Barriers to the delivery of enteral nutrition in intensive care unit patients – a descriptive cross-sectional study
Summary
Background: Intensive care unit patients are particularly subject to malnutrition, which is associated with high risk for a number of complications. The European Society for Clinical Nutrition and Metabolism (ESPEN) recommends delivery of enteral nutrition rather than other methods where peroral intake is not possible.
Objective: The objective of the study was to map the barriers to enteral nutrition in intensive care units (ICUs) nationally. We also wanted to investigate whether the barriers varied according to registered nurses’ (RNs) clinical experience and education, or between local/regional hospitals and university hospitals.
Method: We conducted a cross-sectional study with a descriptive design. A slightly adapted, professionally translated version of an internationally validated questionnaire mapping the prevalence of 21 barriers to enteral nutrition was sent to all ICUs in Norway with adult patients as their main treatment group. A total of 129 of 1,213 RNs from 24 different units answered the questionnaire.
Results: The most commonly reported barriers were ‘Enteral nutrition halted before procedures or operations’, ‘In critically ill patients, other aspects of patient care still take priority over nutrition’, and ‘Delays and difficulties in obtaining small bowel access in patients not tolerating enteral nutrition (e.g. ventricle retention)’. RNs with more than ten years’ clinical experience evaluated the first two items as less challenging than colleagues with less experience. Four of the ten greatest barriers were reported to occur more commonly at university hospitals than local/regional hospitals. No differences were found for the other six barriers.
Conclusion: The study shows a significant number of barriers to enteral nutrition in the ICUs in the study. Over half of the respondents specifically mentioned fasting prior to procedures as a significant problem. The prevalence of barriers seemed to vary somewhat between hospital departments and among personnel with different levels of experience. The respondents frequently reported the lack of availability of a dietician, but the statements in the questionnaire should be revised before further use. We recommend that future research and quality improvement efforts target the most common barriers in order to achieve the greatest clinical benefit.
Cite the article
Thu E, Voldsund S, Sand K. Barriers to the delivery of enteral nutrition in intensive care unit patients – a descriptive cross-sectional study . Sykepleien Forskning. 2025;20(98756):e-98756. DOI: 10.4220/Sykepleienf.2025.98756en
Introduction
Malnutrition and undernutrition frequently occur in patients who are hospitalised in somatic hospital departments, where one in three patients is at risk of undernutrition. The corresponding risk in ICUs can be over 70 per cent (1). Moreover, it has been demonstrated that the nutrition prescribed and administered to patients during their ICU stay is less than their estimated needs (2, 3). Malnutrition in ICU patients is associated with increased risk of infections, prolonged time on ventilator, longer length of stay, and increased mortality (4–6).
The term ‘malnutrition’ can refer to both overnutrition and undernutrition. The Norwegian Directorate of Health uses it as a collective term for conditions where there is an imbalance in the intake and/or uptake of nutrients (7). Critical illness, trauma and intensive care affect the ICU patient’s metabolism, nutritional status and nutritional needs (6).
The guidelines of the European Society of Clinical Nutrition and Metabolism (ESPEN) primarily recommend oral nutritional delivery during the ICU stay (6). If the ICU patient is unable to ingest adequate nutrients, enteral nutrition (EN) is recommended rather than parenteral delivery.
Some studies find that early enteral nutrition leads to reduced hospitalisation, duration of mechanical ventilation, morbidity and mortality (8). Enteral nutrition can be started despite abnormal bowel function, for example when bowel sounds or flatus are absent (6).
The initiation of enteral nutrition should be delayed in the case of haemodynamic instability, but can be started for patients who are stabilised with a low dose of catecholamines and/or infusions (6). It has been demonstrated that quality improvement projects and implementation of nutritional procedures can promote an increase in the use of enteral nutrition (9).
Cahill et al. developed and validated a questionnaire to map the barriers to enteral nutrition. They found an inverse correlation between the prevalence of reported barriers and the delivery of enteral nutrition (10, 11).
Since then, the questionnaire has been used in a number of international studies, indicating that these barriers exist in different countries and cultures (12–14). It is recommended that barriers are mapped for the relevant population or organisation where improvement is desired with the aim of tailoring measures to overcome the main barriers (15).
