Operating room nurses’ experiences with redeployment and task shifting during the COVID-19 pandemic
Summary
Background: In March 2020, Norway was hit by the COVID-19 pandemic. Major challenges for the health service were anticipated, and plans were made to treat a large number of patients in a short period of time. The number of planned surgeries was reduced. Operating room nurses were redeployed to help meet the need for nurses for a potentially large number of patients with COVID-19. Redeployment involved being allocated tasks in a setting other than the operating room.
Objective: The objective was to explore operating room nurses’ experiences of how their professional expertise was utilised during redeployment in the first two waves of the COVID-19 pandemic.
Method: We recruited a strategic sample of operating room nurses who had been redeployed during the early waves of the COVID-19 pandemic. Semi-structured individual interviews were held with the help of an interview guide. Digital audio recordings of the interviews were transcribed verbatim. The data were analysed using the NVivo 12 data analysis software, based on Braun and Clarke’s reflexive thematic analysis.
Results: The study shows that operating room nurses’ professional competence was underutilised during the first two waves of the COVID-19 pandemic. Crisis management differed across health authorities because they were not well prepared for a crisis and faced challenges relating to information flow and resource management. Operating room nurses experienced an increased psychological and ethical burden. The pandemic was managed in solidarity with society and in accordance with professional standards. The operating room nurses felt frustrated during the pandemic because they found that patient safety was compromised to some extent, particularly when the task shifting involved entirely new patient-facing duties in relation to critically ill patients.
Conclusion: In the next major crisis situation, hospitals should have more detailed plans for how to utilise the specific competence of operating room nurses. Transparent and appropriate information and resource management will also be crucial success factors. The allocation of tasks in hospitals needs to be more aligned with employees’ work-life balance in order to prevent burnout and significant shortages of essential nursing competence, and to reduce the risk of compromising patient safety.
Cite the article
Danielsen S, Vikan M. Operating room nurses’ experiences with redeployment and task shifting during the COVID-19 pandemic. Sykepleien Forskning. 2024;19(95013):e-95013. DOI: 10.4220/Sykepleienf.2024.95013en
Introduction
On 11 March 2020, the World Health Organization (WHO) declared a COVID-19 pandemic following a virus outbreak in China caused by the SARS-CoV-2 virus (1). A day later, Norway announced a national lockdown. The health service had to swiftly plan and prepare for a potential surge in critically ill patients requiring intensive care.
The images and experiences from Italy (2) in the first phase of the pandemic made a strong impression and prompted authorities to prepare for waves of sick COVID-19 patients.
Many hospitals in Norway reorganised their daily workflows (3), including a reduction in planned surgeries (4). Consequently, many operating room nurses were redeployed to other departments and allocated tasks that differed from their daily professional practice in an operating room.
In a report from 2019, the European Commission refers to the WHO’s definition of task shifting from 2008 (5): ‘the rational redistribution of tasks among health workforce teams’. Norway’s Healthcare Personnel Commission stated that ‘[t]he distribution and/or redistribution of responsibilities and tasks must be based on strategic competency mapping and competency planning’ (6, p. 129).
Furthermore, the Healthcare Personnel Commission believes that ‘effective task shifting is built from the bottom up’ (6, p. 129). Research has shown that vertical task shifting does not necessarily reduce the quality of the healthcare services provided (7, 8). However, task shifting should not entail reducing the nursing staff or increasing workloads, as these two factors significantly raise the risk of a poorer quality of care and compromised patient safety (9).
In Norway, perioperative nursing is practised according to a specific professional standard (10) and requires a master’s degree in perioperative nursing, as governed by the Regulations on National Guidelines for Perioperative Nursing Education (11). Sections 7 and 8 of the regulations state respectively that operating room nurses must have advanced expertise in infection control and lead relevant infection control efforts. The professional standard is defined by the Norwegian Nurses’ Organisation’s specialist group of operating room nurses (NSFLOS) and outlines operating room nurses’ responsibilities and scope of practice.
