The significance of theory and clinical placement for students’ nursing competence
Summary
Background: Theoretical knowledge and clinical placement are the main components of nursing education. There are a number of studies that have focused on students’ assessments of theory and clinical placement in nursing education. Few studies have focused on the significance of theory and clinical placement courses for nursing students’ professional competence after completing their nursing education.
Objective: The study aimed to examine nursing students’ assessments of theory and clinical placement courses and their self-reported nursing competence. It also aimed to look more closely at the significance of theoretical knowledge and clinical placement for students’ nursing competence.
Method: This is a cross-sectional study of nursing students at an educational institution in Norway who completed their education in 2019. The data were collected using an online questionnaire. Nursing competence was measured using the Nurse Professional Competence Scale Short Form (NPC Scale–SF). The response rate was 63%.
Results: In terms of preparing them for the nursing profession, nursing students attribute statistically significant greater importance to clinical placement than theory courses in their education. The students have high scores in all competence areas, but score highest in the competence area ‘Value-based nursing care’ and lowest in ‘Development, leadership and organisation of nursing care’. The analysis shows a correlation between students’ assessments of theory and clinical placement courses and several of the nursing competence areas. Theory courses have somewhat greater significance for nursing competence than clinical placement courses.
Conclusion: The study shows that students consider clinical placement courses to be the most important for their future nursing career. It also shows that theory courses have a somewhat greater significance for students’ nursing competence than clinical placement courses.
Cite the article
Kirchhoff J. The significance of theory and clinical placement for students’ nursing competence. Sykepleien Forskning. 2024;19(94772):94772. DOI: 10.4220/Sykepleienf.2024.94772en
Introduction
Since the early days of nursing education, theoretical knowledge and clinical placement have been the main components in the education of nurses (1, 2). Both components are important and mutually dependent in the development of students’ nursing competence and identity (3, 4). This article focuses on how nursing students’ weight theory and clinical placement while studying, as well as the importance of theoretical knowledge and clinical placement in students’ self-reported nursing competence after completing their nursing education.
Despite nursing competence being considered to be fundamental to professional nursing practice, there is no uniform definition of this concept (5). EU Directive 2013/55/EU on the recognition of professional qualifications (6), which helps regulate the content of Norwegian nursing education, describes the competence areas for nursing. These have been further expanded upon by the European Federation of Nurses Associations (7), and include, for example, assessing nursing care needs, diagnosis, planning, implementation and evaluation.
Other competence areas that have been expanded are culture, ethics and values, health promotion and prevention, guidance and instruction, decision-making, communication and cooperation, research, development and leadership. These also correspond to the World Health Organization’s (WHO) global standards for the initial education of nurses (8), in which both theoretical knowledge and clinical placement contribute to attaining nursing competence.
A number of studies show, however, that nursing students value clinical placement more highly than theoretical knowledge (9–11), and consider clinical placement periods to be the most important aspect of their education. The opportunity to practise procedures, gain insight into patients’ experiences of being ill, get to know their own limitations and develop self-confidence are some of the reasons that students’ assign substantial weight to clinical placement (13–15).
Consequently, nursing students express a need for more clinical placement and simulation-based education in order to be prepared for the nursing profession (11, 16, 17). Studies also indicate that the right conditions must be in place to ensure that clinical placement promotes learning, such as longer clinical placement periods, good relationships with placement supervisors that offer opportunities for reflection, and variation in the nursing care provided to patients (18–23).
Despite the fact that students attach the greatest importance to clinical placement periods during their studies, they also recognise the value of theoretical knowledge in order to become qualified nurses (3, 24). However, they expect knowledge to be relevant to their future professional practice and for theory to be linked to clinical placement (25).
Previous studies show that nursing students rate theoretical knowledge in courses in nursing care, medicine and science, pathophysiology and pathology higher than, for instance, the philosophy of science or social science knowledge (9, 16, 25). Vågan et al. (9) describe this as a technical-instrumental view of knowledge.
The studies that are presented show that researchers have predominantly focused on nursing students’ ranking and assessment of theoretical knowledge and clinical placement during their nursing education. There are, however, few studies that have examined how theoretical knowledge and clinical placement impact on their nursing competence after completing their education.
Among the exceptions are Høegh-Larsen et al.’s study (17) of the importance of simulation-based education (SBL) and clinical placement in nursing students’ self-reported nursing competence. Their findings indicates that both SBL and clinical placement are of importance in nursing students’ self-reported competence in several nursing competence areas (17).
