The surgical team’s adherence to recommended guidelines for surgical hand preparation: a quantitative observation study
Summary
Background: Surgical hand preparation is a vital infection prevention measure to reduce the bacterial count on the hands of the surgical team. It reduces the risk of transmitting micro-organisms to the patient through perforations in surgical gloves.
Objective: The objective was to investigate the degree to which scrub nurses and surgeons carry out surgical hand preparation in accordance with the Norwegian Institute of Public Health (NIPH) guidelines, and to find out if there is a difference between the occupational groups.
Method: We conducted a cross-sectional study in which we observed the length of time and the technique used in surgical hand preparation. We carried out 132 systematic observations of 52 surgeons and 32 scrub nurses. The data were analysed using regression analysis.
Results: We found that adherence to the NIPH guidelines for surgical hand preparation was low. The majority chose surgical antisepsis (58%) in preference to hand washing (33%), and 26% (n = 20) spent the correct length of time for surgical antisepsis. The average time spent was 90 seconds (120 seconds is recommended). The correct technique was used by 21% (n = 16). Only 12% followed both the recommended length of time and technique for surgical antisepsis. Scrub nurses had a higher probability of adhering to the guidelines than surgeons (p = 0,047). Adherence to the recommendations for surgical hand washing was somewhat better; 34% (n = 15) spent the correct length of time of 240 seconds, while the average time was 209 seconds. The correct technique was used by 34% (n = 15), but only 20% used both the correct length of time and technique for surgical hand washing. There was no difference between the occupational groups.
Conclusion: The study identified areas for improvement in relation to both time and technique in surgical hand preparation. The reasons for the low level of adherence have not been examined, but training, implementation and follow-up of the NIPH guidelines may have an impact on adherence levels.
Cite the article
Nieves V, Gundersen T, Mykkeltveit I. The surgical team’s adherence to recommended guidelines for surgical hand preparation: a quantitative observation study. Sykepleien Forskning. 2024;19(95142):e-95142. DOI: 10.4220/Sykepleienf.2024.95142en
Introduction
Postoperative surgical site infections inflict additional social costs and harm to patients in the form of longer hospital stays, unnecessary pain, suffering and increased risk of death (1). Preventive efforts are deemed to require less use of resources and are more cost-effective than surgical site infections (2). Correct hand preparation is a vital and simple infection prevention measure (3, 4).
The aim of surgical hand preparation is to reduce the risk of surgical site infections by removing transient flora and inhibiting the growth of resident flora (1). The Norwegian Institute of Public Health (NIPH) has drawn up national guidelines explaining how to carry out surgical hand preparation step-by-step, both in terms of time spent and technique used. The NIPH presents two different methods: surgical hand antisepsis and surgical hand washing (5).
While little research has been carried out on adherence to correct surgical hand preparation practice, research shows that healthcare personnel have a low level of adherence to the guidelines for hand preparation (6–8). Insufficient antiseptic solution is used, and certain areas on the hands and elbows are not washed according to the procedure (9).
Correct practice is influenced by both personal and situational factors. A lack of knowledge about correct practice as well as a failure to understand the risks of transmitting micro-organisms have an impact on adherence (8). In addition, research shows that men have a lower level of adherence to surgical hand preparation guidelines than women, and that doctors have a lower level than nurses (8, 10).
Gloves do not provide a secure barrier against the transmission of micro-organisms during surgery as they are vulnerable to perforation, which can be microscopic (11). When double gloving, holes may be more easily detected in the outer glove than the inner glove (12). Surgical hand preparation is just as important when double gloving.
The choice of the surgical hand preparation method appears to make no difference to the incidence of surgical site infections (13), but surgical hand antisepsis is less irritating to the skin than hand washing. Antiseptic solution is more effective than antimicrobial soap and water for reducing bacteria counts and bacteria growth on the hands (1, 14–16).
Studies focusing on adherence to the World Health Organization (WHO) guidelines on surgical hand preparation show that less than the recommended length of time is spent. The average time spent by surgeons was lower than that spent by scrub nurses (10, 17). Another study showed that 22% followed the recommended length of time for surgical hand washing, and 68% used the correct technique (18).
Schwartz et al. found that 12% carried out surgical hand antisepsis correctly in relation to the recommended technique, and 31% carried out the surgical hand washing procedure correctly (19). These findings indicate wide variation in adherence to the recommended times and techniques, and there is a measurable difference between occupational groups.