Operating room nurses engage in direct patient care involving health promotion and preventive, curative and palliative care according to the patient’s needs. The other areas relate to management, coordination, professional development, research and dissemination (10). The professional standard and section 4 of the Health Personnel Act (12) in combination state that operating room nurses have an evidence-based approach to their daily work, thus contributing to patient safety.
This is the first study in a Norwegian context that qualitatively explores and sheds light on operating room nurses’ experiences with redeployment during the COVID-19 pandemic.
Objective of the study
The objective of the study was to explore operating room nurses’ experiences with how their professional competence was utilised during the first two waves of the COVID-19 pandemic.
Method
Study design
We designed a qualitative study and developed a semi-structured interview guide. A combined deductive-inductive approach was planned, with reporting according to the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist (Appendix 1) (13).
Study context and participants
The study was conducted in May and June 2021, shortly after the second wave of COVID-19 patients were hospitalised in Norway. The study participants were operating room nurses at four hospitals in South-Eastern Norway Regional Health Authority. The COVID-19 patient flow was similar in these hospitals during the first two waves in Norway starting in March 2020. We used a strategic sampling method to include operating room nurses with clinical experience of redeployment.
Data collection
We conducted the interviews based on Kvale and Brinkmann’s (14) and Braun and Clarke’s methodologies (15, 16), where the operating room nurses’ experiences were explored deductively and inductively. The individual interviews were carried out by the two authors and a colleague, all of whom have extensive backgrounds in specialised nursing.
Managers at the hospital departments invited to participate approved and facilitated the recruitment of participants. A semi-structured interview guide (Appendix 2 - only in Norwegian) was used in the interviews, and this was based on available literature and our preconception of the field and the context.
Data analysis
The audio recordings of the interviews were transcribed verbatim and the transcription was analysed using NVivo version 12. Immediately after the interviews, we took field notes of thoughts and ideas related to what was said in the interview to support the ongoing preliminary analysis and assess the richness of information in the interviews.
We analysed the data using reflexive thematic analysis as described by Braun and Clarke (15, 17). This was supported by notes taken throughout the data collection and analysis processes. Reflexive thematic analysis is performed in six phases: familiarisation with the empirical data, coding, generating themes, revising themes, defining and formulating themes and finally reporting and writing up the analysis (16).
After familiarising ourselves with the empirical data in phase one, we developed the initial set of codes. First, both authors performed an independent analysis. We then reviewed and discussed the results in two formal analysis meetings to revise codes, subthemes and main themes. Through dynamic discourse and reflexivity, we challenged our preconceptions in the analysis process in order to underpin, in particular, our inductive approach.
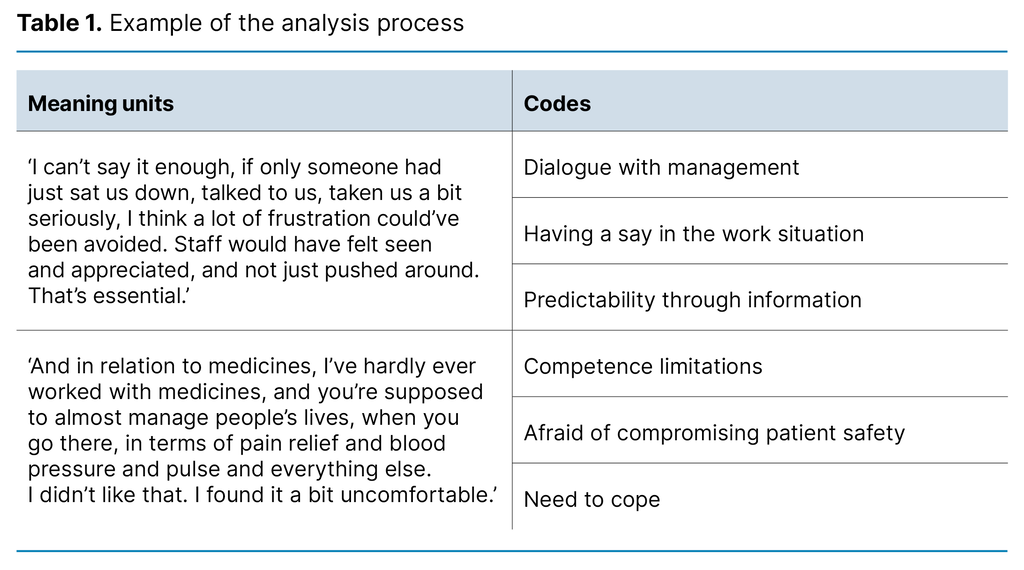
In the reflexive back-and-forth process between data, abstraction and theory, we used systematic field notes. We delineated the final main themes in an iterative process, where our interpretations were continuously revised, and generated latent content. Table 1 shows an example from the analysis process.
