Nurses’ experiences with remote patient monitoring for cancer patients
Summary
Background: The use of digital tools in healthcare services (eHealth) is increasing and is thought to be part of the solution to the expected future challenges in the health service. Nurses at an outpatient clinic that treats patients with cancer and blood disorders have participated in an innovation partnership and helped to develop an app that is used for the remote monitoring of cancer patients. Knowledge about experiences with and benefits of remote patient monitoring (RPM) is currently limited.
Objective: The objective of the study was to explore nurses’ experiences with RPM in the monitoring of cancer outpatients being treated with medication. We also wanted to investigate how the tool impacts on the nurses’ working day and interaction with patients.
Method: The study has an exploratory qualitative design, with data collected in three focus group interviews. The sample consisted of 11 nurses with extensive experience in cancer care. The data were analysed using reflexive thematic analysis.
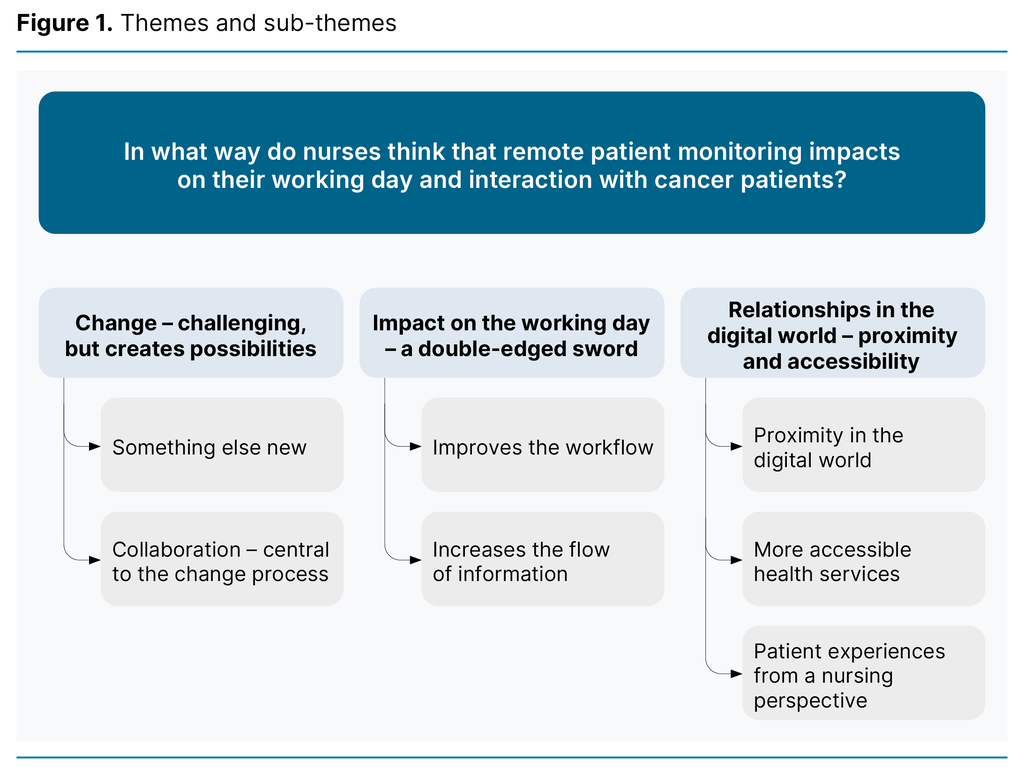
Results: The analysis resulted in three main themes with related sub-themes: 1) Change – challenging, but creates possibilities, 2) Impact on the working day – a double-edged sword and 3) Relationships in the digital world – proximity and accessibility.The nurses reported that RPM can streamline activity and provide more flexibility in certain areas, but they also experienced an increased flow of information, which demands more of their time and creates extra work. They highlighted the importance of their involvement in shaping the tool according to their needs and found that RPM can facilitate closer monitoring of patients.
