Nurses’ parent contact in the low-threshold services – a cross-sectional study
Summary
Background: Nurses play an important role in child and adolescent mental health work in low-threshold services in primary care. National guidelines and manuals encourage family-centred work. Parental involvement and family-centred care are considered to be evidence-based knowledge within health services for children and adolescents.
Objective: To investigate the extent of nurses’ parent contact in low-threshold services. We wished to explore which factors related to the nurses and services are associated with parent contact.
Method: The study is based on questionnaire data from a cross-sectional study conducted by the Regional Centre for Child and Adolescent Mental Health, Eastern and Southern Norway (RBUP). The sample consisted of 243 nurses working in low-threshold services in primary care for children and adolescents. The data were analysed using chi-square tests and ordinal regression analysis.
Results: The results show that the type and frequency of parent contact varies. Telephone contact was the most frequent way to involve parents, and 94 per cent of the nurses in the study reported that they occasionally, often or always had telephone parent contact. Just over 63 per cent reported that they occasionally, often or always saw parents and children together at appointments. Around 30 per cent of the participants reported that they either never or seldom saw parents and children together at appointments, or only worked with parents. The results also show that education, training in manual-based parental counselling tools, wishing to have more time for the child in their work, and being part of the Familiens hus (Family’s House) group of services were associated with frequent parent contact. Working in the school health service and working solely with adolescents was associated with less frequent parent contact.
Conclusion: The results indicate that competence enhancement, clearer frameworks for the services and local guidelines for family involvement may be important priority areas in the future efforts. The need for more research on the low-threshold services’ work with families can be met through larger-scale representative studies. The same applies to studies exploring the experiences of children and adolescents, families and nurses with family involvement.
Cite the article
Steinskog T, Bjørseth Å, Lydersen S, Helland S. Nurses’ parent contact in the low-threshold services – a cross-sectional study. Sykepleien Forskning. 2024;19(96298):e-96298. DOI: 10.4220/Sykepleienf.2024.96298en
Introduction
Mental health problems in children and adolescents are one of the most significant public health challenges faced by Norwegian local authorities (1). The primary care services play a key role in health-promoting and preventive work, and also have a responsibility in the treatment of mental health problems in this population (2). However, there are considerable variations in the type of treatment provision in primary care (2), even though increased pressure on the specialist health service means that more individuals with moderate and severe mental disorders are dealt with in the low-threshold services in primary care (3 ).
Nurses play an important role in helping children and their families (4), both in various low-threshold teams for mental health and in statutory services such as child health centres and the school health service (2). Nurses in Norway report that they spend more than half of their time on tasks related to mental health (5). In addition to the follow-up offered by the school health service for children with mental health issues and disorders, the national clinical guidelines encourage practitioners to consider whether parents should also be informed and included (6).
The importance of family involvement in health services for children and adolescents is widely supported by research (7) and is emphasised in several national guidelines and manuals (1, 8). The child welfare reform in Norway of 1 January 2022 makes it mandatory for the municipal services to work preventively with families and the child’s environment (9), both because proper support from parents can protect the child from developing mental health issues (10), and because neglect is a risk factor for developing physical and mental disorders (11).
Sameroff’s transactional model illustrates how children and parents mutually shape each other over time, and how negative development in the child can be reversed by helping parents change their interpretation of or behaviour towards their child (12). Parents may therefore play an important role as participants in their child’s treatment (13). Moreover, for many parents, their involvement is important for their own health and sense of coping (14).
Within the nursing profession, it appears that attention has moved increasingly from individually centred to family-centred nursing. Several studies point to the advantages of family-centred care (FCC), where the entire family is regarded as recipients of treatment and care (7). Nurses have a generally positive attitude to involving the family (15), but most studies have been conducted among hospital nurses (15).
The few studies that have been conducted in low-threshold services (16–20) show that for nurses in the school health service, most parent contact takes place in telephone conversations (16), and that the contact is mainly problem-based and deals with risk factors for the child’s health or well-being (20).