Surgical hand preparation prior to sterile procedures is to be carried out in accordance with NIPH guidelines (5). Knowledge about hygienic principles and aseptic technique is a key area of responsibility in scrub nursing (20), which also has a legislative basis (21). Scrub nurses are to maintain patient safety and contribute to a professional standard of care (22).
Objective of the study
The objective of the study was to examine existing practice, highlight the need for areas of improvement and focus attention on the importance of surgical hand preparation.
To find out whether scrub nurses and surgeons practise surgical hand preparation according to the guidelines, we asked the following research questions:
- How many members of the surgical team use surgical hand antisepsis as a method compared to those who use hand washing?
- Do the surgical team members spend the recommended length of time on surgical hand preparation?
- Is the correct technique used for each of the steps in surgical hand preparation?
- Are the guidelines for surgical hand preparation adhered to with regard to both the time spent and technique used?
The study is based on the following hypothesis: that there is a satisfactory level of adherence to recommended surgical hand preparation practice.
Method
Design
We conducted a cross-sectional study using systematic field observation in the participants’ normal working environment. A descriptive design approach was adopted as observation studies aim to observe, describe and record phenomena as they unfold (23).
Context and participants
The study was carried out at a university hospital in Norway over seven days during the period November–December 2021. The NIPH guidelines for surgical hand antisepsis and hand washing were on display at each hand-wash station.
We carried out stratified random sampling in which the participants were divided into two different strata based on the categorical variable of occupation: scrub nurses and surgeons. The sample was random, based on who was on duty during the observations. We excluded students and emergency surgery.
Data collection and measurement instrument
Data collection was carried out openly through systematic observations. The participants were informed that observations were being conducted. Direct observation is the most accurate method for examining the adherence of healthcare personnel to the guidelines for surgical hand preparation (24, 25).
The observations were selected from a digital surgery schedule. The first and second authors carried out data collection using an observation form drawn up on the basis of the NIPH guidelines for surgical hand preparation. The observation form contained variables for both surgical hand antisepsis using alcohol with added chlorhexidine and surgical hand washing using antimicrobial soap, containing chlorhexidine or iodine (5).
The reliability of the observation form was tested beforehand to ensure that it gave the same result with repeated assessments under the same conditions (26). The form was tested by the observers, both on each other and on two scrub nurses in the department where data collection was to be carried out. These observations were not included in the study.
We collected information on the following variables: occupation, sex, choice of method, time spent and technique used. A stopwatch was used for recording time taken. Technique was registered as either carried out or not carried out, in the form of yes/no responses to each of the steps. We registered whether participants had been observed on multiple occasions because it could affect the results. The observations were recorded on an ongoing basis on paper observation forms.
Analysis
We analysed the data using Stata/SE 17.0 because this software was suited to taking into account whether some participants had been observed on more than one occasion. Each individual was treated as one cluster and is presented in the number of participants in each analysis. A cluster robust estimation of standard errors took into account that repeated observations of the same individual were correlated. The observers interpreted the data in collaboration with a statistician.
The analyses included hypothesis testing in the form of regression analysis. The following null hypothesis formed the basis for statistical hypothesis tests:
‘There is no difference between scrub nurses and surgeons in adherence to surgical hand preparation practice.’
We used logistic regression analysis for dichotomous variables (yes/no) and Poisson regression for the continuous variable (time). Descriptive statistics (frequency, percentage) were used for categoric variables (occupation, sex, method), dichotomous variables and continuous variables. The mean and the standard deviation (SD) describe the distribution of the continuous variables. The mean also represents the measure of central tendency for time.
We used inferential statistics to compare groups, with a 95% confidence interval (CI). Some of the results are presented as an estimated odds ratio (OR). OR is used to compare groups and estimate differences. Further on, the analysis model estimates the probability of an outcome (23, 27). In relation to the analyses that examined differences in length of time spent by each of the groups, we used ratio of means (RoM). The significance level was set to p-value < 0.05 (5%).
Ethical considerations
The study was approved by the data protection officer at the hospital in question (ID number 2723). The managers and potential participants received information via email, and the lack of a reply was regarded as a sign of informed consent. We did not collect signed consent forms from each individual because a request immediately prior to observation could have affected the results.