Objective of the study
The aim of the study is two-fold. To begin with, the intention was to examine nursing students’ assessments of theory and clinical placement courses and self-reported nursing competence. The main objective was to examine the correlation between students’ self-reported nursing competence and their overall assessments of theory courses and clinical placement periods during their nursing education.
Method
Design
In order to realise the study’s objective, a cross-sectional study of final year students at an educational institution in Norway was carried out.
Sample
All nursing students at Østfold University College who completed their education in spring 2019 were invited in May that year to participate in an online survey. Of the 139 students who were to graduate, 78% responded to the questionnaire. This resulted in a response rate of 63%.
Data collection
The students were invited to participate in the study and fill in a questionnaire via email. The questionnaire was distributed using Nettskjema, which is an application for preparing and conducting online surveys administered by the University of Oslo (26).
The questionnaire contained introductory questions about the students’ background and their overall assessment of the theory courses and clinical placement periods during their studies. The theory courses and clinical placement periods were assessed on the basis of the following question: ‘Overall, to what extent have theory courses/clinical placement courses during your nursing education prepared you for the nursing profession?’ A five-point Likert scale was used for responses (1 = ‘To a very small extent’, 5 = ‘To a very large extent’)
In addition, the students’ self-reported nursing competence was examined using the Nurse Professional Competence Scale Short Form (NPC Scale–SF). This is a simplified version of the NPC Scale, which has been developed and validated to survey self-reported nursing competence (5, 27).
The instrument has been developed in accordance with the standards and strategies of the EU and WHO (6, 8), and consists of 35 items distributed across the following six competence areas: ‘Nursing care’ (5 items), ‘Value-based nursing care’ (5 items), ‘Medical and technical care’ (6 items), ‘Care pedagogics’ (5 items), ‘Documentation and administration of nursing care’ (8 items), and ‘Development, leadership and organisation of nursing care’ (6 items) (27).
A seven-point Likert scale was used in relation to each item (1 = ‘To a very small extent’, 7 = ‘To a very large extent’). The instrument has been translated and adapted to a Norwegian context (28). It has been used both internationally and in Norway to survey nursing competence (17, 29–31). The responses are converted into an index for the various competence areas, giving a score from 0 to 100. A score of 100 means that the respondent believes that they are competent in a particular area ‘to a very large extent’.
Analysis
The responses were analysed using IBM SPSS, version 28. Descriptive statistics were used to describe the students’ backgrounds, their assessments of theoretical knowledge and clinical placement, as well as their self-reported nursing competence.
Bivariate analysis was performed to determine whether there were any correlations between the students’ backgrounds and their assessment of theoretical knowledge and clinical placement on the one hand and their self-reported nursing competence on the other. The analysis included cross tables, chi-squared tests and non-parametric correlation analyses using Kendall’s Tau as a correlation co-efficient. The Wilcoxon test was conducted to examine the correlation between the students’ assessments of theory and clinical placement courses. A significance level of 5% was selected.
Ethical considerations
The study was carried out in accordance with the Declaration of Helsinki’s ethical principles for medical research (32) and approved by the Norwegian Centre for Research Data (NSD), reference number 890325. The students were informed about the study. By filling in the questionnaire in the Nettskjema application, they consented to participate in the study.
Results
Most of the students who participated in the study were women (97%) aged 20–25 years (61%) who had work experience in the health and social services sector prior to commencing nursing studies (56%). In addition, the majority of the students (92%) worked in the health and social services sector during their studies, primarily for less than 10 hours per week (Table 1).