In Norway, family-centred care has been studied in mental health services for adults (21, 22), but has received little attention in the services for children and adolescents. In studies investigating the work of the Norwegian school health service with mental health issues, however, public health nurses express the importance of involving the family and strengthening the role of parents (5, 23).
Despite positive attitudes to family involvement, there are still challenges in implementing family-centred care in practice (24). Implementation of new knowledge is a frequently studied topic (25), and several theoretical models and frameworks have attempted to describe what characterises successful implementation processes (24).
The ‘Knowledge-to-Action’ framework (26) illustrates the importance of closeness between the field of research and the users. It shows how knowledge should be tailored to users’ needs and barriers identified in the context in which the new knowledge is to be implemented (26). For routines and tools for family involvement to function well in the low-threshold services, it may therefore be important to know what characterises the services’ work with families.
The purpose of this study is therefore to answer the following research question:
‘What is the extent of nurses’ parent contact in low-threshold services for children and adolescents, and which factors related to the nurses and services are associated with parent contact?’
Method
This cross-sectional study is based on data from a questionnaire survey undertaken by the Regional Centre for Child and Adolescent Mental Health, Eastern and Southern Norway (RBUP) in 2019 (27). The aim of the survey was to identify the mental health services available for children and adolescents in primary care.
The target group was municipal employees who offer mental health care for children and adolescents between 5 and 18 years of age, with no requirement for referral, that are easy to access, and that are primarily intended for children with mild and moderate mental health issues. The data were collected via an online questionnaire (Appendix 1 – in Norwegian only) that was sent out in spring 2019. The questionnaire survey was assessed by the Norwegian Centre for Research Data (NSD), now called Sikt – the Norwegian Agency for Shared Services in Education and Research, as being compliant with data protection legislation, reference number 331014.
Sample
We recruited participants for the survey by emailing 1270 municipal employees in low-threshold mental health services in all Norwegian counties. One reminder was sent, and we encouraged recipients to forward the email to other relevant respondents. Participants were also recruited via RBUP’s website, RBUP’s Facebook page and the website of the Norwegian Resource Centre for Community Mental Health (NAPHA).