Ethical considerations
The former Norwegian Centre for Research Data (NSD), now the Norwegian Agency for Shared Services in Education and Research (Sikt), granted permission to carry out the project (reference number 566062). Written and oral information was given to the participants, and they provided written consent to participate.
Results
We interviewed 13 operating room nurses. All were women aged 31–64 years with experience as operating room nurses ranging from < 1 to 30 years at four hospitals, both university hospitals and local hospitals in South-Eastern Norway Regional Health Authority.
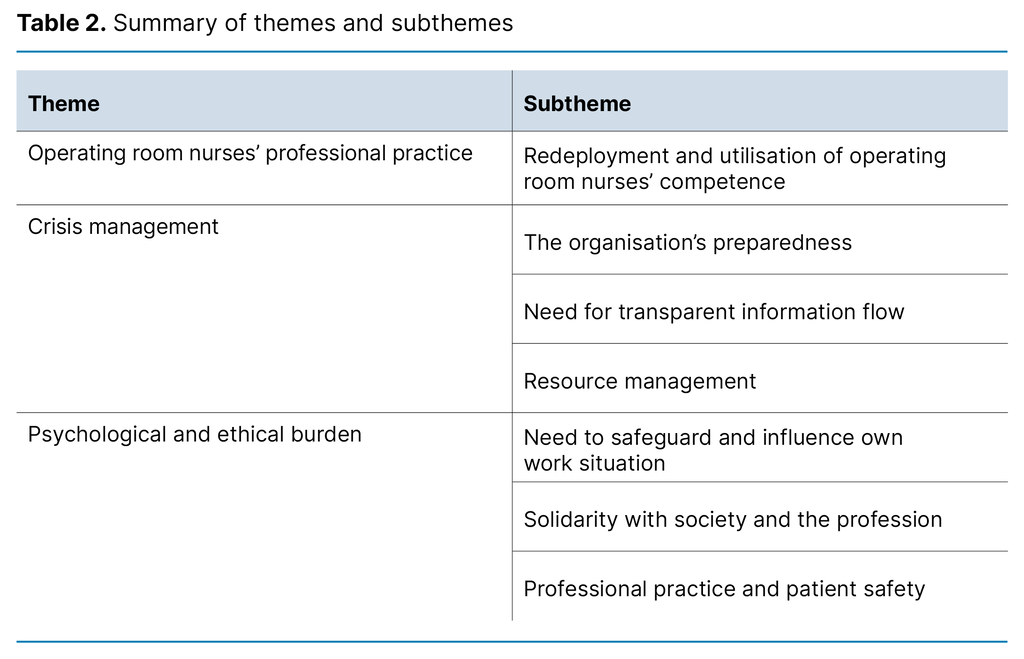
The data analysis resulted in the following three main themes: A) Operating room nurses’ professional practice, B) Crisis management and C) Psychological and ethical burden. Seven associated subthemes are presented sequentially with the main themes and are summarised in Table 2.
Main theme A – Operating room nurses’ professional practice
Operating room nurses have clearly defined tasks in the operating room, but the pandemic created a situation in which several operating room nurses were allocated tasks outside their normal responsibilities and scope of practice. Several of the operating room nurses found the task shifting challenging. Many were redeployed to basic nursing roles, and overall, their professional expertise was underutilised.
Subtheme A – Redeployment and utilisation of operating room nurses’ competence
Several of the nurses found it difficult to depart from their role of professional practitioner, while some coped well with the redeployment: ‘I do still know a bit about all of this, even though it’s been a long time since I’ve done this type of nursing.’