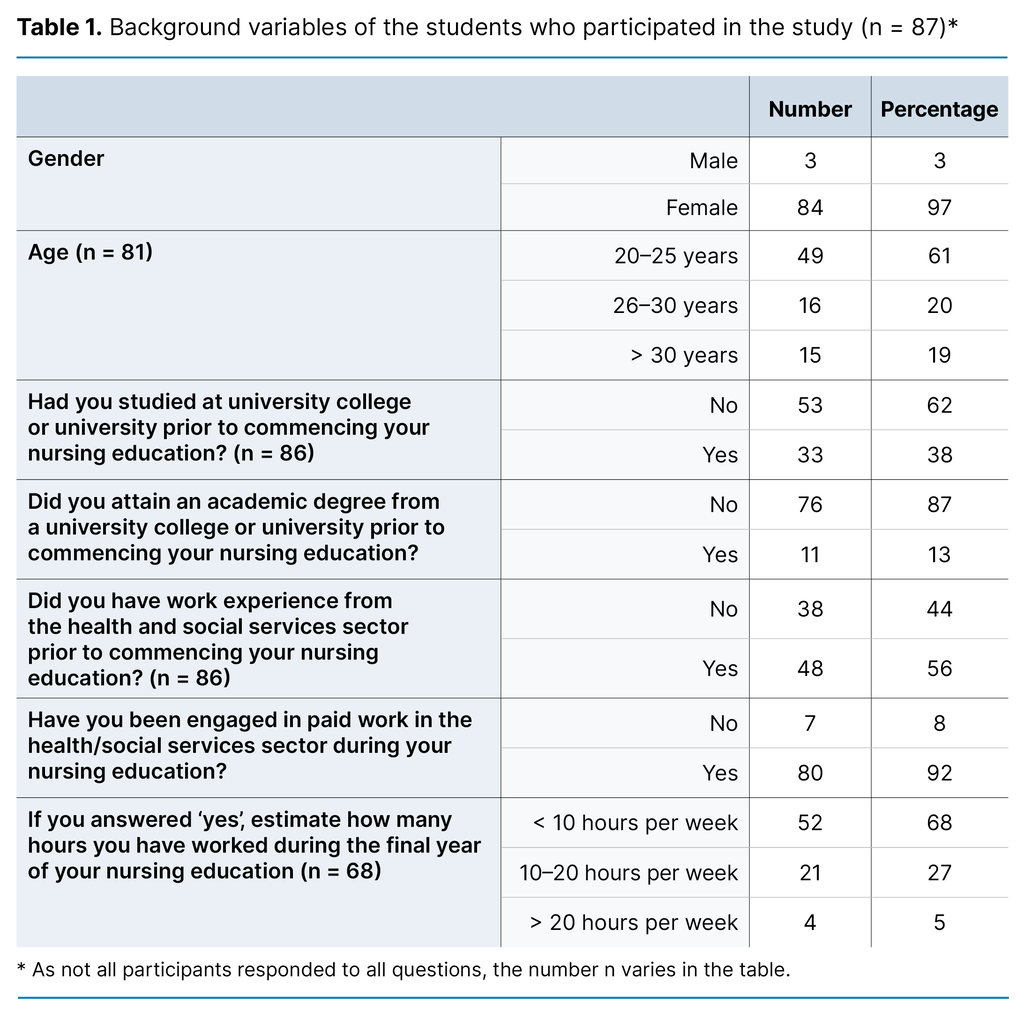
Table 2 shows the students’ responses on the extent to which they considered theory and clinical placement courses to have prepared them for the nursing profession. The table indicates that a greater proportion of students responded that the clinical placement courses ‘to a large extent’ or ‘to a very large extent’ had prepared them for the nursing profession (93%) than the theory courses (80%).
The Wilcoxon test proved that the difference in the students’ assessment of theory and clinical placement courses was statistically significant (p < 0.01). There was no correlation between the students’ backgrounds (Table 1) and their assessment of theory and clinical placement courses.
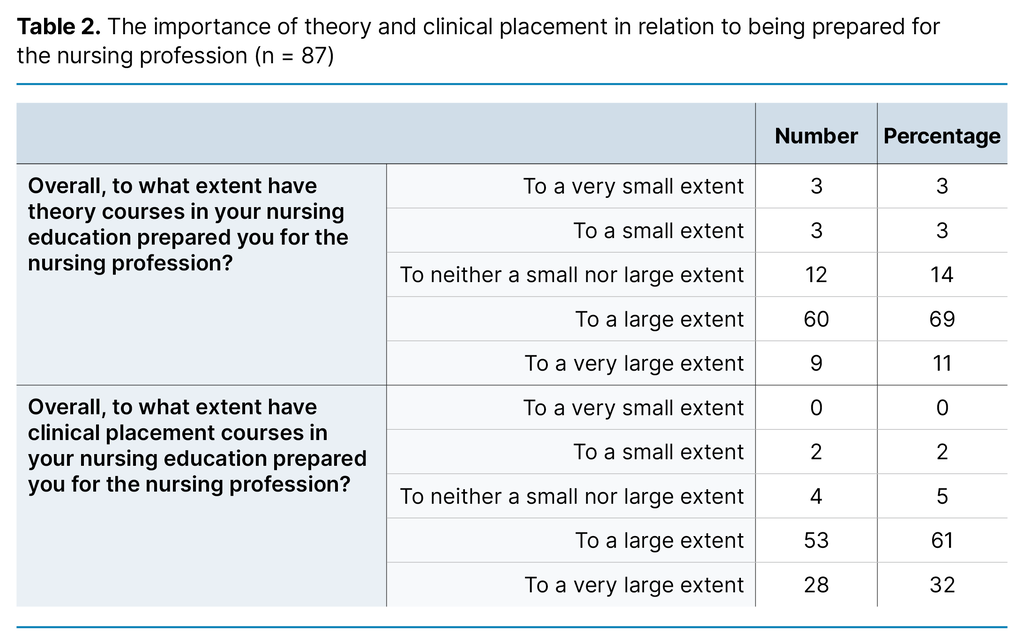
Table 3 shows the students’ self-reported competence linked to the competence areas in the NPC Scale–SF.
