Initial nursing care for neonatal hypoxic-ischaemic encephalopathy – a systematic review
Summary
Background: Hypoxic-ischaemic encephalopathy (HIE) is a serious birth complication that occurs in approximately 1 in every 1000 births in Norway. Many of the infants who are affected are born in delivery rooms or hospitals with no therapeutic hypothermia facilities. These infants must be stabilised before being transferred to a regional therapeutic hypothermia unit for further treatment. Neuroprotective care in this stabilisation phase, including from a nursing perspective, is an under-researched area.
Objective: To collect and summarise knowledge for use in specialised training for nurses working in delivery rooms or hospitals with no therapeutic hypothermia facilities.
Method: Systematic literature review and reporting in PRISMA. Literature searches were conducted in the Medline, Embase and CINAHL databases. We performed a thematic analysis of quantitative studies, and the results are presented in a narrative form.
Results: Out of 1863 titles identified, we excluded 1859. One study was identified outside the systematic search, resulting in the inclusion of five cohort studies involving a total of 797 neonates with moderate to severe HIE. In the analysis, we identified the following themes: ‘Specialised neuroprotective care based on knowledge and clinical competence’, ‘Nurses play a key role in adhering to protocols, guidelines and documentation’, and ‘Nurses’ role in initiating passive cooling’. Specialised training for nurses needs to focus on early identification, stabilisation and transferral, which can contribute to reduced mortality, fewer seizures and shorter hospital stays. The nurse has a specific role to play in relation to documentation and must ensure adherence to guidelines for the assessment and selection of neonates for therapeutic hypothermia.
Conclusion: Nurses who work with neonates should receive specialised training and possess clinical competence in the early identification, stabilisation and transfer of at-risk patients to tertiary care. Adhering to guidelines and documenting assessments are crucial for identifying neonates who meet the criteria for therapeutic hypothermia. The literature review indicates that nurses play a key and active role in the treatment team. It also shows that specialised training can improve patient care standards and outcomes.
Cite the article
Holtmoen H, Aagaard H, Solevåg A. Initial nursing care for neonatal hypoxic-ischaemic encephalopathy – a systematic review. Sykepleien Forskning. 2023;18(94179):e-94179. DOI: 10.4220/Sykepleienf.2023.94179en
Introduction
Approximately 55,000 children are born in Norway every year (1). Moderate to severe perinatal asphyxia occurs in about 1 in every 1000 births, which is around 55 children annually (2). Perinatal asphyxia is a condition characterised by oxygen deprivation before, during and/or after birth. The condition can cause hypoxic-ischaemic encephalopathy (HIE), which is one of the most serious birth complications in neonates (3). According to Sarnat and Sarnat, HIE is classified as mild, moderate or severe based on systematic neurological examinations (4).
In a broader sense, asphyxia is defined as inadequate tissue perfusion, known as ischemia, where the body’s oxygen supply and the need to eliminate waste products are inadequate. Severe perinatal asphyxia has an adverse effect on the perinatal transition: from life inside the womb to life outside. Ischemia in vital organs such as the brain, kidneys and digestive organs can lead to further damage (5).
