Nurses’ experiences with home nursing care teams – a qualitative study
Summary
Background: The home nursing service is currently facing major challenges. The combination of increasing care needs among service users, a broader range of patient groups and shorter hospital stays is putting greater demands on nurses’ expertise and the organisation of services. In recent years, various organisational models have been developed to optimise the use of nursing resources and expertise, as well as to improve the standard of care. One such model is the use of nursing teams in home nursing care. However, research is limited on the experiences of nurses who have worked in these teams.
Objective: To gain a deeper understanding of nurses’ experiences of working in a home nursing care team.
Method: The study employed a qualitative research design. We conducted semi-structured interviews with eight nurses who were working in nursing teams during the project period.
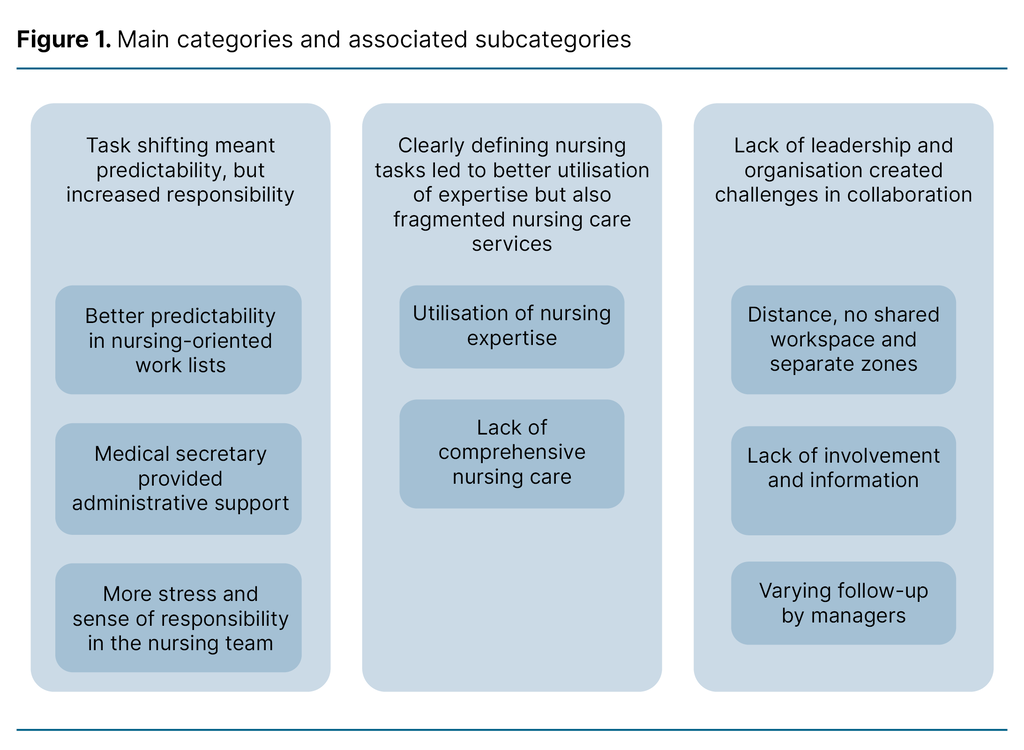
Results: Three main themes were identified: 1) Task shifting meant predictability, but increased responsibility, 2) Clearly defining nursing tasks led to better utilisation of expertise but also fragmented nursing care services, and 3) Lack of leadership and organisation created challenges in collaboration.
Conclusion: The nursing team model led to predictability in the allocation of tasks, but also an increased burden of responsibility for the nurses in the team. Nurses’ expertise was better utilised because tasks were more clearly defined. However, the task shifting also resulted in fragmented nursing care services. Patient contact and the nurses’ ability to provide comprehensive care were adversely affected. A lack of leadership and organisation also made collaboration more difficult.
Cite the article
Thorkildsen T, Karlsen C, Barken T. Nurses’ experiences with home nursing care teams – a qualitative study. Sykepleien Forskning. 2025;20(100995):e-100995. DOI: 10.4220/Sykepleienf.2025.100995en
Introduction
The home nursing service is currently facing major challenges. The combination of increasing care needs among service users, a broader range of patient groups and shorter hospital stays are putting greater demands on nurses’ expertise and the organisation of services (1, 2). The current organisational model in the home nursing service often requires service users to interact with many unfamiliar staff members (3).
Seven out of ten nurses in home nursing care report performing tasks that are not defined as nursing tasks on a daily basis (4, 5). Taken together, these findings suggest that nurses’ expertise is not being fully utilised, indicating the need for the service to find effective organisational solutions (6).