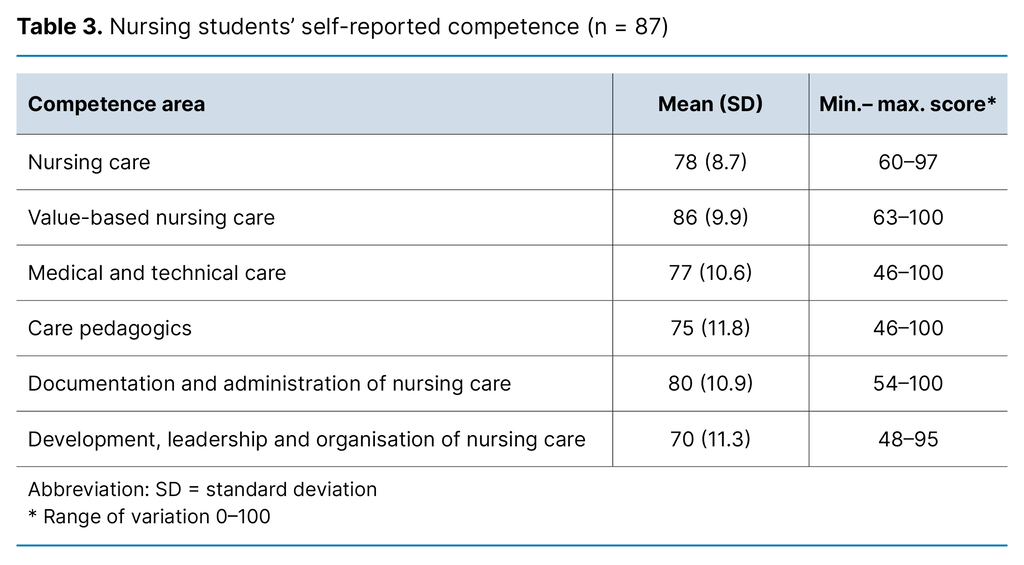
The table shows that the students’ highest score was in the competence area ‘Value-based nursing care’ and the lowest was in ‘Development, leadership and organisation of nursing care’. In addition, it shows that the range of variation was greatest for the competence areas ‘Medical and technical care’ and ‘Care pedagogics’. The analysis showed that there were no correlations between the students’ backgrounds (Table 1) and their scores in the various competence areas in the NPC Scale–SF.
The last table shows the findings of the bivariate analysis of the correlations between the students’ assessments of the theory and clinical placement courses and the various competence areas (Table 4). Overall, it shows a correlation between students’ assessments of the theory and clinical placement courses and their self-reported nursing competence.