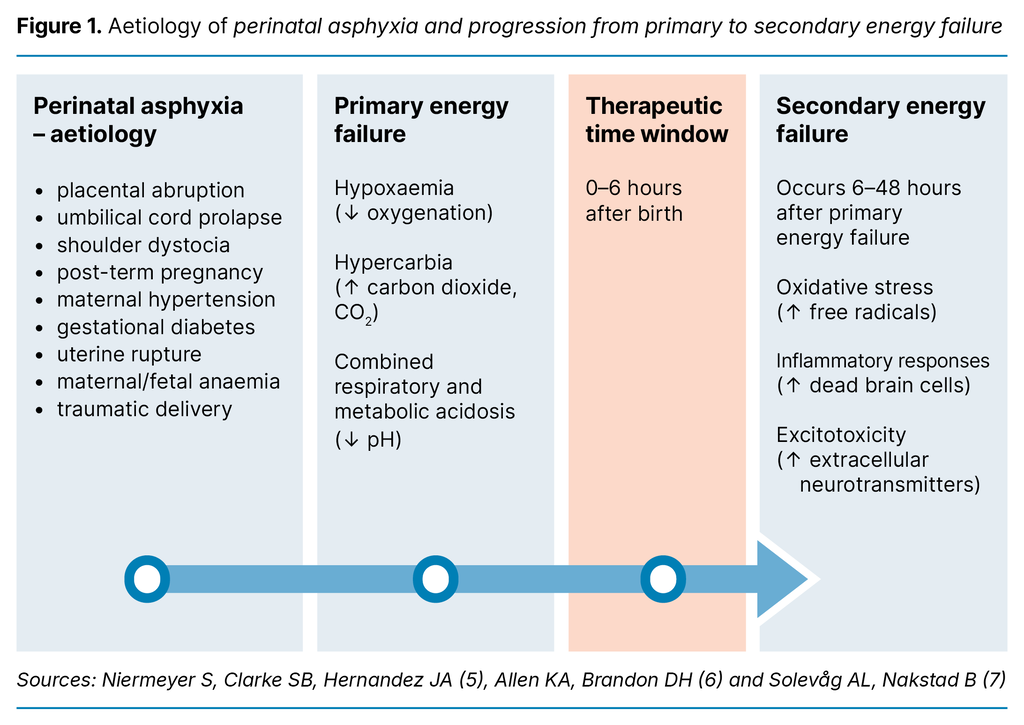
There are many different reasons why perinatal asphyxia affects neonates (7). Aetiology and injury mechanisms of perinatal asphyxia are described in Figure 1. Perinatal asphyxia leads to primary energy failure, with progressive hypoxaemia (decreased oxygenation), hypercarbia (increasing carbon dioxide, CO2) and a combined respiratory and metabolic acidosis (decreased pH). Oxygen-deficient tissue shifts from aerobic metabolism to a significantly less efficient anaerobic metabolism, contributing to energy failure and lactate production (5–7).
This acute phase leads to reduced production of adenosine triphosphate (ATP). ATP is required for many cellular functions, including maintaining the Na+/K+ pump and intracellular calcium. Failure of the Na+/K+ pump can lead to an imbalance at the cellular level, which can result in cerebral oedema due to swelling brain cells, as well as cellular necrosis and apoptosis (programmed cell death) (6).
Stabilising the neonate ensures reoxygenation and reperfusion, and temporarily restores cellular functions. This period, lasting up to six hours, is called the therapeutic time window, during which neuroprotective agents can limit the damage that occurs in the subsequent injury phase, caused by secondary energy failure (Figure 1) (6).
Therapeutic hypothermia (TH), with a core temperature of 33–34°C for 72 hours, is currently the only treatment that reduces mortality and brain injury in neonates with moderate to severe HIE. For optimal results, TH should be initiated as early as possible, preferably within six hours after birth (8).
The decision to perform TH is based on whether the neonate meets the so-called A, B and C criteria. ‘A’ criteria include Apgar scores, the need for positive pressure ventilation and acid-base values; ‘B’ criteria involve clinical encephalopathy assessment; and ‘C’ criteria include electroencephalography (EEG) (8). TH improves outcomes in neonates with gestational age ≥ 36 + 0 weeks and above with moderate to severe HIE. However, many infants still die or experience severe disabilities after undergoing TH (3, 6, 9).
In Norway, TH was introduced in 2007 as a treatment option for neonates with moderate to severe HIE (2). The treatment is advanced and resource-intensive, and only a few regional therapeutic hypothermia units therefore provide TH in Norway (2). In comparison, there are 45 maternity units and 20 neonatal intensive care units. Consequently, many neonates with HIE need to be transferred from the birthing unit to a regional therapeutic hypothermia unit (10, 11).
TH and other medical interventions for HIE are covered in Norway’s neonatal guidelines (8), but there is no mention of neuroprotective nursing care for this patient group. Recent studies (12, 13) have focused on specialised neuroprotective care for neonates with a recognised risk or who are at risk of brain injury. Specialised neuroprotective care involves assessment, monitoring and protection, including positive touch and pain and stress minimisation. Parents should also be present (12).
Glass et al. (14) propose a systematic approach, where the focus is on neurology and optimised care and treatment for, inter alia, neonates with HIE. Nurses play a crucial role in identifying early clinical signs and symptoms in at-risk patients (14). Three of the studies considered (12–14) concluded that more competence and research are needed in how specialised care for neurological conditions can improve at-risk neonates’ neurocognitive development.