From a national perspective, there is a lack of knowledge about the prevalence of barriers to enteral nutrition in ICU patients in Norway. The objective of this study is to map these factors. We compared reported barriers at group level with the aim of generating hypotheses.
The groups that were compared were: 1) staff at local/regional hospitals and university hospitals; 2) RNs with short-, medium- and long-term work experience; and 3) RNs with or without advanced clinical education.
Method
Study design
We conducted a cross-sectional study with a quantitative descriptive design. The participants were RNs and specialist nurses from ICUs in Norway who primarily treat ICU patients over the age of 18 years. The nurses had at least six months experience in the ICU in which they were working during the study. Staff on leave or sick leave were not included. Data were collected from April to July, 2023.
The questionnaire was answered and digital consent given on the online portal eFORSK (16). The study was submitted to the former Norwegian Centre for Research Data, now Sikt – Norwegian Agency for Shared Services in Education and Research (Reference number 517858). The study was approved by the data protection officer at the Norwegian University of Science and Technology (NTNU), as well as the local data protection officers at the participating hospitals. De-identified raw data were used in the analysis.
Our aim was to include as broad a sample of the population as possible. All ICUs in Norway were therefore contacted, and 24 of 59 units consented to participate. Contact persons in the units distributed the questionnaire to relevant participants. A reminder was sent after four weeks, which increased the response rate by four per cent.
A total of 129 (11 per cent) of 1,213 possible respondents answered the questionnaire. In the case of the 35 units that did not participate, either the health trust or the unit did not wish to participate (n = 5), there was no response to our request (n = 29) or feedback arrived after the conclusion of the data collection period (n = 1).
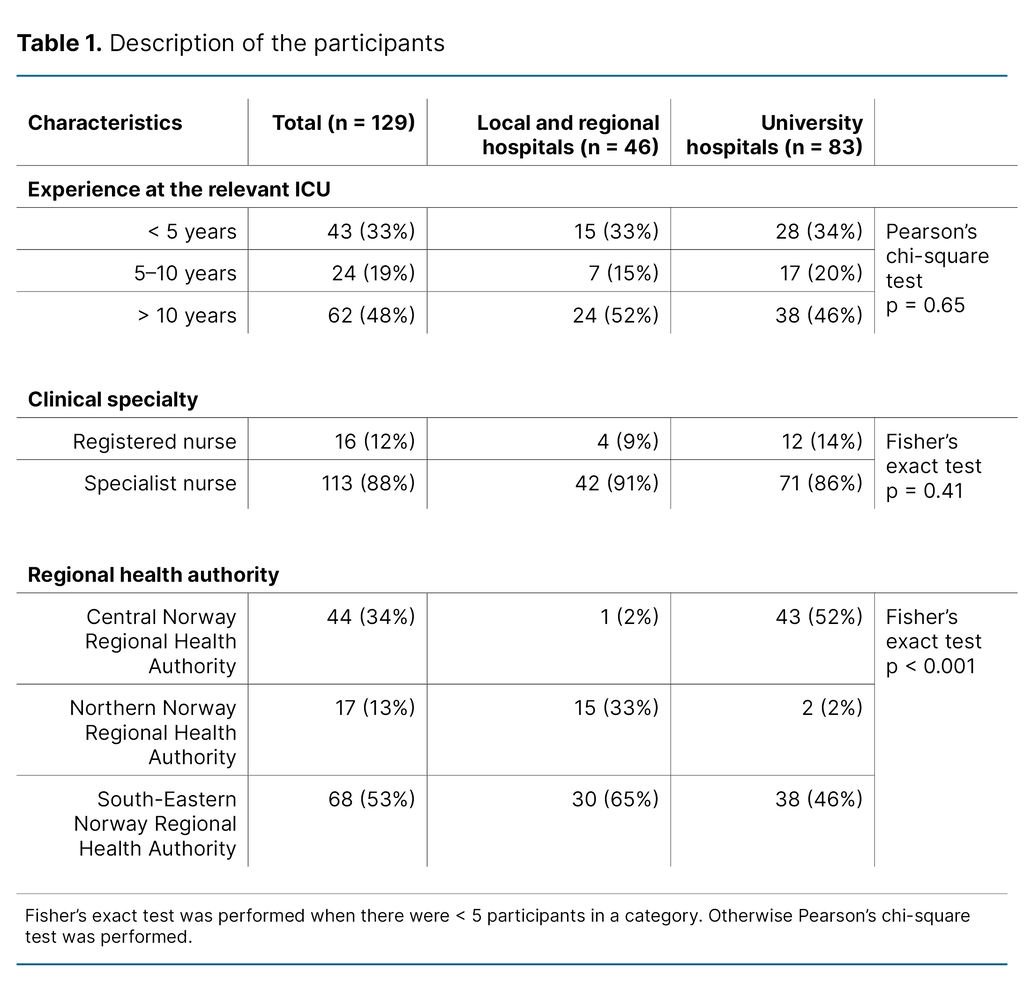
No collected data were excluded. Experience and clinical specialty were evenly distributed between local/regional hospitals and university hospitals, but recruitment in relation to the various health trusts was skewed (Table 1).