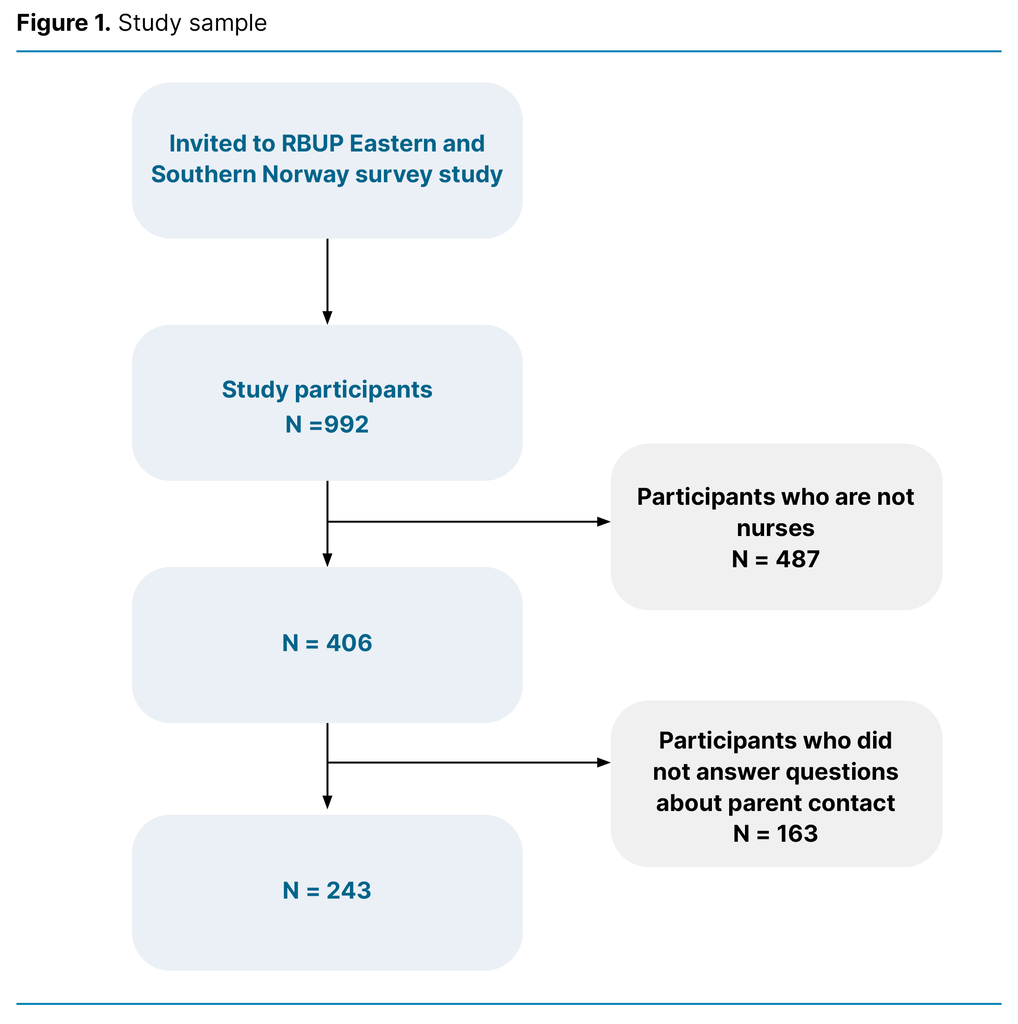
The data collection took place from 21 February 2019 to 21 May 2019. To date, one article has been published from the data material, which relates to the psychologists in the survey (27). Of the 992 respondents in the survey, 406 had a nursing background. Of these, 243 (59.9 per cent) responded to the questions about parent contact (Figure 1). These nurses comprise the sample in this study.
Variables
To investigate parent contact, we posed the following questions: ‘ attend the appointments together with the child?’ and ‘How often do you work solely with parents/guardians?’. The variable is a five-category variable, and the response alternatives were ‘never’, ‘seldom’, ‘occasionally’, ‘often’ and ‘always’.
The participants were asked about gender, age, number of years of relevant professional experience and whether they had specialist education or postgraduate education. The education variable was dichotomised to ‘education beyond a three-year bachelor’s degree’ (‘yes’/’no’).
The participants were asked whether they had training in 16 different manual-based tools that are often used in mental health work with children and adolescents. Of these, nine are considered to be parental counselling tools: De utrolige årene [The incredible years], Tuning into kids, Tuning into teens, Circle of Security, International Child Development Programme (ICDP), Multisystemic therapy, Parent Management Training Oregon (PMTO/TIBIR), Treatment Foster Care Oregon (TFCO) and Functional Family Therapy (FFT).
They also had the opportunity to add any other manual-based tools. The variable was dichotomised to ‘have training in parental counselling tools’ (‘yes’/‘no’).
The participants were asked which service they worked in. The variable was dichotomised to ‘works in the school health service’ (‘yes’/‘no’). They were also asked ‘Which of these groups is the service you work in primarily aimed at?’ and were asked to select one or more of the alternatives ‘infants and young children (0–4 years)’, ‘children (5–12 years)’ and ‘adolescents(13–18 years)’. The variable was dichotomised to ‘work solely with adolescents’ (‘yes’/‘no’).
To map time resources, the participants where asked ‘how often would you like to have had more time/more sessions with the child and/or the family?’. The variable was dichotomised to ‘yes’ (‘often’ and ‘very often’) and ‘no’ (‘very seldom’, ‘seldom’ and ‘occasionally’).
