also a place where you could let off steam, because no one at home would understand what you were dealing with. So, it sort of became natural to talk about it there.’ (Interview 2)
Sharing experiences with colleagues fostered a sense of solidarity. This was particularly important when the nurses felt that either they or their patients were being stigmatised. Humour was considered an important coping mechanism that strengthened this sense of solidarity. The participants also described the working environment as non-judgemental and characterised by mutual trust, making it easier to share experiences with colleagues:
‘When she [a nurse from another ward] shouted, “Should you be here?!”, I felt like a pariah, and if I hadn’t been able to return to my ward and receive support from my colleagues, I would have found it very difficult.’ (Interview 3)
Finally, the participants emphasised the importance of having a supportive charge nurse who made it clear that she was on their side and who passed on their frustrations to higher levels within the organisation.
Discussion
In the focus group interviews, the nurses described a workday marked by a lasting feeling of uncertainty and guilt. They experienced loss of autonomy and control over their work and felt stigmatised by colleagues in other wards. The nurses also reported a decline in the quality of patient care.
These factors combined reduced participants’ motivation and eroded their professional pride. A positive finding, however, was that a supportive working environment served as a protective factor in dealing with these challenges.
Professional authority involves being able to make independent decisions and utilise personal competence in the day-to-day work (22). Professional autonomy fosters nurses’ perception of their role as meaningful (23) and improves the quality of their work (24).
A focus on professional autonomy thus leads to increased patient safety (23), which is important for retaining nurses in the profession (22). According to Pursio et al. (22), four elements are essential for professional autonomy: shared leadership, professional skills, professional collaboration and a healthy working environment. These elements align closely with the findings of this study and are therefore used as a theoretical framework in the discussion.
The nurses felt like they lost control
Shared leadership includes, among other things, the ability of staff to influence their own work situation. The nurses in our study described reduced participation in decision-making, an increased workload and a sense of losing control. The loss of control was particularly evident in connection with the ESBL testing of staff. Although the testing was voluntary, opting out placed nurses in a moral dilemma, as they would remain an unresolved piece of the puzzle. If the nurses chose to be tested, a positive result would create further uncertainty, as the implications of a positive test were not clearly defined.
Several nurses mentioned in the interviews that they would have resigned if they had tested positive. Nevertheless, most of the nurses chose to undergo testing. Although no one tested positive, our data suggest that the ward should have been better prepared, as the testing exposed nurses to considerable uncertainty and stress.
Support from management, but stigmatisation from other wards
Shared leadership also entails supportive management, which has positive effects on nurses’ professional autonomy (22). The focus group interviews highlighted how a supportive manager was crucial for nurses being able to cope with the protracted outbreak.
Professional skills entail nurses’ knowledge being valued within professional collaborations (22). However, the nurses in this study felt demeaned and not respected in their interactions with professionals from other wards. A key finding of the study was the nurses’ experiences of stigmatisation from colleagues in other wards.
A scoping review of healthcare personnel’s experiences during the COVID-19 pandemic also revealed considerable challenges related to stigmatisation, both from other colleagues and from the general public, which caused psychological stress, anxiety, grief and depression (25).
The ESBL-Kp outbreak was more stressful than COVID-19
Our study provides important insight into how even local outbreaks of resistant bacteria can lead to stigma similar to that experienced during pandemics. Although COVID-19 was a greater global threat, the nurses found the ESBL-Kp outbreak to be more distressing from a psychosocial perspective. Psychosocial distress should therefore be taken into account in future outbreak management planning.
The findings of this study indicate a need to develop competence across wards for managing resistant bacteria. Zingg et al. (26) emphasise the importance of the organisation taking responsibility for training and multidisciplinary collaboration in outbreak management.
Better knowledge dissemination may have reduced the stigma experienced by the nurses and strengthened the professional collaboration between wards. It could also have had a positive effect on patient care, which the nurses perceived as diminished due to stigmatisation and a lack of knowledge about infection control.
A positive finding in the study was the significance of the working environment as a protective factor. The participants found support in one another and emphasised the importance of being able to share experiences and frustrations. This form of debriefing was particularly important because the nurses felt that no one else could understand the burden of working during an outbreak.
This finding is consistent with the literature highlighting the importance of social support as a buffer against burnout and turnover among nursing staff (27). Our findings underscore the importance of facilitating this type of support in outbreak situations, for example through structured debriefing sessions and open channels of communication.
Strengths and limitations of the study
Using a questionnaire as the basis for developing the interview guide ensured that the focus group discussions covered topics relevant to the nurses’ experiences during the outbreak. This strengthened the quality of the data and provided richer insights into the nurses’ professional challenges.
The study was conducted shortly after the outbreak ended, which enhances its trustworthiness, as the participants’ experiences were still fresh in their minds. Although the study only included a small number of nurses from a single ward, the results may be relevant for other healthcare workers experiencing various types of infectious outbreaks.
Conclusion
The study illustrates how an outbreak of resistant bacteria in a hospital ward can lead to nurses losing motivation and professional autonomy. The complexity and high level of competence required in the specialist health service highlight the importance of supporting staff during an outbreak.
Identifying nurses’ vulnerabilities in outbreak scenarios is crucial for safeguarding their mental and physical health. Understanding the stressors associated with an outbreak can help prevent nurses from resigning, thereby maintaining the level of expertise necessary to sustain a professional standard.
Lack of knowledge and an absence of outbreak action plans appeared to be key contributors to the negative experiences reported by the nurses. The study highlights the need for strategies that also protect the health and well-being of healthcare personnel in outbreak situations.
Acknowledgements
We would like to thank the nurses who shared their experiences in this study. We would also like to thank Sigrid Cecilie Skøyeneie and Elna Hamilton Larsen, who conducted the focus group interviews, and Sofie Nordby, who transcribed them.
The authors declare no conflicts of interest.
Open access CC BY 4.0



Comments