Barriers to delivery of nutrition in critically ill patients
We used a Norwegian version of Cahill’s Barriers Questionnaire (10). The questionnaire was translated into Norwegian in connection with a quality improvement project at Oslo University Hospital in 2016. The original author was involved in a ten-step process with translation and cultural adaptation. The Norwegian translation is freely available on the Critical Care Nutrition website (Barrierer for ernæring av kritisk syke pasienter )(17).
The questionnaire was distributed to a pilot group so that they could give feedback on the instrument prior to further distribution. The feedback from the pilot group did not indicate any need to adjust the questionnaire. The pilot group’s responses were not included in the dataset.
The questionnaire consisted of three parts. Part A contained 21 statements about barriers to feeding ICU patients enterally. Items 1–7 are combined under the theme ‘Delivery of enteral nutrition to the patient’, items 8–11 under ‘Dietician support’, items 12–13 under ‘ICU resources’ and items 14–21 under ‘The attitudes and behaviour of ICU personnel’.
Each statement was rated on a seven-point Likert scale. The respondents were asked to describe the degree to which each statement was perceived as a barrier in their ICU, from 0 ‘not at all’ to 6 ‘an extreme amount’. The response alternatives ‘a lot’, ‘a great deal’ and ‘an extreme amount’ were combined as in earlier studies (10–13, 18), and are referred to as ‘barriers’ from here on.
Part B contained demographic questions while in Part C, respondents could give free text comments on the questionnaire. The respondents were required to answer all questions in Parts A and B before submitting the questionnaire.
In the original version, Part B contained four categories relating to seniority and experience: 0–5, 6–10, 11–15 and > 15 years’ experience. In our study, the last two categories were combined because the group with more than 15 years’ experience was small. The 6–10 years’ group was smaller than the other two, but we retained it because we found it interesting to compare relatively inexperienced ICU nurses with two groups with longer seniority and experience.
The data in Part A had a normal distribution with the exception of items 9 and 10. In Part C, several respondents also gave free-text comments indicating that these two items were difficult to understand. A test of the instrument’s internal consistency using Cronbach’s alpha showed that this increased from 0.797 to 0.813 after the exclusion of items 9 and 10. Following an overall assessment of these factors, we decided to exclude these items from the ten most commonly reported barriers. However, they will be reported and discussed separately.
We compared categorical demographic variables using Pearson’s chi-square test or Fisher’s test. To compare the rating of barriers between variables with two categories, we used the independent t-test. For three categories we used the one-way ANOVA-test with Tukey’s honest significant difference (HSD) post-hoc analysis. The analyses were conducted using SPSS version 29, while R version 4.3 was used for the figures. Two-sided p-value < 0.05 was regarded as statistically significant.