In recent years, a team-based organisational structure has been a focus area in the development of home nursing services (7–10). This organisational model focuses on expertise and resources and can help promote coordination and efficient organisation (7, 11).
In nursing teams, tasks for each patient are divided between staff members based on their expertise, and transferred from, for example, a registered nurse to a nursing associate (11, 12). Several municipalities have developed different organisational models in recent years to improve service quality, including health teams in Bergen and nursing teams in Tromsø (9, 10).
Objective of the study
This study focuses on the ‘Nursing Team’ project, which was initiated in 2020 in a municipality in southern Norway and concluded in the autumn of 2021. The study is based on experiences from the project period. Research is limited on the experiences of nurses working in home nursing care teams. The objective of this study was therefore to gain a deeper understanding of these experiences.
Method
The study employed a qualitative design with a phenomenological-hermeneutic approach. This approach was chosen to gain a deeper understanding of the participants’ subjective experiences (13). We used the COREQ checklist (14) to ensure the quality of the study's execution and reporting.
Organisation of nursing teams in the project
Home nursing services are organised into different geographical zones. The nursing team in this project consisted of nurses from two different zones working from the same premises. The nurses from the two zones worked together in the nursing team during the day and evening shifts. The nursing associates and assistants in each zone had two dedicated zone teams, with their own office, separate from the nursing team.
The nurses in the team mainly performed tasks that required the specific expertise of nurses, defined nursing tasks, such as complex wound care, medication dosing and administering antibiotics to patients at home. The zone teams carried out other types of tasks, such as personal care, showering and meal preparation.
Service users who required follow-up from both the nursing team, such as medication dosing, and the zone team, such as showering, would receive visits from both a nurse and a nursing associate or assistant at different times.
As part of the project, a shared medical secretary was also appointed to relieve the nurses of certain administrative tasks, including ordering medications and supplies, renewing prescriptions and dealing with certain messages from the electronic nurse messaging service. The nursing team also included two different department managers. After the project period ended, the two zones chose to return to the previous organisational structure. As a result, the nursing team was dissolved.
Recruitment and sample
To recruit participants, we emailed the two department managers responsible for the nursing team. They then shared information about the study with potential participants in the relevant zones. The inclusion criteria for the study were nurses employed in home nursing care who were part of the nursing team during the project period.
A total of seven women and one man, aged between 28 and 60 years, were included in the study. Experience in home nursing care ranged from two to twelve years.
Data collection
We collected the data in eight individual semi-structured interviews with the nurses who were part of the nursing team during the project period. Four participants from each of the two zones took part. The first author conducted the interviews.
The main themes in the interview guide focused on the nurses’ experiences of working in the nursing team, how things were before, the differences between working in the zone team and the nursing team, as well as the opportunities and challenges, and service user follow-up in the team.
The first author made voice recordings of the interviews and transcribed them. The interviews lasted an average of 30 minutes and were conducted a couple of months after the end of the project.
Analysis
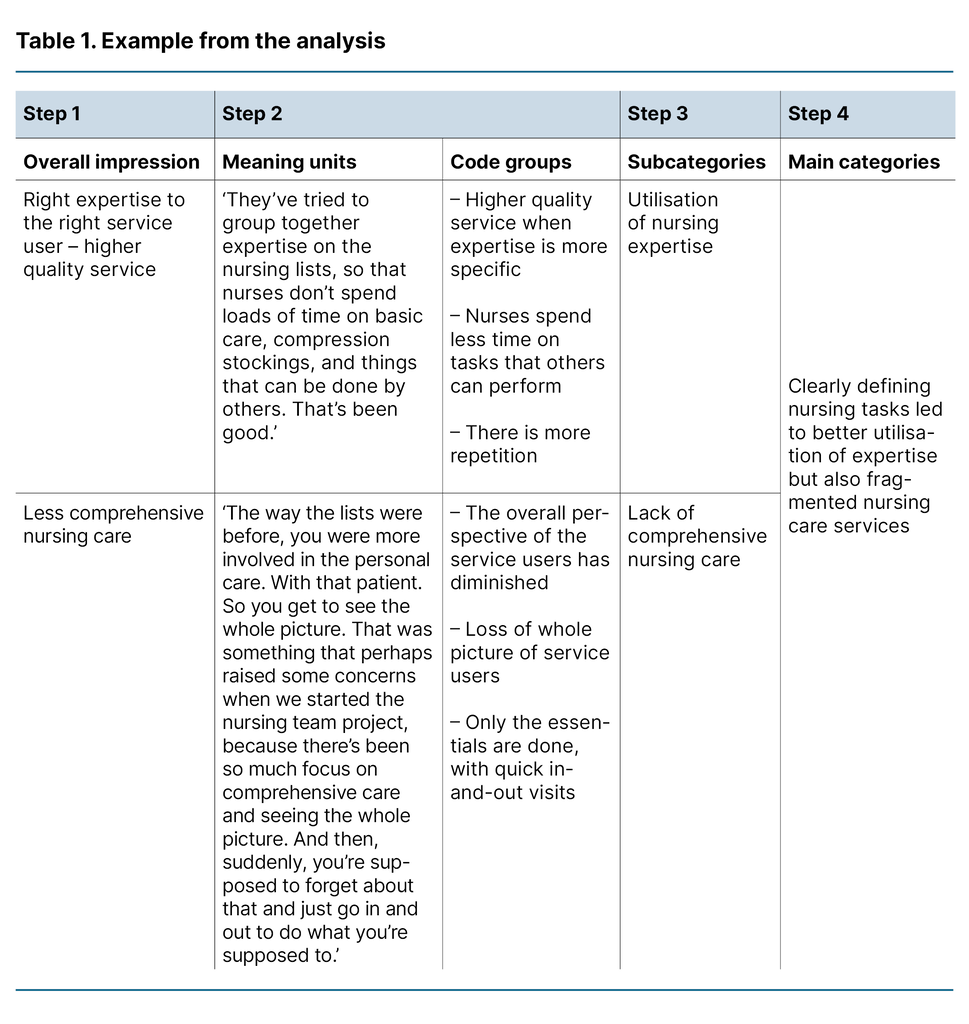
