Infection surveillance in nursing homes in an 18-month period during and after the COVID-19 pandemic
Summary
Background: Healthcare-associated infections are a significant cause of suffering and mortality among nursing home residents. Many of these infections are treated with antibiotics. This widespread use can increase antimicrobial resistance, which is one of the biggest global public health challenges. The primary strategy for reducing antibiotic use is to decrease the number of infections. Infection surveillance is a crucial part of infection prevention and should be initiated to quickly control outbreaks and prevent transmission. Most nursing home residents have weakened immune systems and impaired functional abilities, making them particularly vulnerable to severe illness and death from infections.
Objective: To monitor infections in nursing homes over an extended period and examine the prevalence of various types of infections, the types of antibiotics used in nursing homes, and how sociodemographic variables associated with the prevalence of infections changed during the pandemic.
Method: Healthcare personnel from 22 nursing home wards submitted weekly reporting forms over an 18-month period between February 2021 and August 2022. The reports from each ward included information about the number and type of infections, residents’ sex and age, antibiotic treatment, and type of antibiotics used. We employed descriptive and fixed-effects regression analysis.
Results: A total of 1625 infections were reported. Of all new infections, 91.8% originated in the nursing home, and 88.2% of these were treated with antibiotics. Urinary tract infections were the most frequently reported, followed by respiratory tract and skin infections. The active ingredients trimethoprim-sulfamethoxazole, amoxicillin and mecillinam were the three most used antibiotics. The number of hospital admissions increased in line with the number of infections throughout the study period.
Conclusion: The findings from this quantitative prospective study document infections and antibiotic use in Norwegian nursing homes. Many nursing home residents contract infections and consequently need to be hospitalised. Infection prevention, which includes infection surveillance, can help reduce the number of infections, thereby decreasing suffering and mortality in this patient group. Reducing the number of infections will also decrease antibiotic use and the development of antibiotic resistance.
Cite the article
Sandbekken I, Hermansen Å, Grov E, Utne I, Løyland B. Infection surveillance in nursing homes in an 18-month period during and after the COVID-19 pandemic. Sykepleien Forskning. 2024;19(97178):e-97178. DOI: 10.4220/Sykepleienf.2024.97178en
Introduction
Healthcare-associated infections (HAIs) are infections that occur in a patient in a hospital or healthcare institution. HAIs are prevalent and often lead to suffering and mortality among nursing home residents (1, 2). Many of these infections are treated with antibiotics and widespread use contributes to antimicrobial resistance (3). The United Nations (UN) considers antimicrobial resistance to be one of the top global public health problems (4).
In nursing homes, nurses play a crucial role in limiting the unnecessary prescription of antibiotics and the spread of antibiotic resistance (5, 6). The most effective strategy for reducing widespread use of antibiotics is to decrease the number of infections (3, 7).
An important aspect of infection prevention is monitoring the number of infections (8, 9). This can provide us with information and knowledge about the frequency and types of infections. Early detection of an infection outbreak is essential so that preventive measures can be implemented before the infection spreads further (5, 10).
The World Health Organization (WHO) believes that infection surveillance should be a top priority in institutions (8). In the Norwegian Ministry of Health and Care Services’ action plan for improving infection control in order to reduce HAIs 2019–2023, one of the goals is to improve infection surveillance in hospitals and primary care institutions (5).
The goals outlined in the action plan have not yet been realised. Norway monitors many conditions and has quality registries for these. However, there is no system for continuous infection surveillance in healthcare institutions (5). The Norwegian Institute of Public Health conducts a prevalence survey twice a year (NIOS-PIAH), which asks how many patients have the four most common HAIs on the measurement day (2).
The response rate has been low over time, even though participation is mandatory for nursing homes. In November 2023, only 47.5% of nursing homes in Norway participated. The survey revealed that 3.5% of nursing home residents had an HAI. Of these, 1.7% had urinary tract infections, 0.9% respiratory tracts infections, and 0.7 and 0.1% had skin and wound infections or post-surgical wound infections, respectively (2).
During the COVID-19 pandemic, morbidity and mortality rates increased among older adults, with nursing home residents being particularly vulnerable (11, 12). Most nursing home residents are older, and the natural ageing process can lead to a weakened immune system and reduced physical and cognitive abilities (13–15).