Conclusion: The study suggests that RPM can have a positive impact on the patient-nurse relationship. It makes health services more accessible and provides information that can enable more efficient and flexible nursing care, but it can also lead to additional work. The study indicates that working with developers of digital tools is important for meeting the needs of healthcare personnel.
Cite the article
Bjørnebekk T, Børøsund E. Nurses’ experiences with remote patient monitoring for cancer patients. Sykepleien Forskning. 2024;19(96099):e-96099. DOI: 10.4220/Sykepleienf.2024.96099en
Introduction
Quality and efficiency are two important pillars for the health service of the future, and digital tools are essential to achieving this (1). The World Health Organization (WHO) suggests that there is a need to change how healthcare services are delivered, and highlights the importance of person-centred care when developing new ways of delivering health care (2).
The Norwegian health authorities have a focus on patients and service users being more involved in their own care. They also want to develop digital tools to improve the working conditions of healthcare personnel (3).
The health service is under substantial pressure, and future shortages of healthcare personnel will put further pressure on health services (4). Digitalisation may be a solution to future challenges, but whether digital technology will ease or add to the burdens of staff and patients is uncertain (4). More knowledge is still needed on how we can exploit the potential of eHealth (5).
The potential for remote patient monitoring in cancer care
RPM enables healthcare personnel to monitor patients at home (6). Service users measure their own vital signs and complete self-reported questionnaires that are then sent to healthcare personnel, who can subsequently respond and take the appropriate action (6).
Cancer patients often experience adverse side effects from their illness and treatment (7). RPM for cancer patients in the form of self-reporting can improve symptom relief and quality of life (7) and increase survival rates (8). Using RPM can also facilitate communication between healthcare personnel and patients, strengthen user involvement, improve time efficiency, enhance service quality and reduce resource use (9).
Although RPM can yield positive outcomes for cancer patients and healthcare personnel, implementation and uptake in the health services present challenges (9). A literature review points to a need for more knowledge on how RPM can be implemented and optimised. The literature review recommends exploring how work processes should be reorganised and what role nurses can play in utilising digital tools in cancer care (5).
Nurses’ focus on person-centred care
Health services across the world are increasingly focussed on person-centred care (2), where user involvement and shared decision-making are key aspects (10). To this end, Norwegian health authorities aim to create a health service in which the patient plays a more participatory role (3).
Nurses who feel that they are practising person-centred care are more satisfied with their jobs than other nurses and are more likely to stay in their job. However, the organisation of healthcare services, in which the focus is on operational factors and performance management, can make it challenging for nurses to provide good comprehensive care (11).
RPM for cancer outpatients
A Norwegian hospital entered into an innovation partnership with a technology company with the aim of developing an RPM system for cancer patients to improve the working day of healthcare personnel and patient care at an outpatient clinic. Nurses, doctors and nursing associates participated in the development process, which resulted in the Nimble app. Following an initial trial period from 2020 to 2021, during which around 100 patients tested the solution, the hospital decided to purchase the app and initiated the implementation process in spring 2022.
Nimble consists of different versions for patients and healthcare personnel and can be used on a mobile phone, tablet or computer. In the app, patients are asked to register symptoms and side effects in a self-reported questionnaire prior to a consultation or treatment, and this is then sent to the hospital.
Patients can also communicate with healthcare personnel via secure messaging such as a chat function. The solution also includes video consultations that can be initiated by healthcare personnel. Nimble is synchronised with the patient record system and can transmit data to an electronic chart.
The introduction of Nimble has led to changes in how nursing care is organised and entails new routines for nurses and nursing associates. A new role has been created, RPM manager, where a nurse has overall responsibility for checking that all alerts are followed up. If a patient sends a questionnaire in which some of the symptoms are outside the reference range, or if a message is received in the chat function, an alert is triggered for nurses and nursing associates. This appears as a red dot in the app.
The nursing associates respond to questionnaires and messages and contact a nurse or doctor if alerts are outside their area of expertise. Each nurse must check Nimble daily to monitor their primary patients. The log-in procedure is the same as for the hospital’s ICT systems.