The participants were asked whether the service they work for is part of a family centre or the Family’s House, a service model used by several municipalities to coordinate services for children, adolescents and families. The variable was dichotomised to ‘yes’ (‘yes’) and ‘no’ (‘no’ and ‘don’t know’).
Analysis
Results from descriptive statistics are reported as mean and standard deviation and in absolute and relative numbers. To investigate the associations between different variables and parent contact, we used the chi-square test and ordinal logistic regression analysis with parent contact as the five-category dependent variable.
By using ordinal logistic regression with a five-category dependent variable, we utilised the information available in the data, rather than dichotomising the variable and using normal (binary) logistic regression. The odds ratio in ordinal logistic regression has the same interpretation as in binary logistic regression (28). A two-tailed p-value less than or equal to 0.05 is considered to indicate statistically significant findings. We analysed the data in SPSS version 28.
Results
Description of the sample
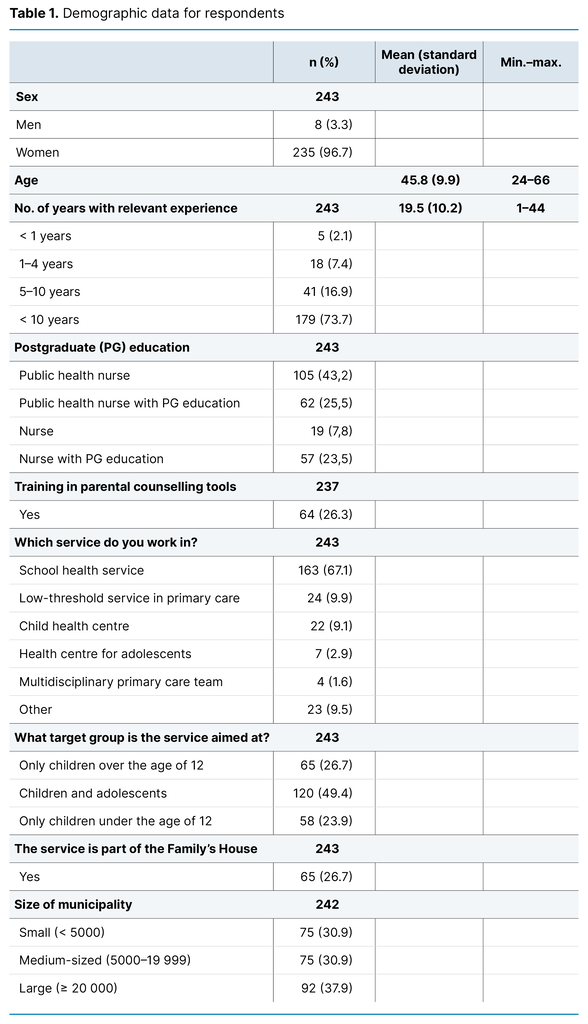
Table 1 shows demographic data for the respondents. When we compared those who completed the survey with those who did not complete the full survey, we found more participants who worked solely with adolescents and in the school health service among those who completed it (Appendix 2 – in Norwegian only).
The extent of nurses’ parent contact
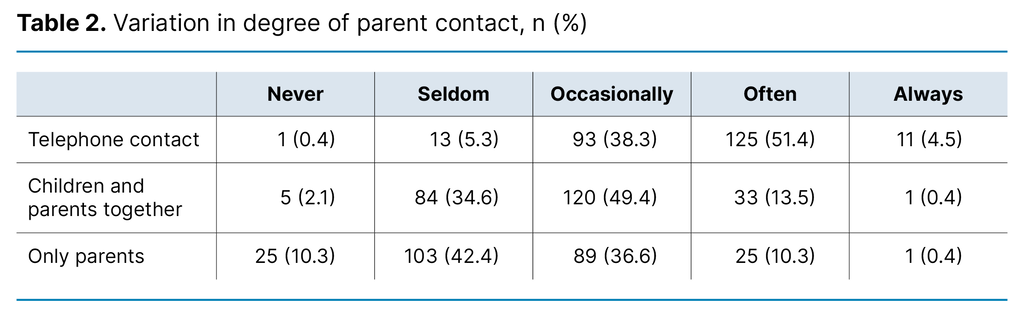
The results shown in Table 2 show variation in the extent of parent contact. Telephone contact was the most frequently used way to involve parents, and 94 per cent of the nurses in the study reported that they occasionally, often or always had telephone parent contact. Just over 63 per cent reported that they occasionally, often or always saw parents and children together at appointments. Around 30 per cent of the participants reported that they never or seldom saw parents and children together at appointments, or that they only worked with parents.