Advancing age also increases the risk of multiple and chronic diseases, which can lead to frailty (13). This combination makes nursing home residents particularly prone to infection (14, 15), and there is little that can be done to avoid these risk factors. They also tend to experience more severe outcomes from infections, such as prolonged hospital stays, suffering, and death (2, 9, 16, 17). Norway’s Cause of Death Registry shows that infections are the third most common cause of death in healthcare institutions outside the hospital setting (18). Many of these infections could have been prevented (2, 9, 16).
This study is the first to map infection incidence and antibiotic use in a sample of nursing homes over time in Norway. The objective of the study was to monitor infections in nursing homes over an extended period in order to examine the prevalence of various types of infections, the types of antibiotics most frequently used in nursing homes, and how sociodemographic variables associated with the prevalence of infections changed during the pandemic.
Method
Design
This study is a quantitative prospective study using weekly reporting forms to monitor infection prevalence in nursing homes over an 18-month period. Data were collected between February 2021 and August 2022.
Sample and recruitment
In December 2020, 17 nursing homes hosting clinical placement students from Oslo Metropolitan University (OsloMet) received information about the study via email, along with an invitation to participate. In January 2021, we contacted the nursing homes again by phone to provide additional information about the study and reiterate our invitation to take part.
Reporting forms and data collection
Nursing home wards selected staff to submit weekly reports on infections and antibiotic use via the digital platform Nettskjema.no. The responses were sent directly to the Services for Sensitive Data (19).
The reporting form included questions about how many residents currently had an infection or had had an infection in the past week, their sex and age (≤ 84 or ≥ 85), as well as when and where (at the nursing home or not) the infection began, the type of infection, whether they had more than one infection, and whether antibiotics were used to treat the infection. If they had received antibiotics, we asked about the type of antibiotic, the start date and the estimated duration of the treatment.
The reporting form was devised specifically for the project, based on the clinical experience of the authors and the staff at a nursing home ward. The form was pilot tested by the department head and the nurses in one ward before the study began. Based on their feedback, we revised the wording of some questions and added several antibiotic options to make the form easier and faster to complete.
The wards received an email reminder the following week if they had not submitted a report. We called the wards if several weekly reports were missing.
In addition to the reporting form, the wards were sent a questionnaire on sociodemographic variables twice during the study period: in the summer of 2021 and 2022. This form contained questions about the type of ward (long-term or short-term), the total number of beds and residents, residents’ age (≤ 84 or ≥ 85) and sex, the number of full-time equivalents (FTEs), and the number of nursing FTEs.
Data analysis
Statistical analyses were performed in Stata version 16. We reviewed the reports in their entirety. Weeks with missing reports were recorded as missing. Healthcare personnel could select the category ‘Other’ for both infection and antibiotic type, and provide free-text responses.
Under ‘Infections’, the ‘Other’ category included 50 different types of infections, while under ‘Antibiotic’, the category consisted of 26 different types. The ‘Unknown focus’ category under ‘Infections’ indicates that healthcare personnel had found an infection but were uncertain about the type.
Descriptive analyses were performed, including cross tabulation. We conducted fixed-effects linear regression analyses to examine which sociodemographic variables could be associated with infection prevalence and how these variables changed over the course of the study. The 18 months were divided into three periods, each spanning six months.
All significant variables in bivariate analyses at one of the three time points were incrementally included in a multiple regression analysis for each time period. The number of infections reported each week was used as the dependent variable. An interaction term between ‘Ward type’ and ‘Percentage of nursing positions’ was included in the regression analysis.
A significant result indicates that the effect of the number of nurses (percentage of nursing positions) on the number of infections differs depending on the ward type. The variable ‘Occupancy rate’ indicates the percentage of the ward’s beds that are occupied, and the variable ‘Percentage of nursing positions’ refers to the number of FTEs. P-values < 0.05 were considered statistically significant.
Ethical considerations
This study is part of a larger project that has been reviewed and assessed by the Regional Committee for Medical and Health Research Ethics (REK), reference number 196911 and 226694/REK South-East. Sikt – the Norwegian Agency for Shared Services in Education and Research found that the project complied with data protection regulations, reference number 118936.
Nursing home residents and their families received a letter giving them information about the study and informing them that they could opt out of data being collected on them for the study and that they could withdraw at any time. Before the study could commence, the department head or quality manager at each nursing home received an information letter and had to sign a cooperation agreement for each ward in the study.