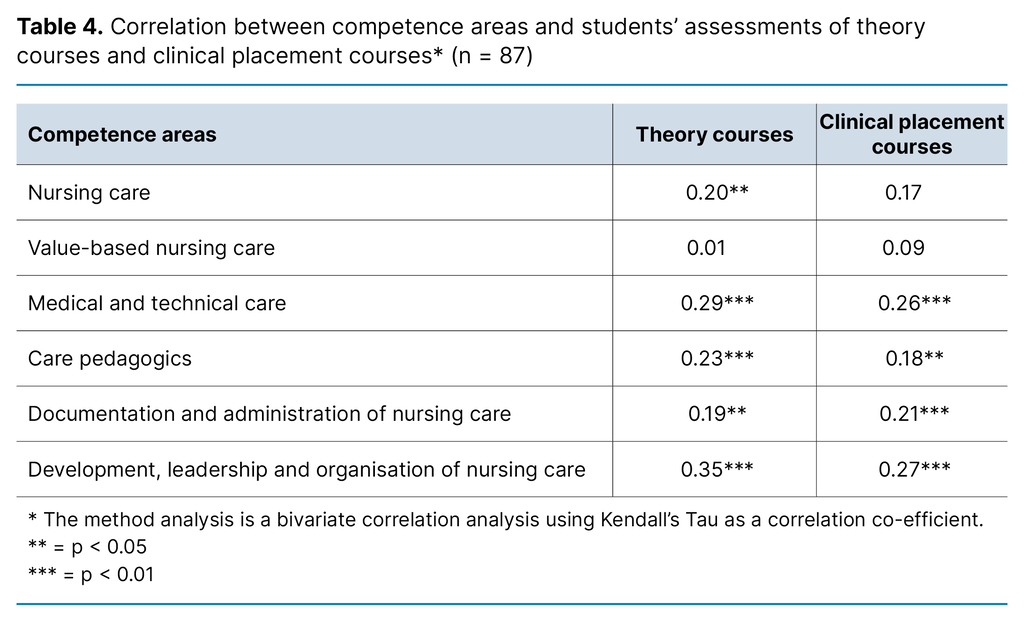
With the exception of the competence area ‘Value-based nursing care’, the table shows statistically significant correlations between the students’ assessments of the theory and clinical placement courses and most of the competence areas. If the students assessed that the theory courses prepared them for the nursing profession, an increase in their self-reported competence within the competence areas could also be seen. This correlation was strongest in the competence areas ‘Development, leadership and organisation of nursing care’ (Kendall’s Tau = 0.35) and ‘Medical and technical care’ (Kendall’s Tau = 0.29).
Moreover, Table 4 shows that there were significant correlations between the students’ overall assessment of clinical placement courses in several competence areas, and this was strongest in the competence areas ‘Development, leadership and organisation of nursing care’ (Kendall’s Tau = 0.27) and ‘Medical and technical care’ (Kendall’s Tau = 0.26). There were no correlations between students’ assessments of the clinical placement courses and the competence areas ‘Value-based nursing care’ and ‘Nursing care’.
In addition, the differences in the strength of the correlation factors between the students’ assessments of theory and clinical placement courses within each competence area indicated what was of greatest importance for the various areas. For example, the table shows a stronger correlation between the competence area ‘Development, leadership and organisation of nursing care’ and the students’ assessment of theory courses than that between this competence area and their assessment of clinical placement courses. Conversely, there was a slightly stronger correlation between the competence area ‘Documentation and administration of nursing care’ and the clinical placement courses than was the case with the theory courses.
Discussion
Firstly, this study shows that, like previous studies, nursing students attach more importance to clinical placement than theory courses in relation to being prepared for the role of nurse (9–11). Secondly, it indicates, in addition to the high score in most of the competence areas, that there was variation in the nursing students’ self-reported competence towards the end of their studies. They perceived having the highest level of competence in the competence area ‘Value-based nursing care’, while ‘Development, leadership and organisation of nursing care’ received the lowest score.
The high score of the students in the competence area ‘Value-based nursing care’ was also a finding in previous studies (5, 12, 17), while their low score in ‘Development, leadership and organisation of nursing care’ corresponds with studies that show that newly qualified nurses often lack this competence (33, 34). One possible explanation for this is that nursing education is aimed at clinical practice and work with patients (17), as well as the fact that the goal of nursing education in this competence area is primarily action preparedness rather than action competence (35).
What is the reason for the students’ high score in ‘Value-based nursing care’?
An interesting finding in this study, however, is the lack of statistical correlations between the students’ assessments of theory and clinical placement courses and specific competence areas. This particularly applies to ‘Value-based nursing care’, where there is a high score in the competence area but there is no statistical correlation between the competence area and the students’ assessments of theory and clinical placement courses. However, this does not mean that theory and clinical placement courses are of no significance for development in the competence area.
A possible explanation may be that an overall assessment of the importance of the courses for the nursing profession, as formulated in the questionnaire, is not specific enough to determine which theory or clinical practice courses help to develop the students’ competence in ‘Value-based nursing care’.
Another explanation may be linked to a previous study, which found that there are factors other than theory and clinical placement that are of significance for ‘Value-based nursing care’. For example, Lillemoen (36) found that students justify their moral conduct on the basis of personal characteristics.