Despite the abundance of medical research and literature on neuroprotective treatment, there is a lack of literature reviews viewed from a nursing perspective. The initial stabilisation of neonates with HIE before TH is also inadequately described. Collecting and summarising knowledge about the nurse’s role from medical literature can strengthen the treatment team function and help standardise and improve the patient care pathway.
Objective of the study
The purpose of this systematic literature review was to compile knowledge that can be used in the specialised training of nurses in delivery rooms and hospitals that do not provide TH.
The research questions are as follows:
- What knowledge and clinical competence do nurses need to provide neuroprotective care for neonates with HIE during the stabilisation phase up to the point of transferral?
- What is the nurse’s role in the treatment team during the stabilisation phase with continuous monitoring, clinical assessment and treatment up to the point of transferral?
Method
We conducted a literature review using a systematic search process with inclusion and exclusion criteria, and the studies included were subjected to critical assessment and systematic analysis (15). No specially designed computer programs were used in the selection or analysis process. The PRISMA 2020 Checklist was employed (16).
Search strategy
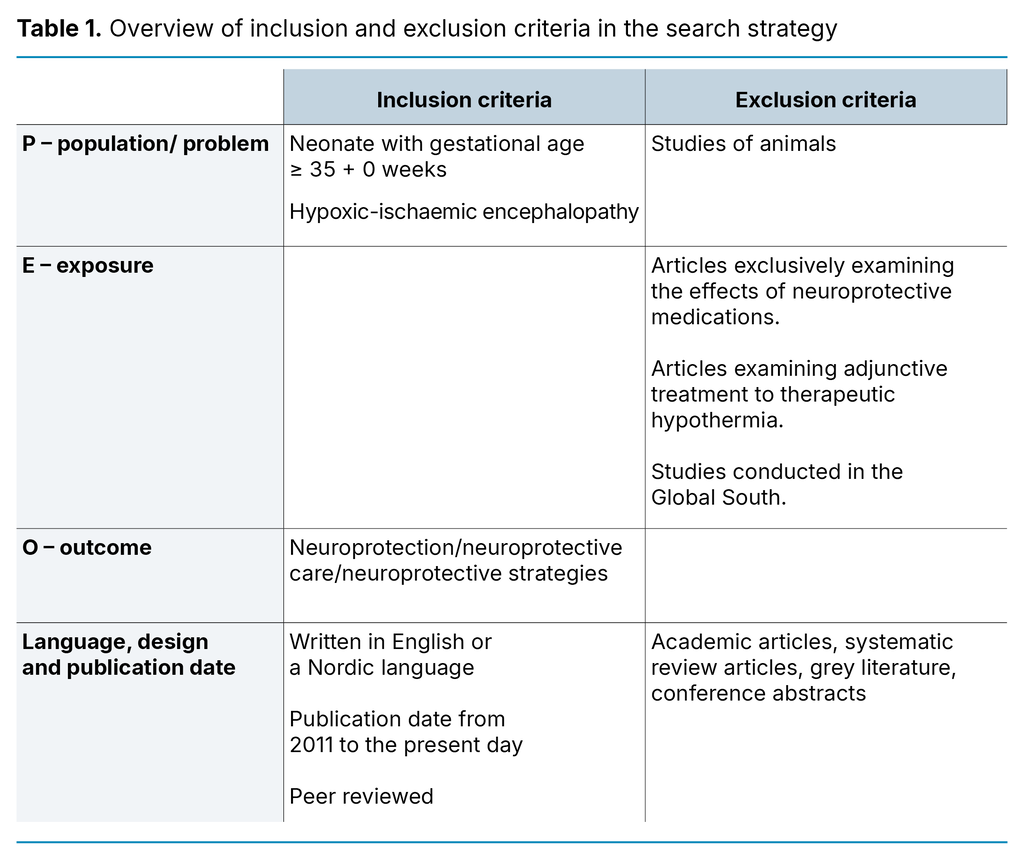
The search strategy was based on a PEO form (Appendix 1), which combines the elements Population, Exposure and Outcome (17). Several additional searches were initially performed using ‘nurse’ in the Exposure element, but this significantly limited the results. It was therefore assumed that the nurse’s role is inferred in the care and treatment being studied.
Articles identified when devising the search strategy indicated that hospitals in the same country can have different criteria for TH, including the gestational age threshold. The Norwegian guidelines provide for neonates with a gestational age ≥ 35 + 0 weeks to be assessed for TH, even though, in principle, the threshold is ≥ 36 + 0 weeks (8).