Results
A total of 22 nursing home wards from 9 different nursing homes wished to participate in the study. The wards consisted of 3 short-term care units and 19 long-term care units in 2021, and 2 short-term care units and 17 long-term care units in 2022. Two wards were closed in the spring of 2022, resulting in two fewer wards in 2022.
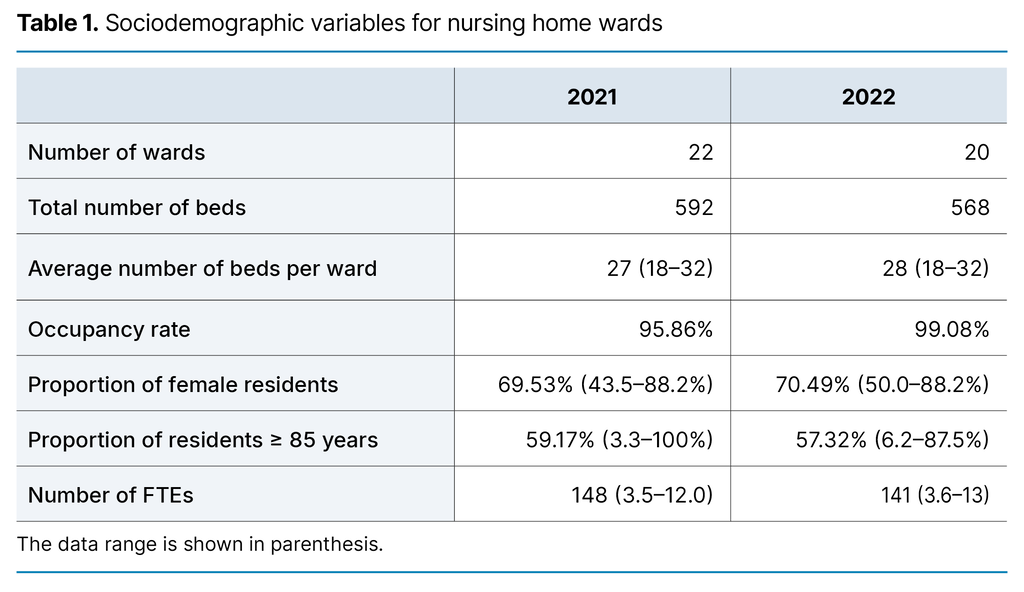
In the summer of 2021, 15 of the wards were organised into several small groups with their own kitchen. All residents had their own toilet, while seven wards were a single large ward with shared toilets for several or all residents. In the summer of 2022, 15 wards still had small groups and individual toilets for residents, while the number with a single large ward and shared toilets was reduced to five. Table 1 shows sociodemographic variables.
During the 83 weeks of reporting, we received 1391 weekly reports. Each ward submitted an average of 63 reports, but there was significant variation, ranging from 31 to 81.