Several participants expressed feeling like ancillary workers, which they found tedious at times. Others tried to maintain a positive attitude: ‘It’s not like we stop being nurses just because we’ve become operating room nurses.’
Many of those who coped best with the redeployment had a background that was relevant to the new tasks. This was especially true for those with experience from emergency departments and intensive care units (ICUs).
However, despite been allocated basic nursing tasks, the participants experienced various challenges: medicines had new names, the equipment and documentation system was new, and there were new logistics in an unfamiliar place: ‘Even though I’d worked in intensive care until I became an operating room nurse, there are so many changes in relation to equipment and medicines and such like’.
There were also operating room nurses with no ICU experience and with only brief training who were left alone with patients on ventilators at times.
At some hospitals, the operating room nurses were eventually redeployed to assist with managing the flow of personnel entering and leaving the ICUs. Here, they could utilise their professional competence in infection control, both with therapeutic responsibility and in a preventive function.
The doctors and nurses working together appreciated the use of the hospitals’ practical infection control specialists to manage logistics and infection prevention in sluice rooms, which are high-risk areas. However, it also emerged that healthcare personnel outside the operating room, including doctors and nurses, are not very familiar with the core competence of an operating room nurse.
Main theme B – Crisis management
Management of available nursing resources is crucial for hospitals’ delivery of high-quality services to patients under normal conditions. Day-to-day management is challenged in a crisis situation, as was the case when a COVID-19 pandemic was declared in Norway in early 2020.
Subtheme B1 – The organisation’s preparedness
Most participants said that the hospitals’ pandemic plan was unknown both prior to and at the onset of the pandemic: ‘I don’t think there was a good plan. I don’t think anyone had sat down and looked at it or, like, I think they just sort of lined up all the staff and then just placed them.’
The poor pandemic preparedness resulted in different approaches to management of the situation. This was reflected in how redeployments were made and what tasks the nurses were allocated. At one hospital, personnel were almost switched from one place to another without there being any plan: ‘Using people correctly, well, then you have to map out people’s skills in peacetime, I almost said, not when a crisis hits.’
At another hospital, they took a clearer approach based on the actual competence of each member of staff, including previous experience, which resulted in less workload stress.
Subtheme B2 – Need for transparent information flow
Most of the operating room nurses acknowledged that hospital management tried to provide information as best they could in the prevailing situation. However, experiences with information flow management were mixed. The nurses felt everything from satisfaction to intense frustration: ‘Where I was redeployed to, they were very good at providing information. We received regular updates.’
Another added: ‘I wish someone had talked to me. If we’d been given some kind of forewarning, and prepped a bit, and knew.’
The operating room nurses recognised the importance of information transparency during a crisis, both in terms of content and form.
Subtheme B3 – Resource management
Resource management of personnel and equipment was highlighted as a major challenge during the first two waves of the pandemic. The operating room nurses considered the deployment of personnel and task shifting to be less than ideal: ‘Create a pool of people who would be willing to be moved in the next pandemic, next time it happens, so that you have a pool to draw from, with staff who have more training and are willing.’
Several participants expressed that the redeployment could have been managed more effectively in relation to previous experience and training.
There was a shortage of personal protective equipment (PPE) in the beginning: ‘We lacked some PPE, even though the management here actually said that there was no shortage of anything.’
The operating room nurses expressed loyalty to the hospital and tried to ensure appropriate distribution of the equipment. However, they were also mindful of their professional responsibility.
This responsibility entails a culture where the responsibilities and functions inherent to the profession are synonymous with quality and patient safety. It is not, therefore, surprising that equipment shortages led to frustration: ‘There was a bit of arguing about equipment.’
Main theme C – Psychological and ethical burden
The early waves of the COVID-19 pandemic challenged the operating room nurses’ balance in the work situation, both psychologically and ethically. Their professional practice was affected in various ways, which in turn made them uncertain about whether they were providing good quality of care and adequate patient safety.