Results
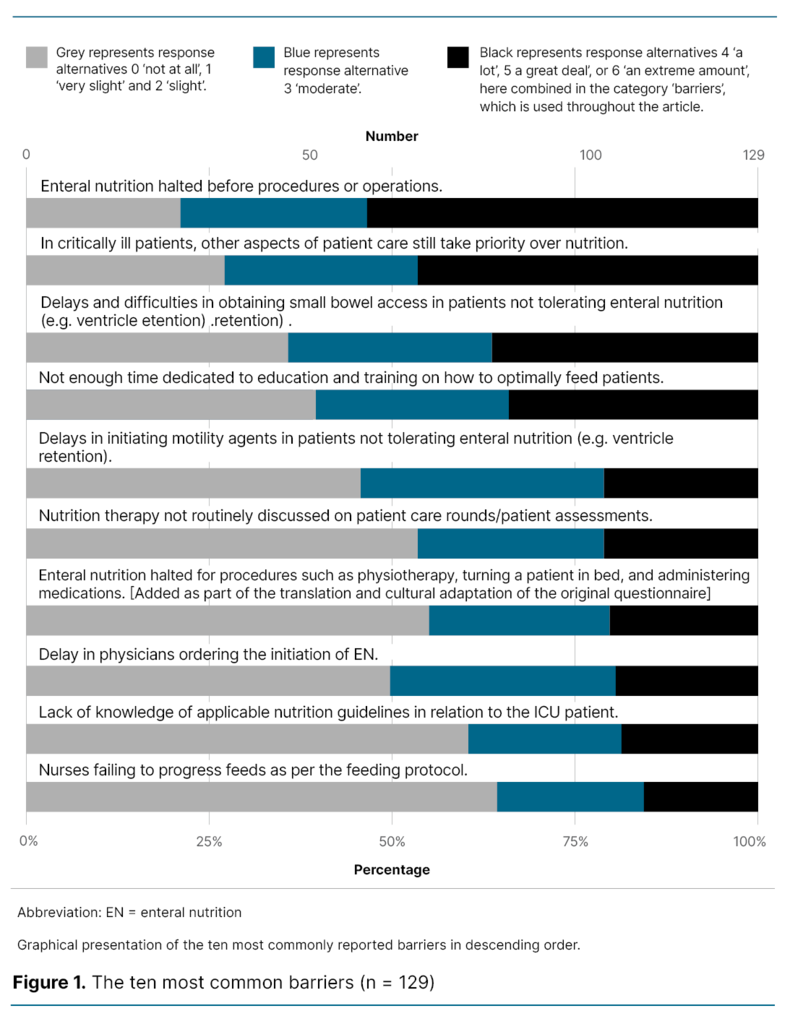
The most commonly reported barriers were item 19 ‘Enteral nutrition halted before procedures or operations’ (69/129, 53 per cent), item 6 ‘In critically ill patients, other aspects of patient care still take priority over nutrition’ (60/129, 47 per cent), item 5 ‘Delays and difficulties in obtaining small bowel access in patients not tolerating enteral nutrition (e.g. ventricle retention)’ (47/129, 36 per cent) and item 11 ‘Not enough time dedicated to education and training on how to optimally feed patients’ (44/129, 34 per cent).
Moreover, the most commonly reported barriers from four to ten are also given. These were reported with declining frequency by 44 to 20 of 129 respondents (34 and 16 per cent respectively). Figure 1 shows the ten most commonly reported barriers in descending order from greatest to smallest.
The most common barriers were item 9 ‘Dietician not routinely present on weekday patient rounds’ (71/129, 55 per cent), and item 10 ‘No or not enough dietician coverage during evenings, weekends and holidays’ (77/129, 60 per cent). These items are omitted from Figure 1 because we received feedback that they were difficult to understand and that the instrument attained a somewhat higher Cronbach’s alpha without them.