Infections in nursing homes
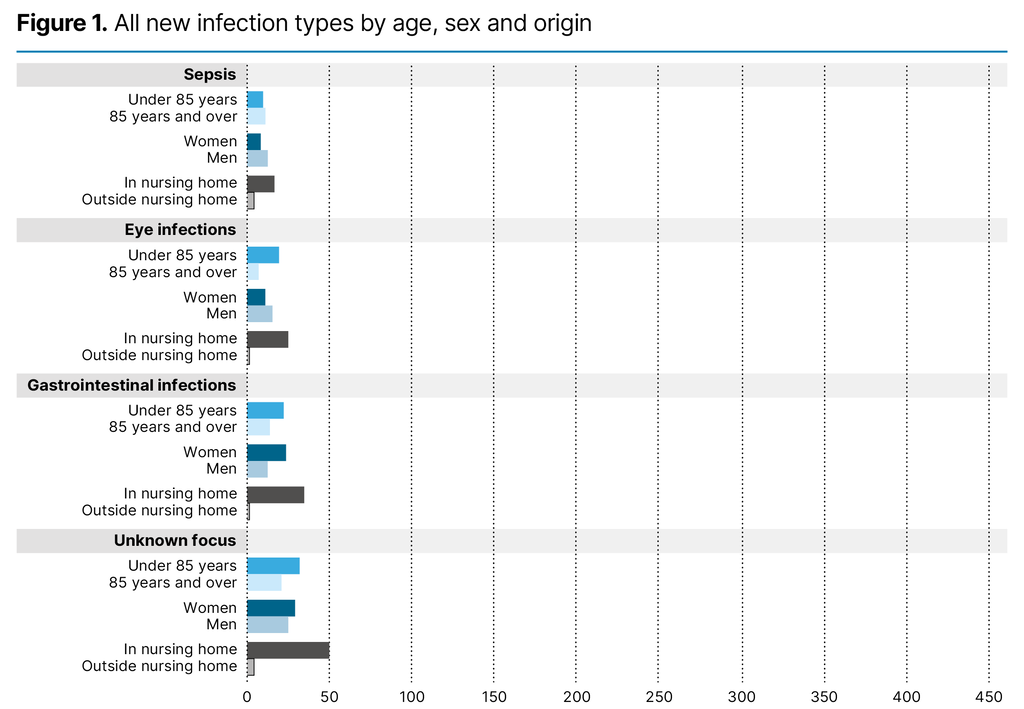
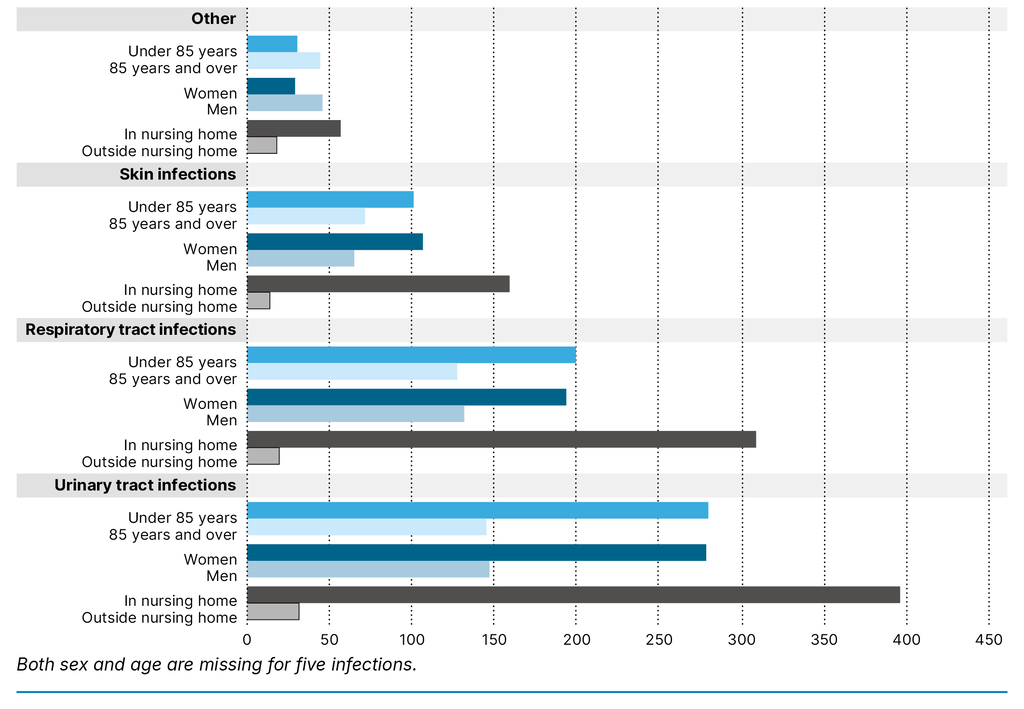
Over the 18-month data collection period, 1625 infections were reported. Of all new infections, 91.8% originated in the nursing home, while only 8.2% were contracted prior to admission to the nursing home. In the short-term care units, this percentage was higher: 19.7–27.8. It was reported that 30.0% of the infections lasted more than one week. The most common infections were urinary tract infections, followed by respiratory tract and skin infections (Figure 1).
Antibiotic use in nursing homes
The different infection types were generally treated with antibiotics, and 88.2% of all new infections were treated with antibiotics. Urinary tract infections were treated with antibiotics in 98.2% of cases, skin infections in 92.5% and respiratory tract infections in 75.9% of cases. The exception was gastrointestinal infections, where 61.8% of the infections were not treated with antibiotics.