We therefore included studies of neonates from 35 + 0 weeks. Systematic searches were conducted in Medline, Embase and CINAHL up until 31 August 2021. The search strategy and history for the various databases are presented in a separate form (Appendix 2).
The sample of articles is presented in a PRISMA flowchart (16) (Appendix 3). The first and last authors screened titles and abstracts and included articles that matched the inclusion and exclusion criteria specified in Table 1. Four articles (18–21) were identified in the systematic search. In addition, we included one article (22) that was identified when devising the search strategy (Appendix 3).
Quality assessment of studies included
The studies included were critically assessed by the first and last author separately using the Checklist for Cohort Studies from the Joanna Briggs Institute (23). The first and last author discussed each article until a consensus was reached.
Analysis strategy
It was not possible to synthesise the numerical data in the studies included, and the thematic analysis performed by the first author was therefore based on the studies’ textual content (15, 24). Thematic analysis consists of six different phases and ‘is a method for identifying, analysing and reporting patterns (themes) within data’ (24, p. 79). We provide a narrative presentation of the results. As no qualitative studies were identified, we chose a thematic analytical approach to the quantitative data, with a view to highlighting the results that address the research questions.
Results
Five cohort studies were included in the literature review: one prospective (18) and four retrospective (19–22). The quality of the articles was considered to be good to high. The quality assessment is further described in the critical assessment of the studies provided in Appendix 4, and in the literature matrix (Appendix 5 – in Norwegian). The studies included (18–22) were from hospitals with TH facilities that have developed and implemented procedures for the neuroprotective care and initial treatment of neonates being assessed for or receiving TH. All hospitals accepted neonates with moderate to severe HIE referred from local hospitals.
Two of the studies involve nurses specialising in neonatal nursing care (20, 21), one study uses the terms ‘nurse’, ‘neonatal nurse’ and ‘neonatal team’ (18), and two studies only refer to ‘neonatal intensive care unit’ or ‘referring hospital’ (19, 22). Two studies were conducted in the United States (18, 20), two in Canada (21, 22) and one in Australia (19). The studies include a total of 797 neonates with moderate to severe HIE.
Our analysis identified the following themes: ‘Specialised neuroprotective care based on knowledge and clinical competence’, ‘Nurses play a key role in adhering to protocols, guidelines and documentation’, and ‘Nurses’ role in initiating passive cooling’. A summary of the results is presented in Table 2.
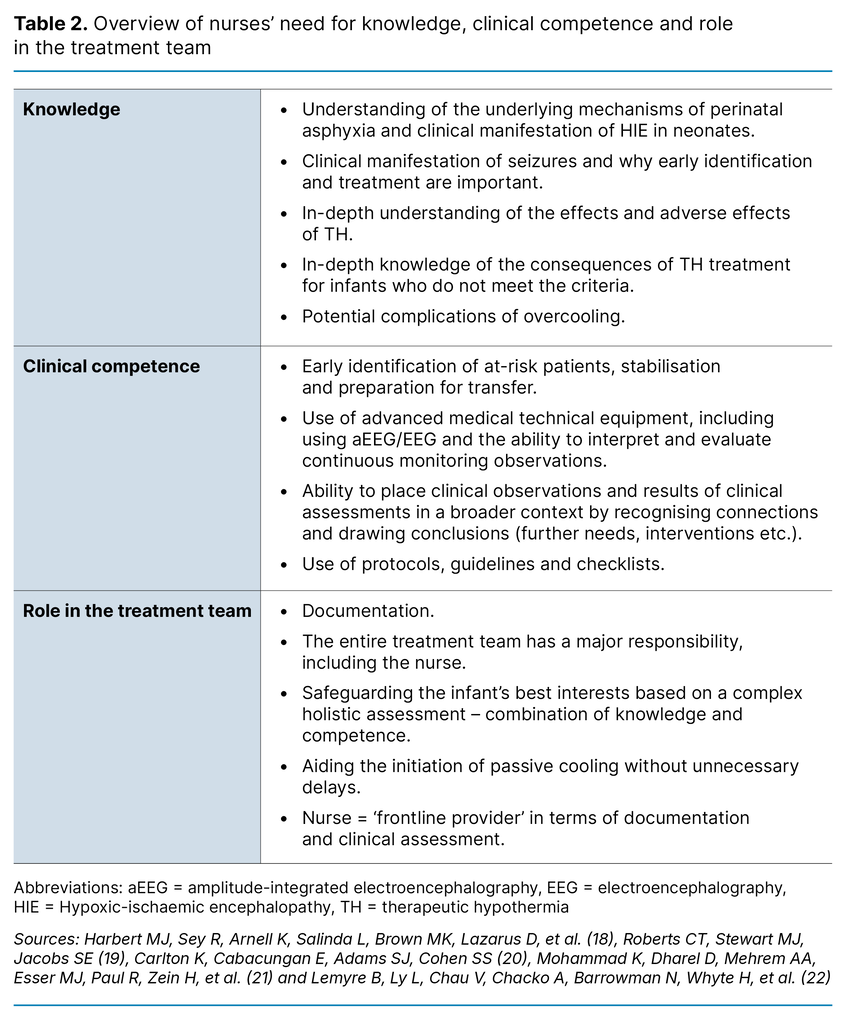
Specialised neuroprotective care based on knowledge and clinical competence
Harbert et al. (18) describe how when a neuro-intensive care service was introduced at both a regional therapeutic hypothermia unit and the affiliated local hospital, certain outcome parameters improved, including a reduction in the hospitalisation of neonates treated with TH. Nurses specialising in neurology were considered to be an important part of the treatment team, and there were always at least two of these nurses on duty (18).