The lack of a correlation between the students’ assessment of clinical placement and the competence area ‘Nursing care’ can, however, be due to other causes. This competence area requires competence in basic nursing care. Examples include being able to follow the nursing process, meeting patients’ basic needs and documenting patients’ health status, which are skills students learn early in their nursing education. This study was, however, carried out towards the end of their nursing education, when clinical placement courses are, to a greater extent, aimed at attaining competence in other areas, such as ‘Medical and technical care’ and ‘Development, leadership and organisation of nursing care’
The significance of theory and clinical placement for students’ nursing competence
Of most interest, however, are the positive correlations between the students’ assessments of theory and clinical placement courses and their self-reported nursing competence. To start with, this study, like Høegh-Larsen et al. (17), found statistically significant correlations between clinical placement and several of the competence areas on the NPC Scale–SF.
Yet there is a difference. In Høegh-Larsen et al.’s (17) study, statistically significant correlations were found between clinical placement and all of the competence areas on the NPC Scale–SF, whereas this study did not find similar correlations connected to the competence areas ‘Nursing care’ and ‘Value-based nursing care’.
Differences in the study design may partly account for this, since Høegh-Larsen et al. (17) carried out a longitudinal study that encompassed both SBE and clinical placement during different phases of the nursing education, while the findings in this article are based on a cross-sectional study carried out at the end of the nursing education. The main point, however, is that both studies indicate that students’ assessments of the clinical placement courses appear to have importance for a wide range of competence areas within nursing competence and the development of a professional identity during studies (3).
Theory courses are of slightly more importance than clinical placement courses for students’ nursing competence
Furthermore, this study indicates that the students’ assessments of the importance of theory courses appear to have slightly more impact on their nursing competence than clinical placement courses, even though the students consider clinical placement courses more important than theory courses for their future nursing role.
Two factors help to underpin this. Firstly, the students’ assessments of theory courses correlate with more of the competence areas than the clinical placement courses do. In addition, the strength of the statistical correlations between the students’ assessments of theory courses and the various competence areas is often greater than those of clinical placement courses. For example, the correlation coefficient of the correlation between the students’ assessment of theory courses and the competence area ‘Medical and technical care’ is greater than the correlation between the same competence area and their assessment of the clinical placement courses.
One possible explanation could be the importance of pathology classes and other scientific subjects, which represent a considerable proportion of the theory courses in nursing education. These are theoretical subject areas that students consider important for the practice of nursing care (25), and which are closely connected to the competence area ‘Medical and technical care’. However, no similar studies have been found to enable the comparison of these findings.
Overall, the findings indicate that students’ assessments of theory and clinical placement courses alone are not sufficient to conclude what has the greatest importance for developing students’ nursing competence. To examine the importance of theory and clinical placement, the content of the various components of nursing education needs to be linked to the areas for nursing competence. Studies that link assessments of theory and clinical placement courses with assessments of nursing competence will, for that reason, contribute valuable information on the importance of the courses in relation to the various areas within nursing competence.
Strengths and weaknesses of the study
Despite a high response rate, the data were only collected from one educational institution. Furthermore, there were relatively few male participants compared to the proportion of male students who completed nursing education. This led to bias in the sample (37). It is not therefore possible to generalise the findings of this study to all nursing students who complete bachelor’s degrees in nursing. Nevertheless, given the sample size and response rate, it may contribute to a study with a probability sample finding similar correlations and thereby strengthen the external validity of the findings (37).
Another weakness is connected to the internal validity, that is, to what extent it is possible to draw conclusions regarding causal relationships between the importance of theory and clinical placement courses and the students’ self-reported nursing competence. The correlations that are presented in the results indicate causal relationships. However, they are insufficient to be able to draw the conclusion that A (e.g. students’ assessment of the importance of clinical placement courses) leads to B (self-reported nursing competence) (38). A design that checks other possible causation variables would be able to strengthen the internal validity of the results, as in the case of a longitudinal intervention study.
The strength of the study is its use of the NPC Scale–SF to measure students’ self-reported nursing competence. The NPC Scale has been translated and tested for a Norwegian context. The reliability tests resulted in a satisfactory Cronbach’s alpha in all competence areas, which strengthens the study’s conceptual validity (38).
Conclusion
The study shows that nursing students attach greater importance to the clinical placement periods than the theory courses during their nursing education in relation to being prepared for the nursing profession. However, this difference does not mean that clinical placement courses are of greater significance for the development of students’ nursing competence.
The study indicates that both theory and clinical placement courses are of approximately the same value for the students’ self-reported nursing competence, but that the theory courses have somewhat greater significance than the clinical placement courses. There are, however, limitations to the sample and the design that necessitate further investigation.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge







Comments