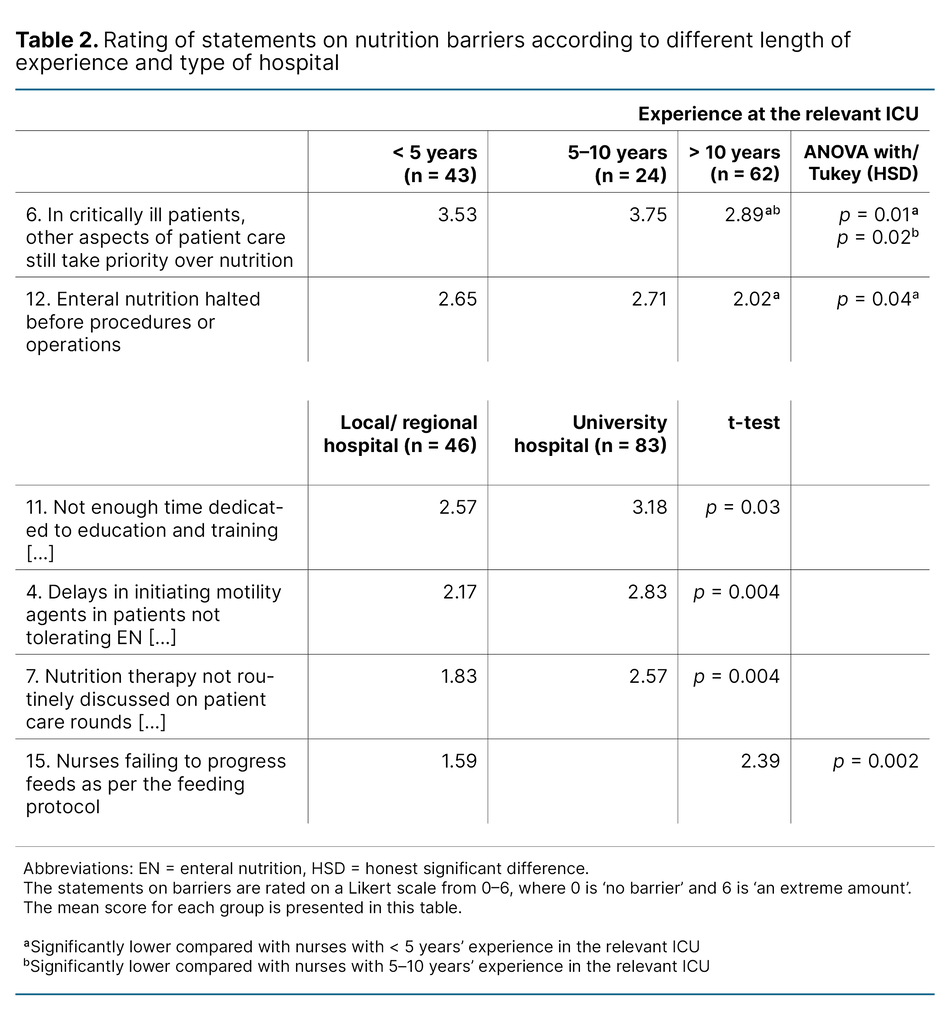
Table 2 compares different subgroups. When we compared the rating of the ten most commonly reported barriers at university and local/regional hospitals, we found that barriers 11, 4, 7 and 15 were evaluated as greater (p < 0.05) at the university hospitals.
The barrier ‘In critically ill patients, other aspects of patient care still take priority over nutrition’, was rated lower (p < 0.05) by nurses with over 10 years’ experience compared with groups with 5–10 and 0.5–10 years’ experience.
Nurses in the group with 0.5–5 years’ experience reported the item ‘Enteral nutrition halted for procedures such as physiotherapy, turning a patient in bed and administering medications’ as a greater challenge compared with nurses with more than ten years’ experience.
We found no significant differences in the ratings of the ten most commonly reported barriers among nurses with advanced clinical education compared with those without.
Discussion
The respondents in this study reported a high prevalence of several known barriers to the delivery of enteral nutrition at ICUs in Norwegian hospitals. The barriers most commonly reported are linked to fasting prior to procedures, prioritisation of other areas of patient care, challenges in establishing a jejunostomy tube, and a lack of time for education and training.
Enteral nutrition halted before procedures or operations
ICU patients are often subject to procedures or operations that may entail fasting. This was the most commonly reported barrier in the study, and 53 per cent of the respondents stated that it hindered them in the delivery of enteral nutrition. A systematic review article by Ros et al. identifies fasting as one of the most common reasons for interruption of the delivery of nutrition (4).