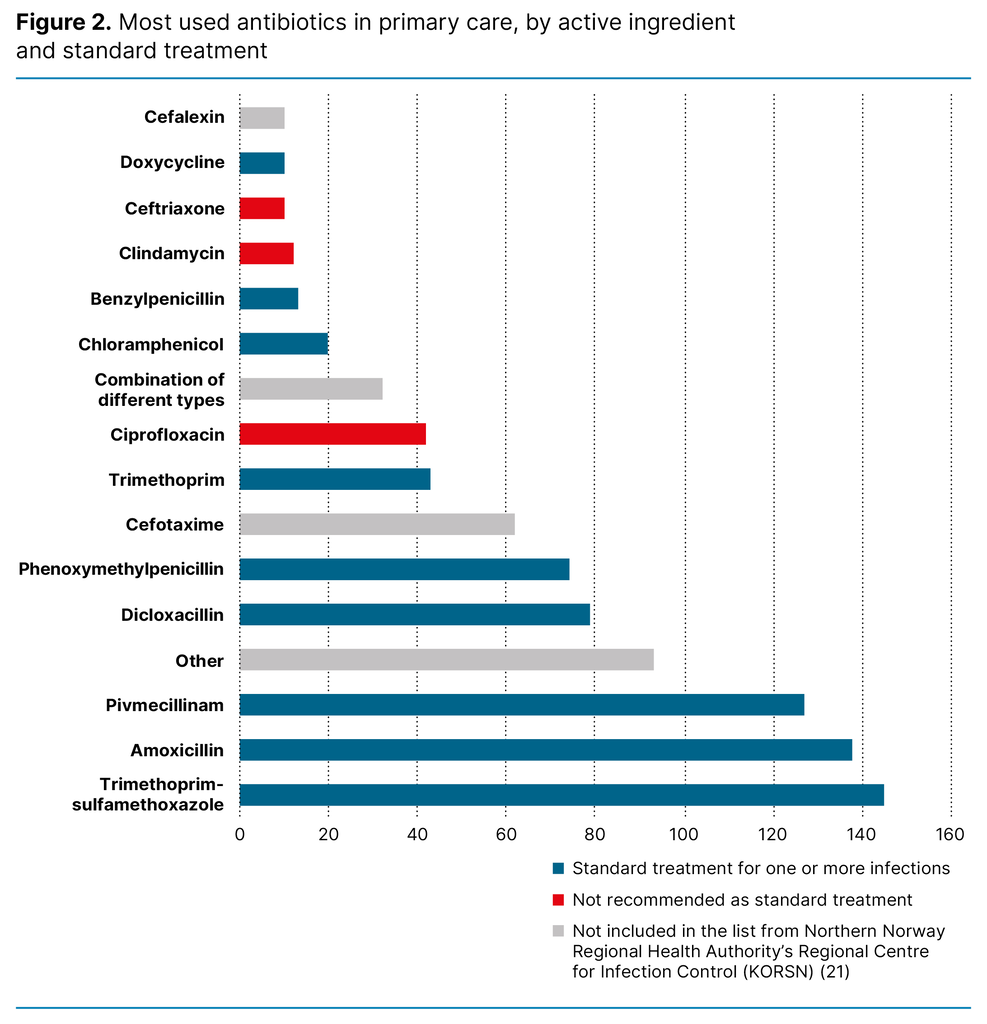
The active ingredients trimethoprim-sulfamethoxazole, amoxicillin and mecillinam were used the most. Figure 2 shows the distribution of the various active ingredients, colour-coded to highlight which antibiotics are standard in primary care (20, 21).
The category ‘Other’ consists of 20 different antibiotics, all of which were used fewer than 10 times. ‘Combination of different types’ can refer to either two different medications or a single-pill combination.
The most common treatment for respiratory tract infections was amoxicillin (34.2%), followed by phenoxymethylpenicillin (19.9%). Urinary tract infections were treated with pivmecillinam in 32.5% and trimethoprim-sulfamethoxazole in 27.1% of cases. Skin infections were most frequently treated with dicloxacillin (47.3%), followed by the ‘Other’ category (26.0%).
Gastrointestinal infections (76.9%), sepsis (33.3%), infections of unknown focus (26.3%), and the general infection category ‘Other’ (40.0%) were most frequently treated with antibiotics from the general antibiotic category ‘Other’. This category consisted of different types of antibiotics, each of which was reported fewer than ten times.