In two of the studies, it emerged that nurses should have knowledge and competence in setting up and interpreting amplitude-integrated electroencephalography (aEEG), with a particular focus on identifying seizures (18, 21). They had a specialised and systematic approach to neonates who qualified for and underwent TH. This significantly reduced the number of identified seizures (38 per cent vs. 14 per cent, p = 0.003). A fall in mortality was also observed (17 per cent vs. 5.4 per cent, p = 0.03) compared to the period before the introduction of the specialised treatment programme (18).
Mohammad et al. (21) discuss key interventions at local hospitals with specialised training in neuroprotective care. The interventions were intended to stabilise and prepare the neonate for transfer. Simulation training was an important part of the specialised training, and nurses were part of the team that provided this training. Practical training included early identification of HIE symptoms, stabilisation and transfer to tertiary care.
The data showed that mortality and/or severe brain injury decreased from 35 per cent to 11 per cent (p ≤ 0.001) after the specialised training (21). A survey of 143 healthcare personnel, including 85 nurses, was also conducted after the specialised training. The respondents reported a supportive learning environment, practical applicability of the skills, and that they were comfortable using the acquired knowledge and skills in clinical practice (21).
Roberts et al. (19) conducted, but did not evaluate, specialised training prior to their study. Healthcare personnel at local hospitals were given an introduction to assessing, stabilising and initiating passive cooling for neonates with HIE.
Nurses play a key role in adhering to protocols, guidelines and documentation
Protocols and guidelines were drawn up in all studies at the respective hospitals to ensure adequate care and treatment (18–22). The study by Carlton et al. (20) showed that 54 per cent of neonates met the TH criteria based on documentation from clinical, physiological and neurological assessments.
Sixty-five per cent of these neonates were referred by local hospitals, and 65 per cent of those who did not meet the TH criteria had documented mild HIE (20). Standardised documentation was therefore introduced, with a focus on how long it took to assess cooling criteria: clinical HIE assessment according to the Sarnat system, HIE severity, seizures and when passive cooling was initiated (20).
Incomplete documentation was also identified by Roberts et al. (19) Carlton et al. (20) found that nurses specialising in neonatal care are ‘frontline providers’ in terms of documentation and clinical assessment.
Carlton et al. (20) demonstrated that, on average, 4.6 of the 6 categories in the modified Sarnat score were documented. Categories relating to muscle tone, followed by neurological reflexes, were most likely to be missing in the written documentation. This study (20) further showed that when standardised documentation was introduced, documented parameters, including the Sarnat score, increased.
Roberts et al. (19) revealed that important parameters such as Apgar score at 10 minutes of age, HIE severity and blood gas levels at < 60 minutes of age were not documented in 36.6, 9.5 and 22.8 per cent of study participants, respectively.