Factors associated with parent contact
Factors associated with nurses’ parent contact
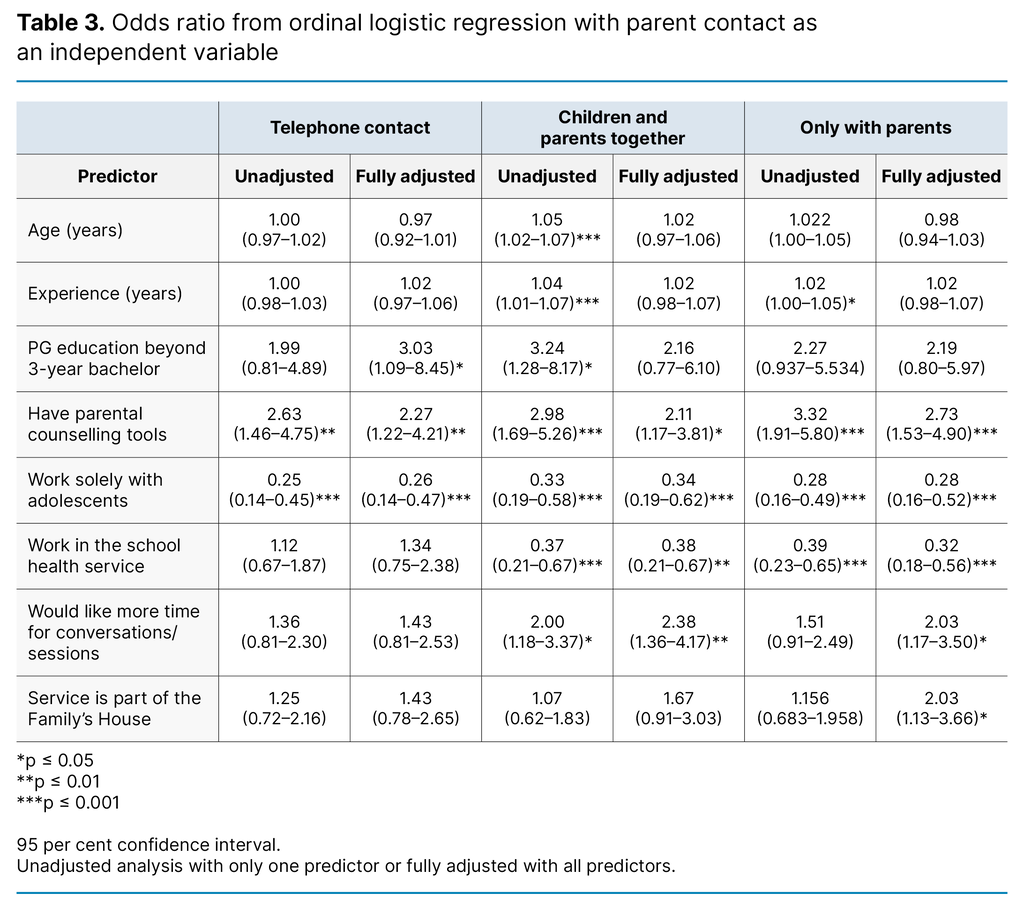
The results in Table 3 show that the likelihood of nurses reporting that they see parents and children together at appointments increased with the nurse’s age, experience and postgraduate education, but education was only statistically significant with regard to telephone contact in the adjusted analysis.