Sociodemographic variables associated with the prevalence of infections during the study
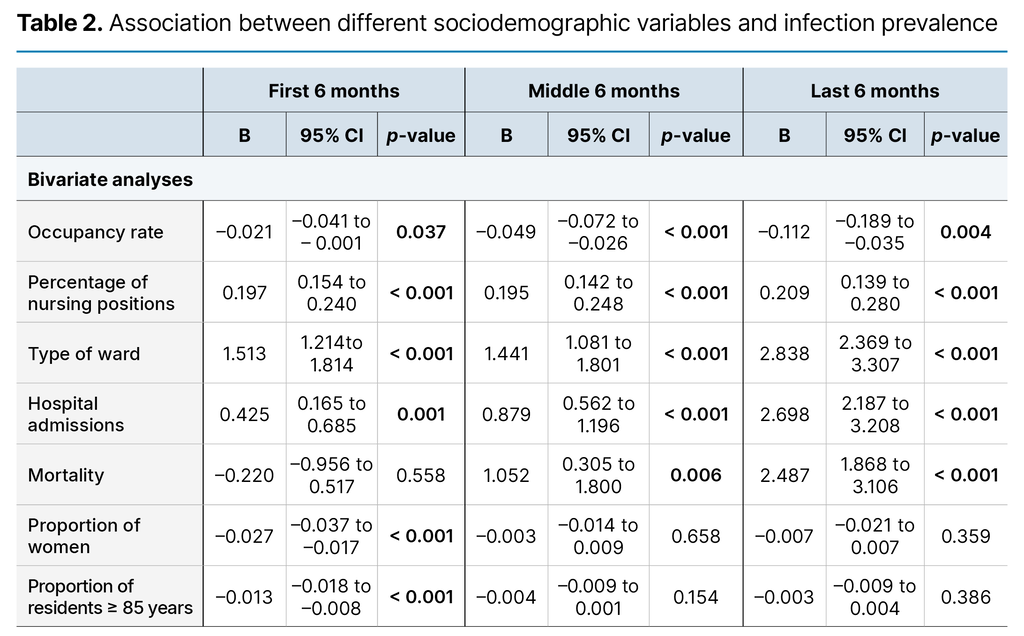
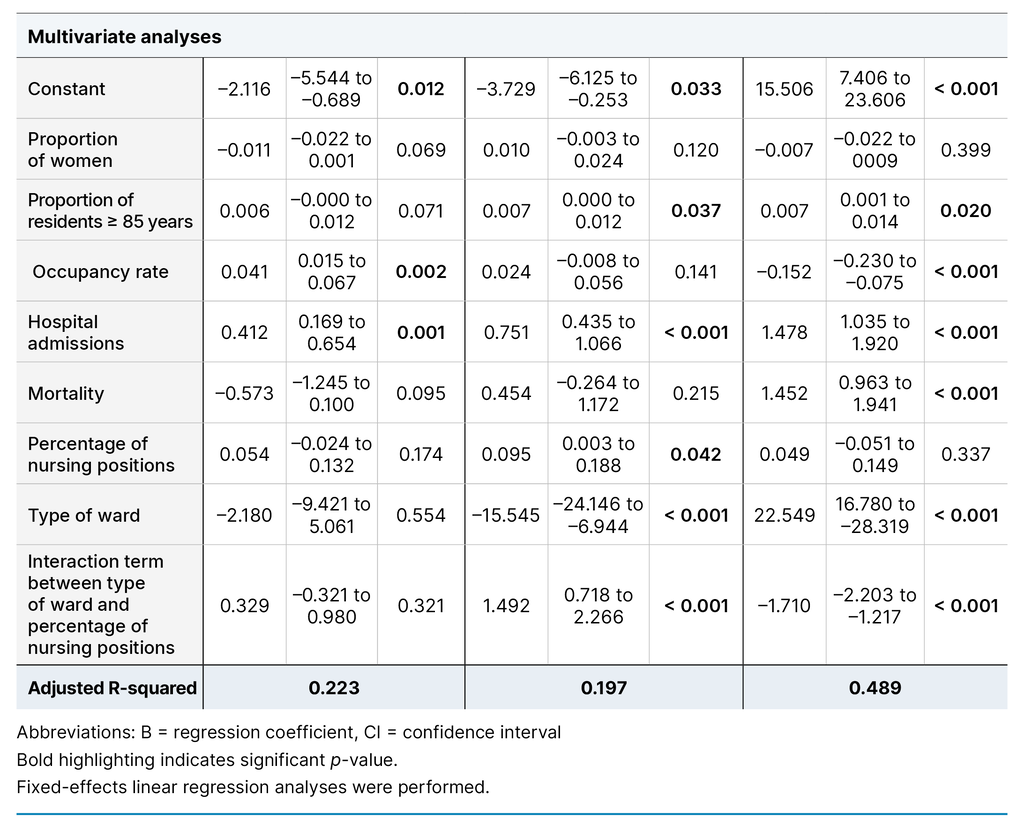
The results from the regression analyses show different significant findings across the three six-month periods. The results indicate that high infection rates occur simultaneously with a high number of hospital admissions, which is the only variable that continues to be significant throughout the entire period (Table 2).