Nurses’ role in initiating passive cooling
The temperature of neonates with asphyxia will naturally decrease to a core temperature of 34–35°C within a short space of time. Allowing this to happen, even below 34°C, is referred to as ‘passive cooling’ (8). Two studies (19, 22) reported on passive cooling during stabilisation before transfer to a therapeutic hypothermia unit. Lemyre et al. (22) found that 71 per cent of neonates had reached a core temperature of 33–34°C within six hours of birth, and that the desired core temperature was reached earlier in neonates with severe HIE than with moderate HIE.
Harbert et al. (18) reported that the time to the desired core temperature increased after both the regional therapeutic hypothermia unit and the local hospital introduced specialised neonatal care (203 ± 110 mins. to 249 ± 115 mins., p = 0.05). Roberts et al. (19) found that cooling initiated by the referring hospital was started significantly earlier (p < 0.01) than prior to specialised training with an increased focus on passive cooling, and neonates reached the desired core temperature earlier (p < 0.01). Both studies (18, 19) reported overcooling (33°C) but did not mention any serious complications.
Lemyre et al. (22) observed that many healthcare personnel only initiate passive cooling after consulting the regional therapeutic hypothermia unit. This occurred in a total of 50.9 per cent of cases. Mohammad et al. (21) reported an increase in the number of those starting TH within six hours of birth in connection with specialised training (80.5 per cent before and 95.5 per cent after [p = 0.003]). In addition, the number of neonates who had reached the desired core temperature upon arrival at the therapeutic hypothermia unit increased (28 per cent before and 65 per cent after [p = 0.03]).
Discussion
Nurses’ need for knowledge and clinical competence relates to specific elements of patient care, with a view to ensuring swifter identification of at-risk patients and providing them with adequate care and treatment. These areas take priority in the specialised training across several of the studies included (18, 19, 21) and can be linked to nurses’ clinical judgement (25).
According to Benner (25), the nurse’s clinical judgement relates to their ability to act. This skill evolves through the progression from novice to advanced beginner, competent practitioner, proficient practitioner and expert. Nurses at the expert level assess the overall situation and act based on a complex picture, unlike the novice, who considers the separate components of the situation individually (25).
According to the Norwegian Directorate of Health, the minimum requirement is one specialist nurse per shift in departments with the lowest treatment complexity, known as category 2 (26). These departments must be able to ‘initiate passive cooling for children with brain injury due to oxygen deprivation before transferral to another department’ (26, p. 7). This task is likely to need specialised training. The results from our literature review indicate that such specialised training in neuroprotective care in the early phase impacts on certain outcome parameters in this patient group (18, 21).
Other research shows a reduction in the number of neonates with brain injuries after specialised care was implemented. It also shows a reduced incidence of seizures that require treatment in moderate to severe HIE (27). Based on this, we therefore believe there is a correlation between a strengthened focus on specialised care and improved patient outcomes. Our literature review shows that specialised training, particularly at local hospitals but also at regional therapeutic hypothermia units, can improve the quality of patient care pathways (18–21).
Simulation training helps consolidate theory and practice, and the nurses felt more confident in caring for patients after the training (21). In order to translate theory into practice, nurses need to see connections, and this is linked to their gradual evolution from novice to expert (25).
Specialised training can improve patient outcomes
The results confirm that specialised neurological care requires nurses to address all aspects of neonates in need of TH: make observations, conduct clinical assessments and implement appropriate and necessary interventions (18–22). Based on Benner’s theory (25), we argue that experts have the ability to make a much more complex overall assessment than novices. The literature review shows that nurses play a central and active role in clinical patient care in all stages, and that specialised training can improve patient outcomes (18, 21).
Nurses and specialist nurses are pivotal to the implementation of measures that enhance knowledge and competence, as well as to carrying out targeted clinical patient care (18, 20, 21). The literature review sheds light on how nurses practise their profession in complex patient situations that require knowledge and competence as well as crucial tools, such as guidelines, flowcharts and protocols (18–22).
Several of the studies included highlight training in the use and interpretation of aEEG or EEG (18, 21). The study by Harbert et al. (18) shows that such knowledge and competence combined with a more holistic approach reduce the incidence of identified seizures. Recent research indicates that a nurse’s knowledge and competence in assessing clinical observations and interpreting aEEG have a bearing on how quickly interventions are implemented (28).