The nurses’ training in parental counselling tools is the factor that appeared to be most strongly associated with parent contact. The nurses with training in such tools were more than twice as likely as other nurses to report that they often had parent contact.
Factors associated with parent contact in the services
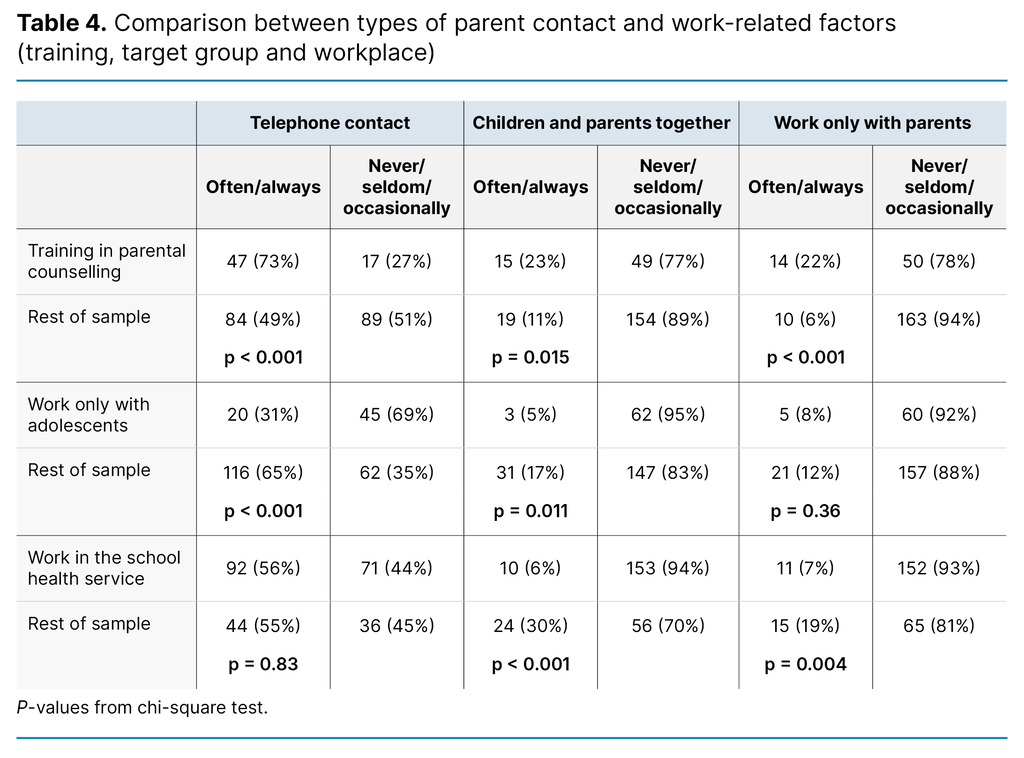
The results show that nurses who worked solely with adolescents reported having parent contact to a far smaller extent than the rest of the sample (Tables 3 and 4).
The nurses who worked in the school health service reported having parents present in appointments less frequently, either with or without the children (Table 3 and 4).
The percentage who reported that they frequently had parents and children attend appointments together, was five times higher in the rest of the sample than for the nurses who worked in the school health service (Table 4). We did not find large differences in the other variables between nurses in the school health service and the other services (Appendix 2 – in Norwegian only).
The nurses who wished for more time or more sessions with the children and/or their families reported having parents at appointments more often than the rest of the sample (Table 3).
Discussion
The objective of the study was to examine the extent to which nurses in low-threshold services have parent contact and which factors impact on this contact. Overall, the results show that the type and frequency of parent contact varied. Over 94 per cent of nurses had telephone contact and over 63 per cent had parents present in sessions. This is much higher than a US study in which 77 per cent of nurses had parent contact by telephone and only 18 per cent had parents present at in-person appointments.