Self-reported values within the normal range, such as no fever or side effects, self-reported blood pressure within the normal range and stable weight, are used as a basis for organising chemotherapy or immunotherapy, which will then be ready for the patient to start when they arrive at the outpatient clinic.
Objective of the study
The objective of the study was to explore nurses’ experiences with RPM for cancer outpatients being treated with medication. We also wanted to investigate how the tool impacts on the nurses’ working day and interaction with patients.
Method
The study has an exploratory qualitative design with an inductive approach. Data were collected in semi-structured focus group interviews, and the COREQ checklist was used to promote clear reporting of the research (12).
Sample and setting
The informants were recruited from an outpatient clinic at a hospital in Norway that treats patients with cancer and blood disorders, and experience with RPM was one of the inclusion criteria. Potential informants received information about the study from their manager. Those interested received oral and written information from the first author.
Out of 26 potential informants, 17 expressed an interest in participating. We interviewed 11 informants based on their availability at the time of the focus groups and operational considerations in the department. An operations coordinator divided the informants into three focus groups, independently of the first author.
The informants were women and men aged 30–63, with a median age of 48 years, who had been using the app for at least six months. They were nine oncology nurses and two other nurses, all with extensive experience in cancer care.
Data collection
We collected data based on a semi-structured interview guide (Appendix 1 (in Norwegian)) in three focus group interviews with a total of 11 nurses. Two of the groups each had four informants and one group had three. The interview guide was developed based on the authors’ preunderstandings, previous research and discussions. We pilot-tested the interview guide before the interviews. The first author, who conducted the interviews, had a collegial relationship with the informants.
The interviews were conducted at the informants’ workplace in autumn 2022 and lasted between 40 and 55 minutes. Informants were asked all the questions in the interview guide in addition to follow-up questions. They were given the opportunity to shed light on other topics that did not emerge when following the interview guide. Audio recordings were made of the interviews, and these were subsequently transcribed verbatim.
Data analysis
The first author coded and analysed the data together with the last author, using Braun and Clarke’s reflexive thematic analysis. This a six-step systematic process in which the researcher critically examines their own role in the research process (13).
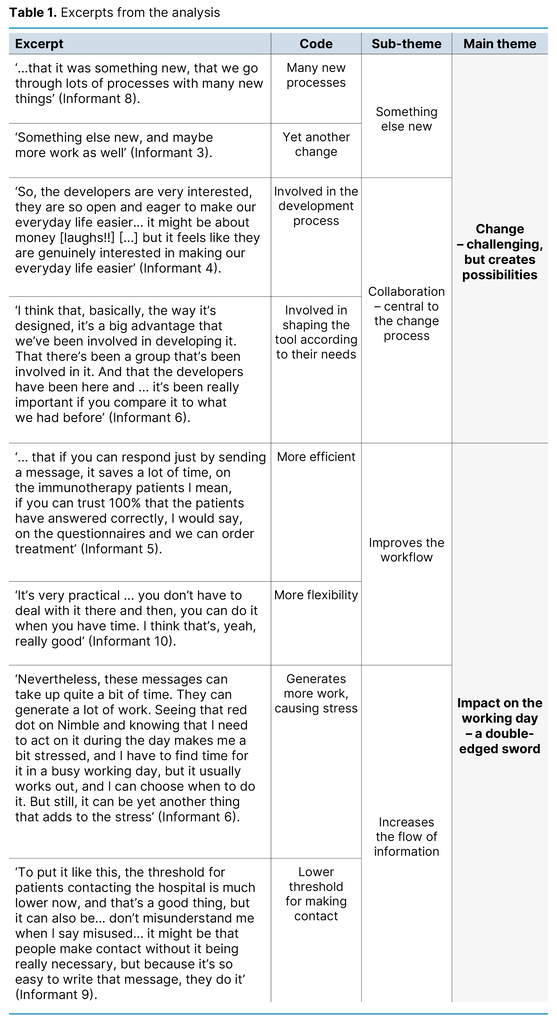
We started by identifying meaning units, which were coded. We then developed subcategories, which ultimately formed the basis for the main themes. Table 1 shows excerpts from the analysis.