A stronger focus on targeted training is needed to optimise and standardise clinical practice (29). It is crucial that seizures are identified quickly. This highlights the need for nurses to have in-depth knowledge of the clinical manifestation of seizures and why early identification and treatment are essential (29).
Early initiation of passive cooling at the local hospital is crucial
Two of the studies in the literature review (19, 22) demonstrate that early initiation of passive cooling at the local hospital is crucial for the outcome. The need for extensive resuscitation can be interpreted as an objective sign of severe asphyxia and can inform assessments of the severity of the asphyxia. This contributed to earlier initiation of passive cooling (22). Conversely, the need for advice and guidance delayed the initiation of passive cooling (22).
In comparison, empirical data from Roberts et al. (19) show that the time until the desired core temperature was achieved was significantly shorter when the local hospital initiated passive cooling. This finding is consistent with other findings in our literature review, indicating a marked increase in the number of neonates undergoing cooling within the first six hours of birth. We also identified an increase in the proportion of neonates reaching the desired core temperature upon arrival at the therapeutic hypothermia unit (21).
However, Harbert et al. (18) demonstrated that the time taken for the infant to reach the desired core temperature increased after the introduction of specialised care. Possible reasons may be related to careful temperature monitoring to prevent overcooling. Two studies (19, 22) described several cases of overcooling, but there were no associated complications. Other research indicates that, upon departure from the local hospital, the basal temperature of neonates with severe HIE was 0.9 °C lower than those with mild and moderate HIE (30).
This finding highlights the importance of continuous temperature monitoring. Nurses have numerous tasks to take care of during the initial phase and must have the knowledge and competence needed to master the complexity of the tasks. As an extension of this, nurses must possess knowledge about various clinical observations and assessments that have a bearing on the initiation of passive cooling for neonates with moderate to severe HIE. They must also be aware of the potential complications of overcooling. Furthermore, part of their role in the team entails ensuring that unnecessary delays are prevented.
Patient safety can be impacted by the quality of documentation
One of the articles included pointed out that the nurse is a ‘frontline provider’ of crucial aspects of clinical practice and thus plays a key role in the treatment team (20). This is consistent with other research stating that a nurse specialising in neonatal care is a key contributor to the application of evidence-based practice to improve services and elevate competence (31). Incomplete documentation was also found in several of the studies included (19, 20).
Specialist nurses are portrayed as important contributors to the documentation and execution of clinical assessments in this patient group (20). Incomplete documentation in the initial phase may lead to questions about whether the infant really qualifies for TH. This can result in administering TH to neonates who do not meet the criteria for treatment, or failing to identify neonates who do meet the criteria (20).
The quality of the documentation of clinical assessments can impact on patient safety and the professional standard of treatment, which can have both positive and negative implications for the infant. The European guidelines for newborn resuscitation emphasise the importance of thoroughly documenting interventions and clinical observations to ensure adherence to relevant protocols for further care and treatment (32). Incomplete documentation combined with insufficient knowledge and competence may result in infants with moderate to severe HIE not being identified and, consequently, not receiving the necessary care and treatment.
Methodology
The study meets the requirements for a systematic review article with literature searches in three relevant databases (15). One of the weaknesses of our study is the lack of systematic searches in Scopus. Another is that we did not use search terms such as ‘training’, ‘care’ and ‘treatment’. The first and last author contributed to the inclusion and exclusion processes for primary articles, as well as the individual quality assessments of studies.
A further weakness of the literature review is the limited number of studies identified. The limited number of studies that met the inclusion criteria suggests a need for more research on the topic. A majority of the studies (18, 20, 21) scored high on methodological quality, which strengthens our literature review and its findings.
Conclusion
This systematic review demonstrates that standardising specialised care and treatment for patients with HIE can help improve certain outcome parameters. Nurses providing neuroprotective care in the initial stabilisation phase before transfer to regional therapeutic hypothermia units require advanced knowledge and clinical competence. They also play a key role in the treatment team.
Nurses need knowledge and clinical competence in the early identification of at-risk patients, stabilisation and preparation for transfer. They also need knowledge about the potential complications of overcooling, as well as an in-depth understanding of the effects and adverse effects of TH. Clinical competence involves the ability to use advanced medical technical equipment, including the use and interpretation of aEEG or EEG.
They must also be able to conduct relevant clinical assessments and actively use protocols, guidelines and checklists. Finally, they must help ensure that documentation is adequate.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge





Comments