In a retrospective cohort study from the United States, nutrition delivery was halted for 4.8 hours daily on average between days two and six of the ICU stay. The main reasons for these pauses were presumed to be extubation, fasting before procedures, loss of enteral access, ventricle retention, and radiology suite procedures (2).
Nurses with more than ten years’ experience rate fasting in connection with procedures as less of a barrier (p < 0.05) compared with colleagues with less than five years’ experience. ICU nurses have a complex area of responsibility in a stressful working environment (19–21). Studies show that the learning environment in ICU nursing is challenging. Much has to be learned in a short period of time, while good time management and the ability to prioritise are also expected (20, 21).
The ability to establish good routines, optimalise time management and improve prioritisation skills is developed over time. Less experienced nurses have a greater need for mentors or guidelines in connection with complex treatment (22). The lack of procedures and standardised time intervals for fasting in the case of intubated ICU patients is an issue that has been discussed earlier (14, 15, 20). We were unable to find national guidelines or procedures for fasting in the case of intubated ICU patients.
In critically ill patients, other aspects of patient care still take priority over nutrition
The next most common barrier in our study was that enteral nutrition was given lower priority than other issues in critically ill ICU patients. According to the available literature, ICU personnel recognise the importance of enteral nutrition, but state that it is given lower priority in a number of situations (23). However, earlier studies have shown that it is possible to influence several of the factors that delay delivery, and a number of nurses pointed out the importance of prioritising nutrition (24).
Nurses with more than ten years’ experience also rated this barrier as lower. It is conceivable that nurses with longer experience are more familiar with ways of optimalising nutrition while also attending to procedures and taking care of the patient’s other needs.
It is important to note that the content of this item in the questionnaire differs somewhat from the original. There it was emphasised that the prioritisation of other procedures applies to haemodynamically stable patients, who, according to guidelines, might be candidates for enteral nutrition. This may mean that the barrier reported in this study is potentially overestimated.
This study did not explore the situations in which nutrition is given lower priority or the reasons for this. A lack of knowledge about correct nutrition and the significance of hard outcomes may also result in lower prioritisation. Not devoting enough time to education and training on how to optimally feed patients is the fourth most common barrier in the study. This was also found to be more prevalent at university hospitals.
A lack of education and training may be the result of a busy workday with increasing demands as to productivity and efficiency (25, 26). More focus on and training in enteral nutrition can optimalise its administration (3, 27).
Delays and difficulties in obtaining small bowel access in patients not tolerating enteral nutrition (e.g. ventricle retention)
Delayed jejunal access was the third most commonly reported barrier to delivery of enteral nutrition in ICU patients. Enteral feeding intolerance and ventricle retention are regarded as some of the most common reasons for the interruption of delivery of enteral nutrition (4). In patients with ventricle retention where medication has been given without effect, the establishment of jejunal access is subject to delays (6).
The insertion of a jejunostomy tube requires special competence, and the lack of personnel can thus be a limiting factor. Nonetheless, reports on this barrier did not vary between university and local/regional hospitals where the availability of personnel with such skills might be expected to differ.
On the other hand, nurses at university hospitals reported that the failure to discuss nutrition therapy on patient care rounds was a greater barrier (p < 0.05). A number of studies highlight the advantages of using a daily goals checklist during rounds in order to optimalise delivery of nutrition, among other things (28–30).
If nutrition is not discussed during the round, it is likely that the detection of ventricle retention and the initiation of motility agents will be delayed, or that the failure to comply with nutrition protocols will not be discovered. Using a nutrition protocol can ensure that more ICU patients achieve their nutritional goals (31).
It is uncertain why university hospital nurses rate the four barriers as greater (p < 0.05) when compared with local/regional hospitals. A possible reason may be differences in patient conditions, where university hospitals treat different patient groups than local/regional hospitals and offer intensive monitoring and interventions that cannot be carried out at local/regional hospitals. This may entail that nutrition delivery is given lower priority in favour of other treatment. Another explanation may be that dissimilar recruitment from different regions and hospital size can have impacted on the results.