Subtheme C1 – Need to safeguard and influence own work situation
Being redeployed or put on standby for redeployment, with little or no preparation, was challenging for the operating room nurses and increased the psychological burden. The participants were anxious about being assigned tasks they were not prepared for and that entailed a professional standard they were unable to relate to in terms of their responsibilities and scope of practice: ‘They hadn’t been very clear, so, then suddenly you were in a situation that wasn’t exactly optimal.’
They found that, particularly in the first wave, they did not have much of a say and were not included in the decision-making process for redeployment and the distribution of tasks: ‘I think a lot of frustration could’ve been avoided. Staff would have felt seen and appreciated, and not just pushed around. That’s essential.’
However, in the second wave, several participants found that the working situation improved somewhat: ‘Now in the second round, the management tried to be... they were actually very good.’
Subtheme C2 – Solidarity with society and the profession
The operating room nurses demonstrated solidarity and a great willingness to undertake the work of the health service when the COVID-19 pandemic hit Norway: ‘I think there were a lot of us who rolled up our sleeves and helped out wherever it was needed, whether it was in ICU, the emergency department, or on the wards.’
Even when they faced heavy workloads and challenging situations in their redeployment, they tapped into the core of their professional ethics, which helped them cope: ‘Because you knew you couldn’t refuse, because the world, society, the hospital, Oslo, the whole of Norway... you were there to help patients who needed help, so you just gritted your teeth and got on with it.’
The community spirit that prevailed in Norway also extended to healthcare personnel: ‘They were so good at helping out, those who worked there, that when things started to get critical, they were there right away.’
However, the transition was not entirely seamless for the staff. Several experienced disparities in workloads. Some were redeployed to work with the most critically ill patients in ICUs, while others sat in front of a computer working on e-learning courses or other tasks. This disparity was most prominent in the first wave, when almost no operations were performed.
Subtheme C3 – Professional practice and patient safety
The operating room nurses had different opinions on whether redeployment reduced or maintained the quality of care and patient safety. Those redeployed to ancillary functions expressed that patient safety was not directly compromised.
However, safety became a concern among those in patient-facing roles who had to work with unfamiliar equipment and logistics. It was hard going and stressful, especially in the first wave, when the operating room nurses found that redeployment decisions took little account of patient safety and the quality of care. This resulted in considerable workload stress, both psychologically and ethically: ‘What was said initially was that you shouldn’t have sole responsibility for the care of critically ill patients.’
Another recounted: ‘You’re supposed to manage people’s lives, with medications, and in terms of pain relief and blood pressure and pulse and everything else. I found that a bit uncomfortable, I didn’t have enough expertise to be there.’
The operating room nurses who were less well prepared for task shifting experienced moral stress and increased workload stress.
Discussion
The objective of the study was to explore how Norwegian health authorities utilised the professional expertise of operating room nurses during the first two waves of the COVID-19 pandemic. The redeployment of operating room nurses entailed task shifting. This task shifting generated knowledge and provided important information in the discussion about future task shifting in the health service in crisis situations.
Operating room nurses’ professional practice
Many operating room nurses were redeployed to basic nursing roles and ancillary functions, which is also described in another context (18). The professional expertise of the operating room nurses, particularly in infection control, could have been better utilised, both in the planning and implementation of hospitals’ practical infection prevention efforts.
The authorities self-evaluated their management of the COVID-19 pandemic (19). They emphasised the need for clarification regarding the health authorities’ obligation, under the Health and Social Preparedness Act, to have an overview of personnel who can be mobilised. They also stated that the health authorities should plan for escalation, de-escalation and redeployment during a crisis. This improved overview of employees’ competence could also benefit from the inclusion of professional practitioners’ specialist expertise, leading to a more efficient and effective task shifting process in times of crises.
Such an approach will also help to raise awareness of operating room nurses’ specialist expertise among other categories of employees in the health authorities. Good interprofessional collaboration leads to a higher quality of healthcare services (20, 21). It is also likely to improve the health authorities’ preparedness for the next crisis or pandemic preparedness and help to give professional practitioners more say and predictability.