Ethics and ethical considerations
Participation was voluntary. The participants received oral and written information in advance and consented to participation in writing. The study was reported to Sikt (the Norwegian Agency for Shared Services in Education and Research), reference number 802570. The audio recordings were collected via the dictaphone app Nettskjema-diktafon before being encrypted and sent to Nettskjema.no. The audio files were downloaded and stored in an approved location in accordance with routines at the University of South-Eastern Norway. They were then transcribed verbatim, and the transcripts were de-identified and treated confidentially.
The first author has been involved in implementing RPM in the informants’ workplace and her prior knowledge, experiences, thoughts and attitudes have influenced the research process, potentially limiting the emergence of new insights (14).
In order to ensure that the informants’ experiences come to light and that the emerging themes are not a construct of the first author’s biases, the analysis process was carried out together with the last author, who has no relationship to the informants. Additionally, the themes were presented to the informants after the analysis to check that they recognised the content.
Results
The informants described how RPM impacted their working day and the interaction with patients. The following three themes emerged from the analysis: 1) Change – challenging, but creates possibilities, 2) Impact on the working day – a double-edged sword and 3) Relationships in the digital world – proximity and accessibility (Figure 1).
Change – challenging, but creates possibilities
The informants described the changes that RPM had brought about in their working day. ‘Something else new’ was a recurring phrase in the focus group interviews, and the nurses talked about a constantly changing health service. The informants initially feared that using the app would be time-consuming:
‘Something else new, and maybe more work as well, when will there be time for it? I thought more work and something else new’ (Informant 3).
They emphasised that it was challenging to deal with changes, especially when there was already so much work. However, they also saw that RPM has future potential and considered it part of the evolution of the health service. They described RPM as a new way of working. They wanted to preserve human contact and stressed that RPM was not comparable to physical meetings.
Several informants also described how the self-reported questionnaires effectively assessed health status and side effects, and met the nurses’ need for information. The nurses also reflected on whether their own relationship to and interest in digital technology could impact on how quickly they adopt the new solution.
The informants valued the opportunity to contribute to the app development. They considered it essential that eHealth developers understand users’ needs, and described the collaboration with the developers as important for user friendliness.
Impact on the working day – a double-edged sword
The informants stated that RPM can aid their work and serve as a useful tool in their working day, but that it also created extra work.
The informants found that the app can help streamline their tasks. They pointed out that the self-reported questionnaires that patients completed the day before treatment provided the nurses with sufficient information to pre-order treatment such as chemotherapy and immunotherapy, which they described as time-saving. This results in shorter hospital visits, which is beneficial for both the patient and the outpatient clinic. One informant expressed it as follows:
‘Less time in the chair, more efficient from our perspective. And less time at the hospital for the patient’ (Informant 9).
The informants found that the self-reported questionnaire and the messaging function could also prevent unnecessary hospital visits. This benefitted both the nurses and the patients, as they could spend their time on something else and save on travel costs.
The informants felt that the messaging function created flexibility and gave them better control of their time. Several mentioned that they experienced fewer interruptions from phone calls and that it was beneficial to be able to respond to messages when it suited them. They could then consult with a colleague or the duty doctor before responding, enabling them to provide more informed feedback to the patient. The informants said that the app ensured quality-assured communication about important information and changes to medication dosage.
The informants also said that alerts in the app can lead to extra work and stress, as they are time-consuming to deal with, and no time is allocated for them alongside other tasks:
‘Nevertheless, these messages can take up quite a bit of time. They can generate a lot of work. Seeing that red dot on Nimble and knowing that I need to act on it during the day makes me a bit stressed, and I have to find time for it in a busy working day, but it usually works out, and I can choose when to do it. But still, it can be yet another thing that adds to the stress’ (Informant 6).