There is little literature available on differences in the barriers to enteral nutrition at local or university hospitals, but a Chinese study (13), in which a locally adapted version of Cahill et al.’s questionnaire was used, found greater barriers at local hospitals. The authors discussed whether the differences could be attributed to a lack of resources at smaller hospitals, but these results can probably not be compared directly with Norwegian conditions.
Nurses with and without advanced clinical education
We did not find any differences between the responses of respondents with advanced clinical education compared to those without. However, there was a considerable bias in relation to respondents, as 88 per cent of the responses were from personnel with such education. Bloomer et al. (24) found no differences in the extent to which nutrition was given priority in patient treatment when comparing health personnel with different educational backgrounds.
Support of a dietician
Items 9 and 10, relating to the availability and support of a dietician during patient rounds and nursing shifts, were not included amongst the ten most commonly occurring barriers due to skewed data and feedback that the statements were difficult to understand. Some respondents saw the lack of availability of a dietician in the unit or hospital as a barrier, but were uncertain which question to use to report this. Future studies should therefore include a question on whether the hospital has a dietician or not.
Providing the correct nutrition to an ICU patient can be challenging because of the patient’s altered metabolism in connection with acute illness or injury. Enteral nutrition must be specifically adapted to the patient’s condition because both over- and underfeeding can result in a number of complications (32). A multidisciplinary approach including support from a dietician can give better outcomes for ICU patients, as well as shorter ICU stays (33).
It is likely that all the barriers mentioned above vary from hospital to hospital and among the various ICUs in line with available resources, local guidelines and culture. This highlights the value of mapping barriers at the local level in the institution seeking improvement.
Strengths and limitations
This study is the first national mapping of barriers to the delivery of enteral nutrition in ICU patients. The use of an internationally recognised and validated questionnaire developed to map barriers to enteral nutrition in ICUs is a strength. The questionnaire was systematically translated into Norwegian earlier, in cooperation with the original author (17).
Cronbach’s alpha shows that the questionnaire has a high internal consistency. Free-text comments in response to items 9 and 10 indicated that the statements could be misunderstood. We also note that item 6 deviates somewhat from the original questionnaire, as pointed out above. This was not discovered when we pilot tested the questionnaire, but the wording of these items should be evaluated prior to further use of the Norwegian version and should be adapted to local conditions if appropriate.
We wanted to include as many informants as possible and invited all ICUs in Norway to participate. However, the respondents come from only three of the four health regions, with some bias in the subgroups as shown in Table 1. The low response rate and the total number of responses mean that we cannot generalise the findings to apply to all nurses at Norwegian ICUs, but must interpret the results with caution (34).
However, the study does provide some insight into the barriers that can occur in Norwegian ICUs because it includes respondents from 24 different ICUs. Our findings on the most common barriers concur with findings in comparable international studies (10, 12, 14, 18), and this strengthens our results.
Web-based questionnaires are known to have a lower response rate (35). The requirement to log in using a recognised form of electronic ID may have raised the threshold for participating in the study. These factors combined may have led to data bias in that only the nurses who were most interested in nutrition responded (34). A different form of distribution should be evaluated for future surveys or there should be stronger local focus to ensure that the results can be generalised.
Our study may encourage ICU personnel to pay more attention to the barriers to the delivery of enteral nutrition in ICU patients. These can be reduced by mapping them and becoming more aware of them. To obtain an overview of the barriers that exist at the individual ICU, the questionnaire used in this study can be utilised in local quality improvement projects.
Conclusion
This study reports the barriers to enteral nutrition in Norwegian ICUs for the first time. The barriers most commonly reported are that nutrition is halted in connection with procedures, nutrition is given lower priority in relation to other procedures and that jejunal access is delayed in patients with ventricle retention.
Nurses with over ten years’ experience evaluated the prioritisation of nutrition and fasting in connection with procedures as less of a barrier than colleagues with shorter experience. The questionnaire used to map the barriers is freely available and may be useful in further research and quality improvement projects.
Espen Løver Thu and Stian Voldsund share first authorship.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge









Comments