The relatively high degree of parent contact may be due to the increased focus on mental health and family-centred work in recent years. (1, 8).
Despite nurses’ positive attitudes to family involvement, a third of the nurses in low-threshold services reported that parents were seldom or never present in conversations, either with or without the child. This suggests that there may be differing practices for how and to what extent parents are involved, both among nurses and across services.
Training in manual-based tools
The data in this study do not give an indication of whether the nurses are engaged in supportive or therapeutic work. However, the factor most strongly associated with parent contact among the nurses was training in manual-based parental counselling tools.
This finding aligns with other studies that have shown that training in family-centred methods fosters positive attitudes to family involvement (15), and that public health nurses are more likely to contact parents and invite them to family sessions after receiving training in family-centred conversation tools (29).
Since nurses are more likely to carry out the parts of family-centred care they consider necessary (30), knowledge about the benefits of family involvement may also be important. Criticism has been levelled at nursing education in Norway for lacking a family perspective (31).
Given that only 26 per cent of nurses in low-threshold services reported having training in parental counselling tools, there appears to be a need to raise competence levels in family-centred work. Training in manual-based tools could potentially bolster competence (29). Consideration should also be given at a national level as to how nursing education in Norway can help enhance competence and increase the number of tools used in family-centred care.
The largest portion of nurses in our sample had a public health nursing education or other additional training, which it is assumed will impact on their work. Education and experience, however, did not show such a clear association with parent contact. This finding is somewhat surprising, since several other studies found that higher education can lead to increased confidence and better skills in family care (19). Studies also show that less experienced nurses express uncertainty about family involvement (18, 19).
However, some studies have found no association between education and experience and positive attitudes to family involvement (17). It is conceivable that factors such as training in parental counselling tools or type of postgraduate education may have impacted on the results. Public health nurses have expressed a lack of tools when dealing with children with mental health issues (5, 17, 20), which has been found to be associated with a greater tendency to view the family as a burden (17).
Thus, competence in mental health may also impact on the frequency of nurses’ parent contact. Supervision for the least experienced nurses could be useful for promoting family-centred work, while more knowledge is needed about what aspects of education and experience affect the degree of family involvement.
Less contact with parents of adolescents
The study found several factors in the services to be associated with parent contact. Nurses working with children had more parent contact than those who work solely with adolescents, which is consistent with previous research (17). This may be because, under Norwegian law, children over the age of 12 have the right to influence what information is given to their parents (5, 32).
Public health nurses have expressed fears that conversations with parents may damage the relationship of trust with the child, leading them to prioritise the child’s wishes for confidentiality (20). Many parental counselling tools are also aimed at younger children, which can make nurses unsure about counselling parents of adolescents. More research is needed on the factors that impact on the degree of parental contact in adolescent health care.
The results show that parents are much less frequently present in conversations with nurses in the school health service than nurses in other low-threshold services, and those working as part of the Family’s House have conversations solely with parents more often. Differing frameworks and guidelines may partly explain this gap, and other studies have confirmed this to be an important factor (15, 25).
According to national guidelines, the main focus of the school health service is preventive and health-promoting work (6). Some local authorities have indicated that they involve family centres in cases requiring more follow-up (2). The advice in national guidelines for the school health service to involve parents can be perceived as weak (6). Users, primary care services and the specialist health service have all expressed a lack of clear directives or frameworks describing what can be expected from mental health services for children and adolescents in primary care (2). Different cultures of family involvement may also partly explain the difference in parent contact between the school health service and other services (15, 25). For instance, schools may be perceived as more of ‘the child’s space’, whereby children more often contact services without their parents’ involvement (33).