We analysed the interviews using systematic text condensation, inspired by Malterud (13). In the first step, we carefully read through the voice recording transcriptions to form an overall impression, and noted 13 preliminary themes.
In step two, we used the analysis tool NVivo to review all the interviews again and identified meaning units. We then sorted parts of the text that could illuminate the research question and then systematically categorised and coded the meaning units. In the final step, we created code groups.
In step three, we abstracted the content of the code groups, where twelve subcategories were formed. In the fourth step, the fragmented text pieces from the previous steps were condensed and recontextualised, and the subcategories were divided into three main categories.
Three main themes were identified in the analysis. Table 1 provides an example of the steps involved in the analysis.
Ethical considerations
The Norwegian Centre for Research Data (now called Sikt – the Norwegian Agency for Shared Services in Education and Research) was notified of the project (reference number 231545). We obtained written consent from the participants. They consented to the interview being recorded, and were assured that the data would be securely stored afterwards. We used fictional names, and place names are not specific. The study is in line with the recommendations of the Declaration of Helsinki (15).
Results
We identified three main themes: 1) Task shifting meant predictability, but increased responsibility, 2) Clearly defining nursing tasks led to better utilisation of expertise but also fragmented nursing care services, and 3) Lack of leadership and organisation created challenges in collaboration. Figure 1 illustrates the main categories and corresponding subcategories.
Task shifting meant predictability, but increased responsibility
Task shifting in the nursing team led to predictability in the daily work routine, but it also increased the nurses’ burden of responsibility. Task shifting entailed transferring tasks from nurses with more advanced expertise to other healthcare personnel within the zone team. This meant that several staff could be allocated tasks for each service user.
Delegating tasks that could be performed by other categories of personnel led to more nursing-oriented work lists. It also meant more predictability as the nursing team was assigned the same service users over several days.
Task shifting also involved appointing a medical secretary, which further increased predictability for the nurses and provided them with administrative support. The medical secretary relieved the nurses of certain administrative tasks and answered the on-call phone. As a result, the participants felt they could concentrate more on the service users and have fewer interruptions. One of the participants described it as follows:
‘I think it’s more professional when you have someone who answers the phone calmly and can quickly find things on the computer, instead of a nurse who’s in the middle of showering a patient. Who can listen. And then you might say: “Oh, I’ll need to call you back.” And then you forget to call them back when there are so many phone calls.’ (Participant 3)
Although task shifting meant more predictability for the nurses, many experienced a greater burden of responsibility and workload. Service users who needed nursing care were grouped into fewer work lists. As a result, the nurses in the nursing team were more isolated, with fewer opportunities to delegate nursing-related tasks. One informant said the following:
‘The work lists are more focused on nursing tasks now. It’s been more hectic. Fuller lists. And there are always so many extra messages. And things we have to do outside the list. New service users. It feels like there’s been more stress and it’s busier on the lists during that period.’ (Participant 2)
In addition to having to follow up the service users on their own work list, they also had to manage administrative tasks both in the nursing team and the zone team. This increased the burden of responsibility and created stressful working days.