Some of the informants expressed that the app increases the flow of information, and that they have to deal with all the messages that come in. Some described how having to deal with multiple patient histories was burdensome.
Relationships in the digital world – proximity and accessibility
The informants described how the app makes them more accessible to patients. They said that patients who never used to call were now more likely to get in touch via the messaging function.
The nurses said that the app had the potential to improve the quality of service, and that increased accessibility is reassuring for the patients and allows nurses to monitor patients at home between treatments. The informants initially feared that they would feel less connected to the patients when using the technology, but after using the app, they found it was possible to use the technology to build a good relationship. One informant described it as follows:
‘You might think that digital communication makes you feel less connected to the patient, but I don’t really think that’s the case. If it’s someone I know, someone I’m monitoring, and have established a connection with, then they feel a bit like ‘my’ patient, and I also think that the patients feel they connect with me through the messaging function. Because I know the patient’ (Informant 6).
The informants also said that they felt the messaging function could provide more personal patient follow-up, described by one informant as follows:
‘I think it can almost feel even more personal, when they send a message, they write ‘Hi [name of the nurse]’, so it almost becomes even more personal than if they phone and get through to some random person on the other end, as it were’ (Informant 7).
However, the informants stressed that it was important to establish face-to-face contact beforehand in order to build a good relationship via the app.
Discussion
The main findings of the study highlighted how RPM for cancer patients impacted on the informants’ working day and the interaction with patients. The informants found the changes in work routines brought about by RPM to be challenging, but they also felt that the tool created possibilities. The informants found that the self-reported questionnaire and messaging function offered benefits such as increased flexibility, the opportunity to work more efficiently, and time-savings for both themselves and the patients.
The greater accessibility has also increased the flow of information, causing stress and extra work. The informants initially feared that RPM might have a negative impact on the nurse-patient relationship; however they found that the tool facilitated more personalised monitoring, contributing to person-centred care.
Changing practice through the introduction of technology
The informants had experienced several technology-related changes in recent years. Although they considered RPM to be part of this development, they found change processes challenging. Technology is advancing at a rapid pace and is changing the way nurses work and interact with patients (15). Healthcare personnel often face a high level of work pressure and have to prioritise which tasks to spend time on (16).
The informants also said they had identified potential in the app that could make certain aspects of their work easier. This finding is consistent with research showing that healthcare personnel are more likely to adopt a new digital solution if they believe it will have a positive effect on work routines (17), is user-friendly and has benefits (18).
The informants highlighted the importance of the collaboration with the developers and linked it to the app’s perceived user-friendliness and benefits. This type of collaboration is described in the literature as ‘co-creation’, where different actors and professions come together in an equal partnership to find new solutions (19). This can serve as an arena for staff learning and reflection, which can have a positive effect on the implementation process (20).
User involvement can prevent resistance (21) and facilitate successful change (16). The informants’ experiences with user involvement can also be observed in person-centred care, where the nurse’s professional autonomy is crucial for job satisfaction, as it includes being part of the decision-making about nursing practice (11).
As the informants themselves experienced, digital competence impacts on how they relate to digital tools. Healthcare personnel’s age, gender and experience influence acceptance and use of digital tools (18). A high level of digital competence is associated with a positive view of technology, while a low level is linked to concerns about patient safety and own competence (22).
People with advanced technological expertise reap greater benefit from digitalisation, while those with more limited knowledge find that it creates extra work (23). This may suggest that authorities and hospital management should take more of an interest in the importance of digital competence in relation to acceptance of digital innovation. They should focus on training and information, tailor solutions to needs and facilitate employees’ adoption of the solutions (17).
Since nurses can be key contributors in transforming healthcare services, it is important to leverage their visions and knowledge when developing care practices (24).
Possibilities and challenges linked to RPM
The informants highlighted several examples of how RPM impacted on their working day. They were able to work more efficiently and flexibly, which improved the workflow. In line with earlier research, the nurses found that the self-reported questionnaires provided useful information about the patient (9).