Based on our data, we cannot form a conclusion as to why public health nurses choose to include parents often or seldom. Moreover, the reasons children seek out the public health nurse in the school health service vary. Contact with children may consist of either a single conversation or multiple sessions. In cases related to friendships or matters of the heart, it may not always be appropriate or necessary to involve the parents. However, it is worth noting that healthcare personnel in different services involve parents to varying degrees, even though they have similar professional backgrounds and are supposed to follow the same national guidelines for working with patients’ families (8).
The results may indicate a need for local routines and procedures for family-centred work. This also applies when considering whether the frameworks under which the low-threshold services operate are aligned with national guidelines and strategies for working with patients’ families.
Time as a factor in family-centred work
Lastly, the study results suggest that nurses who expressed a desire for more time with children or families more frequently reported involving parents in in-person conversations. Lack of time is highlighted as a significant barrier to implementation (24, 25), and it is possible that the nurses who express a desire for more time are those who already spend extra time on conversations with parents. This is merely an assumption, as the reason why these nurses feel they have too little time is unknown.
Some nurses have expressed that family work is more time-consuming than individual follow-up (22), while others stated that family intervention is a time-saving and efficient way to gain an overview and provide help (28). These findings may indicate differences in how families are involved.
The results may also suggest that nurses have different perceptions of how much time family involvement requires. More studies are therefore needed to examine experiences with different family interventions. Since Norwegian public health nurses signal that they have a heavy workload (5), it is crucial to consider that time is an important resource that must be prioritised.
The associated factors we found in the study align with several aspects that implementation research identifies as facilitators or barriers (24). The ‘Knowledge-to-Action’ framework emphasises the importance of tailoring knowledge tools and interventions to local conditions and identified barriers (26). It is therefore important that management and staff in the various services understand the prerequisites for evidence-based care (26).
The fact that several service-related factors are associated with parent contact strengthens the argument that changes are also needed within each service and organisation for new knowledge to be implemented (24). Family-centred work should not only be anchored in national guidelines but also in the various service frameworks, local procedures and working methods (15, 25).
For knowledge development to meet users’ needs and contexts, it is also important that priority is given at a national level to knowledge development within low-threshold services. The planned initiative to establish a national centre of excellence for child health centres and the school health service can be an important step in this direction (34).
Methodology considerations
The larger sample size compared to similar previous studies was a strength of the study (16–19). However, cross-sectional studies cannot provide causal explanations between variables. Neither does the study elucidate the content of parent contact, whether practical information was involved, health assessments or guidance, or whether the content differed between telephone and in-person conversations.
A possible bias in the sample could be that participants were not randomly selected and that those who responded to the surveys might have been those who were most interested in the topic. The use of non-validated questions may be a weakness, as it is possible that the questions may have been misinterpreted. Using more objective quantifiers and response categories based on frequencies could have provided more valid data (35).
It is also possible that responses from school health service staff were based on all children who use the service, not just those with mental health issues.
Conclusion
The study shows variation in how and to what extent nurses in low-threshold services have parent contact. Factors related to both the nurses and the services are associated with the frequency of nurses’ parent contact. The findings suggest a need for more knowledge and tools in family-centred work, as well as clearer frameworks for services and local routines for family involvement.
An important step going forward could be to consider the content of nursing education and develop the national research community for low-threshold services. Knowledge about and tools for family involvement must be tailored to the needs and conditions of low-threshold services in order to strengthen family-centred work aimed at children and adolescents in primary care.
More studies are needed with larger, representative samples to explore how the various low-threshold services work with parents and families. Qualitative studies exploring nurses’ experiences with what hinders and promotes parental involvement are also needed, as is knowledge about the experiences of children, adolescents and parents with family involvement.
There is a further need for intervention studies examining how various family-centred interventions can aid nurses in their work with children and adolescents. The overarching goal should be for the child’s and family’s situation to guide decisions about when to involve parents, rather than factors related to individual nurses or services.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge


Comments