Clearly defining nursing tasks led to better utilisation of expertise but also fragmented nursing care services
Many of the participants felt that the organisation of the nursing team led to better utilisation of their expertise, as they only performed defined nursing tasks. Participants also experienced more repetition as they were performing the same procedures frequently. This boosted their confidence in carrying out these tasks. Such repetition could improve both the quality and continuity of care. One informant illustrated this as follows:
‘I prefer working in the team. With more concentrated tasks, you learn more, get more repetition, more training. It brings more continuity. And the quality improves because you perform procedures more often. They’ve tried to group together expertise on the nursing lists, so that nurses don’t spend loads of time on basic care, compression stockings, and things that can be done by others. That’s been good.’ (Participant 1)
Although clearly defining nursing tasks led to better utilisation of expertise, it also made for a more fragmented nursing care service. One informant said the following:
‘The way the lists were before, you were more involved in the personal care. With that patient. So you get to see the whole picture. That was something that perhaps raised some concerns when we started the nursing team project, because there’s been so much focus on comprehensive care and seeing the whole picture. And then, suddenly, you’re supposed to forget about that and just go in and out to do what you’re supposed to.’ (Participant 5)
This fragmentation was particularly evident in the follow-up of service users with complex and extensive needs. The participants illustrated this by describing a situation from their working day: service users who needed help with both showering and medication administration received two separate visits instead of one – first from the zone team for help with showering, and then from the nursing team for help with medication. Consequently, visits to some service users by the nurses in the team were very short, leading to less comprehensive and less patient-centred nursing care.
Lack of leadership and organisation created challenges in collaboration
The participants described a lack of leadership and organisation of the nursing team. They reported a lack of preparations, routines and information prior to the launch of the project. Several felt that they were not sufficiently involved from the beginning, and as a result, the project did not gain strong support among the staff.
The participants also described varying follow-up by the department managers in the two zones. Management of the project differed, as did engagement and attitudes. This, in turn, impacted on the participants’ attitudes to the nursing team. Several participants expressed resistance to working in the nursing team and were critical of the change. One of them described it as follows:
‘I feel like I noticed quite a range of attitudes among people about working in a team. Some were really negative and felt it was a waste of time and a nonsense to be there.’ (Participant 8)
In addition to the participants experiencing a lack of preparation and leadership, there was also no provision for a shared workspace. Several of the participants would have liked a common medication room, zone office and collaboration on mutual patients. Each nursing team covered its own geographic area within the municipality, which resulted in long distances between the zone offices. One participant said the following:
‘Because that’s what I thought when we were selected for this project, that we were going to work across teams. But we’ve hardly done that at all. So I think we would have gotten much more out of it if we’d had a mixture of service users. And then I think collaboration would’ve been easier.’ (Participant 1)
Despite the introduction of the nursing team model, the original organisation of the zone offices was maintained. The nursing team only spent time together when giving a joint report before their shift started. The separation of the nursing team and the zone team meant that participants lost the sense of the overall picture and contact with their colleagues.
The two zones within the team also had no work lists with mutual service users, which led to the participants losing any sense of ownership and connection to the service users in the other zone. This affected the collaboration within the team.
Discussion
The objective of this study was to gain a deeper understanding of nurses’ experiences of working in a home nursing care team.
Task shifting meant predictability, but increased responsibility
The findings of the study show that task shifting in the nursing team led to greater predictability in the daily work. Tasks were transferred, for example, from registered nurses to nursing associates, and the work lists had a greater focus on nursing-related tasks. The correct allocation of tasks can help maintain and improve the quality of services, as well as increase employee efficiency and job satisfaction (7).
In this study, appointing a medical secretary helped relieve nurses of administrative tasks. In healthcare organisations, administrative work is often invisible, despite its significant impact on the quality of services (16). Shortages of administrative personnel can lead to heavier workloads (17).
Our study shows that task shifting also led to an increased burden of responsibility due to fewer work lists and nursing-related tasks that could not be delegated. In addition, the nurses worked more independently. Consequently, participants had a more stressful working day.
According to Gjevjon (12), the allocation of responsibilities and tasks must be deliberate and structured. If healthcare personnel who are assigned new tasks lack the necessary expertise, they are likely to feel uncertain and experience a greater burden of responsibility. Their job satisfaction may also be diminished.