RPM streamlined the work and saved time for both patients and nurses (25). Furthermore, the nurses found that the messaging function allowed them to provide better feedback than in a phone call because they could consult with colleagues before responding.
The informants found there to be several positive aspects of RPM. However, they also said that the alerts from the app could lead to extra work and stress. Although technology is typically introduced to improve working conditions, it can also have unintended adverse effects, such as increasing the workload rather than easing it (23).
For the nurses in this study, this meant having to deal with more information. RPM results in more frequent and a higher volume of information about patients, which in turn reveals that more patients need treatment or follow-up (22). As a result, nurses need to spend time on patients beyond the scheduled appointments (9).
The nurses noted that digital tools can impact on their work in various ways. This can be explained by the complexity of hospitals, which consist of a multitude of occupational groups (4), and the multifaceted challenges faced by cancer patients (26). It is therefore difficult to find a solution that meets everyone’s needs, which suggests that future research should focus on cultural and human factors related to the implementation of digital tools (16).
The patient-nurse relationship with RPM
Oncology nurses highly value their interpersonal relationships with patients (27). The informants initially feared that the app would make them feel less connected to the patients. This finding is in line with other research indicating that nurses fear that digital tools could negatively affect the nurse-patient relationship (22), that technology might diminish their ability to provide holistic person-centred care, create distance and render the care more impersonal (28).
However, the informants in our study found that the app could facilitate a closer relationship, and highlighted the importance of the messaging function for achieving a closer dialogue. Nevertheless, face-to-face interaction is crucial for creating a digital relationship (22), which the informants also pointed out. The informants said that RPM cannot replace physical meetings, which is consistent with previous research. Clinical observations and non-verbal cues from the patient are lost (24), which places demands on the skills and expertise of the nurses (28).
The context for interaction is central to person-centred care (11). The informants described the app as a new setting and way of interacting with the patient. In line with research, the informants found that digital tools support person-centred care by strengthening the relationship between the patient and the healthcare personnel (29) and through empowerment and better communication between the healthcare personnel and the patient. Furthermore, digital tools can improve quality of life and physical and mental well-being (30).
These are values that nurses should base their practices on when adopting digital tools, as oncology nurses have a duty to safeguard ethical and professionally responsible application of innovations, health technology and digital competence (26). It is therefore important that the staff have sufficient knowledge and information about the advantages and disadvantages of RPM, and that they understand the reasons behind the implementation of the tool (16).
Strengths and weaknesses
A weakness of the study is that the focus group interviews only consisted of 11 nurses and that it was conducted in just one outpatient department. This may affect the transferability of the results to other occupational groups and settings. However, several of the findings are consistent with other studies of healthcare personnel’s experiences with RPM, which can strengthen the study’s validity.
The first author works at the same place as the informants, which led her to be particularly mindful of distinguishing between her professional and researcher role. To avoid the possibility of informants agreeing to participate in the study because of a collegial relationship, the first author was not involved in recruiting the informants or in assembling the focus groups.
The fact that the first author conducted the interviews and knew the informants may have made the informants feel secure enough to share information, but it may also have caused them to withhold information. The informants were given the opportunity to read through the results and indicate their recognition of the themes that had emerged, which can support the study’s credibility.
Conclusion
The study suggests that nurses have mixed opinions about using an app to monitor cancer patients. The nurses found that using the app streamlined the work and reduced phone interruptions, thus improving the workflow.
The tool can provide flexibility in the working day and have a positive impact on the nurse-patient relationship. However, RPM can also lead to an increased flow of information, which the nurses can find burdensome. The study further indicates that the collaboration between nurses and developers of e-Health technology can yield a useful and user-friendly solution.
RPM can be a valuable addition to the care of cancer patients receiving outpatient treatment. In order to achieve this, it is important that nurses are involved in tailoring the digital solution to their working day. Resources must also be allocated for new tasks that arise from this new way of organising nursing practices.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge
The article was first published 2 January 2025 due to a technical error. The correct publication date is 20 January 2025.


Comments