The incremental inclusion of variables showed that the interaction term between ‘Ward type’ and ‘Percentage of nursing positions’ was the most important variable for explaining the change in the number of infections. Over the three time periods, this variable accounted for 11.99, 12.64 and 18.10% (adjusted R-squared) of the change in infection prevalence, respectively. In the last period, the hospital admissions variable was the most significant for explaining infection prevalence, accounting for 20.83%.
Discussion
This study is the first in Norway to monitor infections and antibiotic use in a sample of nursing homes over an 18-month period. It describes the prevalence of various types of infections and the antibiotics most frequently used in nursing homes.
Most infections originate in nursing homes
A full 88% of all identified infections in this study originated in nursing homes, and many of these could likely have been avoided with better infection prevention (9, 16). In 2022, Norway’s Cause of Death Registry showed that infectious diseases, COVID-19, influenza and pneumonia were the cause of 3161 of the 24 809 deaths in healthcare institutions outside the hospital setting. This makes infections the third most common cause of death in healthcare institutions outside the hospital setting, surpassed only by tumours and cardiovascular diseases (18).
Unlike tumours and cardiovascular diseases, most infections are contagious and can be prevented in nursing homes. Nursing home residents are generally vulnerable due to their advanced age, multimorbidity (13–15) and reduced intrinsic capacity. This makes nursing home residents particularly susceptible to infections and the severe consequences of these (2, 9, 16, 17).
In addition, older adults often experience atypical symptoms and can find it difficult to convey relevant symptoms to healthcare personnel (15, 22). These factors combined can lead to delayed initiation of necessary treatments as well as a more severe course of disease, such as hospitalisation, sepsis and death (15). Hand hygiene is the most important and cost-effective measure we have to prevent the spread of infection (8).
Previous findings from this research project have shown just 58% hand hygiene adherence in nursing homes (23), but multimodal interventions could improve this (24). However, the transmission of infection is complex, and good hand hygiene alone will not prevent all infections. Continuous infection surveillance will enable a rapid response with appropriate infection control measures, thus reducing the number of residents infected.
Antibiotic use in nursing homes
The antibiotics most commonly used in our study were largely consistent with those most frequently prescribed to patients over the age of 75 in 2020, as reported in the Norwegian Prescription Database (25). Broad-spectrum antibiotics are the standard treatment for various infections (20), which may explain the prominence of several broad-spectrum antibiotics in our study.
It was not possible in our study to investigate whether antibiotics were prescribed with the correct indication. Errors and unnecessary use of antibiotics contribute to increased development of resistance, with broad-spectrum antibiotics fostering greater resistance than narrow-spectrum antibiotics (26).
One of the differences in our study from the Norwegian Prescription Database is that neither methenamine nor nitrofurantoin is frequently used. Neither of these antibiotics has been subscribed more than ten times during the 18-month period and they are therefore classified in the ‘Other’ category in this study. In the Norwegian Prescription Database, methenamine and nitrofurantoin were the sixth and eighth most used antibiotics in 2020 in the over 75 age group (25).
Methenamine, with the most recognised brand name Hiprex, is classified as an antibacterial agent with antiseptic properties. It is used for long-term prevention of chronic recurrent urinary tract infections (27). A 2016 study showed that Norway had the highest methenamine use in the EU/EEA (28).
The low reported use of this medication in our study is therefore surprising. One possible reason may be that nursing home doctors have become more restrictive in prescribing the medication. Research on the preventive effect of methenamine has been inconclusive (29). Consequently, there has not been a clear recommendation to use methenamine (30).