Research shows that successful task shifting requires close collaboration between all team members. Additionally, patient care must be coordinated and based on patient needs. Those involved should be given more decision-making powers, along with training and more support. An effective organisational system is also essential (18).
Clearly defining nursing tasks led to better utilisation of expertise but also fragmented nursing care services
Findings from the study show that clearly defining nursing tasks led to better utilisation of expertise, which in turn provided a stronger foundation for quality and continuity in the delivery of nursing care. Effective use of nursing expertise leads to a better provision for service users and a higher level of job satisfaction for staff (19). Having clearly defined nursing tasks can also help ensure better primary care for seriously ill patients discharged from the specialist health service (14).
However, Melby et al. (20) point out that utilising nursing expertise can also present challenges. If nurses are only assigned nursing tasks, it can reduce their contact with patients (20). Our study supports this finding.
In the nursing team, care was primarily guided by staff’s expertise rather than need. As a result, the nursing care service became more fragmented, which can challenge the ideal of comprehensive nursing (21). One example was when service users with complex needs received help from both the zone team and the nursing team. This required them to interact with many different healthcare personnel, which could be considered a lack of continuity in care providers. This can impact on service users’ dignity, sense of security and patient safety (3).
In addition, nurses may miss important observations (20). Assisting someone with personal care involves much more than just performing a practical task – it includes relationship-building, assessing needs and observing the person’s condition (22). It is important to critically reflect on this kind of task-oriented approach, as seen in the nursing team, and to acknowledge the complexity and comprehensive responsibility inherent in nursing (12).
Lack of leadership and organisation created challenges in collaboration
The study shows that the two zones within the nursing team had problems collaborating with each other, partly due to a lack of organisation. Optimal teamwork and successful collaboration are dependent on several essential factors. The team must share a common vision and have the same goals for patient care (23).
When staff in a team work in isolation, without collaborating, they are less likely to achieve shared goals (24). Problems are more easily solved when the team shares responsibility. Collaboration across different parts of the team makes it more likely that shared goals will be reached (24).
The attitudes and level of engagement of managers impacted on the participants’ approach to the project in our study. Leadership plays an important role for nurses working together in a team (25), and a lack of interest in or willingness to commit to change can act as a barrier to successful implementation (26). Employees can be influenced by the attitudes of others, which can shape their own approach to the change (27).
The participants in our study also reported a lack of information and said they were not very involved in the initial phase of the project. Successful organisational change requires sufficient information for, and support from, employees. Furthermore, staff must be involved at project start-up (25, 28). According to Robinson et al. (27), active involvement can also give employees a better understanding of the change initiative.
This study contributes to the understanding of how the home nursing service can organise nursing teams, but also shows that several factors may have contributed to the project being discontinued. For a nursing team to function effectively in practice, the following prerequisites should be in place: raising awareness of and clearly defining the division of responsibilities and tasks for both staff and management in the home nursing service, as well as ensuring comprehensive care by utilising nursing expertise to meet the needs of service users.
To strengthen collaboration within a nursing team, appropriate organisation is essential. Additionally, management must actively involve employees and ensure they support the project.
Strengths and limitations of the study
The authors are nurses with master’s and doctoral degrees. We have experience from hospitals and the home nursing service, but currently work as nursing instructors at a university. The first author has previous experience from working in a nursing team. We have reflected on our own role as former nurses in all stages of the research process and included reflective elements as part of the research method.
A strength of the study is that the sample included a varied range of ages and experiences. However, there was only one male participant in the study. We believe that the interviews provided rich material with diverse experiences and perspectives.
Despite the small sample, data saturation was achieved. Although sample size can affect the transferability of the study, we believe the results may be transferable to similar contexts.
A limitation of the study may be that the interviews were conducted during a transition phase, when participants were shifting back to the original organisational structure after having worked together as part of a nursing team. Many of the nurses thus said it had been some time since they had worked according to the project’s methods.
Conclusion
This study provides a better understanding of nurses’ experiences with home nursing care teams. The nursing team model entailed a predictable allocation of tasks but also resulted in a greater burden of responsibility for the nurses in the team. With clearly defined nursing tasks, expertise was better utilised, but this led to fragmented nursing care services. As a result, patient contact and the nurses’ ability to provide comprehensive care were adversely affected.
Additionally, collaboration within the team was hindered by a lack of leadership and organisation. Further research on this topic is needed to elicit additional perspectives, including those of managers, nursing associates, and service users and their families.
Acknowledgements
We would like to thank the participants in the study for their time and for sharing their experiences with us.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge


Comments