Crisis management
A crisis is a major event that affects a large number of people, and management must steer the ship to achieve goals with the help of the employees (22). Given the discrepancies in task shifting encountered by operating room nurses following redeployment, we believe there is room for improvement in preparedness and management. This understanding is in line with the report by the COVID-19 Commission in 2021, which notes that the Norwegian government was not sufficiently prepared for the pandemic, despite it being a known risk (19).
A typical characteristic of a crisis is a lack of information, which creates uncertainty (22), as acknowledged by the operating room nurses. The redeployment process would have been more effective if the experience of individual nurses had been taken into account and more transparency had been shown. The operating room nurses also experienced a shortage of equipment, which caused considerable frustration. Previous reports indicate that resource management was challenging in the early stages of the pandemic. Many were faced with dilemmas when prioritising resources (3).
Psychological and ethical burden
The ethical dilemmas experienced by the operating room nurses were evident. Redeployment during the first waves of the COVID-19 pandemic has previously been described as morally stressful and psychologically burdensome for operating room nurses (23–25). Redeployment sometimes leads to healthcare personnel feeling uncertain about whether their professional efforts are sufficient to meet patients’ needs. This compromises patient safety, which in turn increases the risk of staff burnout (26).
Research has shown that nurses are more susceptible to contributing to adverse incidents and patient injuries when exposed to more demanding workloads and stress, and when their efforts are not properly recognised (27, 28).
A high standard of patient safety is part of good quality of care, a principle upheld by the operating room nurses and ingrained in professional practice and ethics. When the nurses felt that redeployment was a threat to patient safety, it was therefore burdensome for them. Conversations with our closest colleagues are perhaps the best type of support available in a crisis situation (29), where patient safety is considered compromised.
Although the operating room nurses demonstrated great community spirit during the pandemic, there is an obvious risk associated with stretching employees’ work morale and increasing their burden. The perceived threat of COVID-19 early in the pandemic has been shown to contribute to burnout among nurses (30). A higher incidence of burnout among healthcare workers during the pandemic was associated with heavier workloads, job stress, time pressure and limited organisational support (31).
A systematic literature review concluded that burnout related to the pandemic can be prevented by reducing workloads through adjusting shifts, reducing job-related stressors and creating a healthy working environment (32). Furthermore, the shortage of nurses as a result of the pandemic has been described as problematic (33, 34), compounding the existing problem of nursing shortages before the pandemic (35).
There is an extremely high demand for nursing competence in the specialist health service (36). Statistics Norway has reported that the shortage of nurses in Norway will intensify in the years ahead (37). A systematic review article points to solutions that can reduce the nursing shortage and thus improve patient safety and the quality of patient care (38).
Some of the solutions include improving staffing levels, optimising the working environment, supporting nurses in meeting the demands of patient care, improving work relationships, utilising new technology and innovations and putting in place strategies for better flexibility and work-life balance (38).
Strengths and limitations of the study
The study has several strengths. Firstly, we conducted interviews at four hospitals. Secondly, the interviews were carried out by specialist nurses with a good understanding of professional practice. Thirdly, the chosen method and timing of data collection were appropriate for gathering rich information on the topic. The operating room nurses were still in a pandemic situation with the prospect of further waves of infection, and there was therefore a reduced risk of bias due to poor memory.
However, as a possible limitation of the study, it cannot be entirely ruled out that the time between the experiences of the operating room nurses and the interviews introduced a bias in how they remembered these experiences. Furthermore, we cannot completely rule out the possibility that our preconceptions influenced the interpretations and that the lack of more contextual data could have yielded different results.
Conclusion
For the next major crisis situation, hospitals should have more detailed plans for utilising the specific professional competence of operating room nurses. Transparent and appropriate information and resource management will be crucial factors in giving operating room nurses more say in how they work.
In order to prevent burnout, task shifting must be organised in a way that has a positive impact on work-life balance. Moreover, it must not lead to a further shortage of key nursing competence or an increased risk of compromised patient safety.
Acknowledgements
We would like to thank Berit Taraldsen Valeberg, Professor in Anaesthesia Nursing, who conducted three of the interviews at one of the hospitals.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge










Comments