However, compelling evidence has recently emerged indicating that the medication may have a preventive effect, but only if the urine has the correct pH level and the substance it converts into, formaldehyde, is present at a certain concentration and remains in the bladder for a specific duration. It is not therefore expected that patients with permanent urinary catheters will benefit from methenamine (29).
Nursing home doctors may have taken this into account, which could explain the reduced use. However, it remains unclear whether the reduced use of methenamine has led to an increase in the use of another antibiotic. Methenamine is an antiseptic agent, and there is currently no evidence that it leads to increased antimicrobial resistance (30). Consideration should therefore be given to whether the use of methenamine is more beneficial than the increased antimicrobial resistance that stems from recurrent urinary tract infections treated with antibiotics (31).
Another reason for the low reported methenamine use could be that the nursing homes in the study did not think to include preventive antibiotic treatment. Although the reports have shown a few instances of preventive treatment, there have been fewer than ten cases per antibiotic, and this has not therefore been highlighted in the study.
Number of infections varied throughout the data collection period
Many infections exhibit a seasonal trend, with a higher incidence in winter (32). It was therefore interesting to observe the seasonal effects on the number of infections in this study. The interaction term was the primary explanatory variable in the model, indicating that the interplay between ward type and the number of nursing positions was significant. In the middle six months, wards with more nursing positions also had a higher number of infections. We can interpret this to mean that nurses are more likely to detect and report infections.
Ward type is the significant finding with the greatest association with infection incidence. In the last six months, infections increased in short-term care units, which may be due to a higher number of patients being admitted with infections in these units.
In the middle six months, the short-term care units had fewer infections than the long-term care units. It is difficult to know why, but various factors related to the pandemic may have impacted on our results. In the first six months of this study, there were fewer infections and deaths in Norway than would normally be expected (33), and this is likely due to the COVID-19 vaccine and stringent restrictions.
During the middle six months, infections and hospital admissions both increased in the autumn, which led to further lockdowns (34). Norway experienced an excess mortality of 11.8% in 2022 (33) in the last six months of the study, when the number of infections and hospital admissions during the pandemic peaked (34).
COVID-19 may have impacted on the organisation of nursing homes, leading to more patients who would normally be admitted to short-term care units being admitted to hospital or a dedicated COVID-19 ward instead. Hospital admissions are the only explanatory variable that remains significant across all three time periods.
However, the incremental inclusion of variables in the regression analysis shows that hospital admissions have a different explanatory power in the model and are the primary explanatory variable in the last six months. These findings support the interpretations above. Although nursing homes are now dealing with many infections independently and administering more intravenous therapy (35), an increasing number of residents are in such poor health that they require hospitalisation for proper treatment (15).
Strengths and weaknesses
The use of self-reporting questionnaires in the study was a limitation that led to incomplete reporting many weeks from some wards. Additionally, the reports may have been influenced by the person submitting them. Consequently, they do not necessarily reflect the full picture.
Although most reports were submitted in the same week they pertained to, retrospective reporting was also possible. This may have led to recall bias, as the staff might not accurately have remembered how many infections occurred going back in time.
Another weakness of the study is that we did not follow individual residents over time, so we do not know their outcomes or if certain residents experienced recurrent infections.
COVID-19 may also have had an impact on the results as it entailed periods with higher infection rates than normal but also stringent restrictions to prevent transmission. The consequence was periods with fewer infectious diseases than usual in the Norwegian population.
Nevertheless, the strength of the study lies in its weekly reporting over an 18-month period, which allowed us to observe the infection rate over time rather than just presenting a snapshot. The study includes various nursing home wards from nine different nursing homes. It also encompassed all types of infections and was not limited to the most common HAIs.
Conclusion
The findings from this study show that most infections in nursing home residents originated in the nursing home. Infections can cause suffering for nursing home residents, leading to hospitalisation and increasing the risk of death. Many of these infections could have been avoided with better infection prevention measures. Continuous infection surveillance in nursing homes must be prioritised to quickly control potential outbreaks.
The high proportion of infections treated with antibiotics in our study is surprising. Increased knowledge and awareness of recommended treatments for infections in nursing homes may help reduce the high use of antibiotics in these institutions. Reducing antibiotic use is a national goal and could also help to decrease antibiotic resistance.
Funding
This study is part of a doctoral project funded by the Norwegian Nurses Organisation, reference number 4207.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge


Comments