Participation was voluntary and the participants were free to withdraw from the study at any time. The collected data would then be deleted in accordance with Chapter 2, Article 7 of the Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 (28).
In the study, we collected data that was de-identified after registration in an ID number access control list. During data analysis, we only used ID numbers and occupations. We registered the number of observations per participant because this could affect the result. The list was treated strictly confidentially in line with the General Data Protection Regulation and research ethics guidelines point 5 on confidentiality (29).
On completion of the project, the access control list was deleted in line with the guidelines.
Results
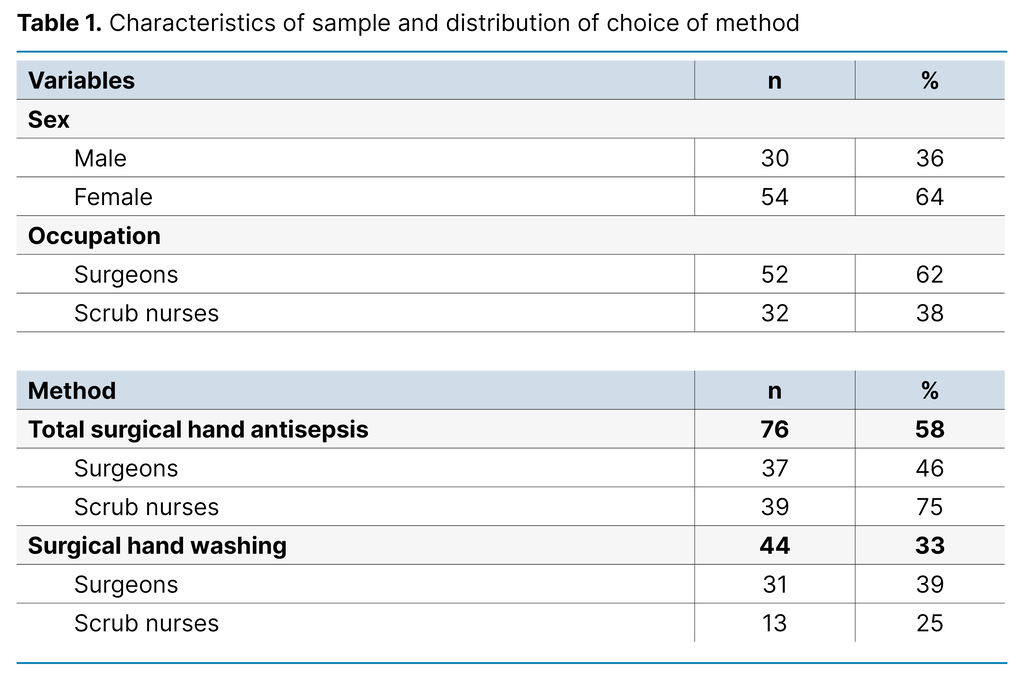
We carried out 132 systematic observations of 84 individual participants, of whom 62% were observed on one occasion only. One participant chose to withdraw from the study. All of the scrub nurses involved were women. A minority of the surgeons, 9% (n = 12), carried out a combination of surgical hand antisepsis and hand washing. They were excluded from the analyses. Table 1 shows how the choice of method for surgical hand preparation was distributed across participants.
Time
The recommended guidelines estimate that surgical hand antisepsis should take 120 seconds to carry out. We conducted 76 observations of 50 individual participants. Only 26% (CI 15–38) spent the recommended length of time on surgical hand antisepsis. The estimated mean time was 90 seconds (SD 55, CI 74–105).
The surgeons spent an estimated average of 66 seconds (SD 36, CI 54–77). The registered time varied from 0 to 150 seconds. The scrub nurses spent an estimated average of 112 seconds (SD 61, CI 89–136). The registered time varied from 32 to 293 seconds. The scrub nurses spent 71% more time than the surgeons (RoM = 1.71; CI 1.35–2.17). There was a difference between the occupational groups (p < 0.001).
The recommended guidelines estimate that surgical hand washing should take 240 seconds to carry out. We conducted 44 observations of 23 individual participants. The recommended length of time for surgical hand washing was followed by 34% (CI 17–51). The estimated mean time was 209 seconds (SD 100, CI 171–247).
The surgeons spent an estimated average of 190 seconds (SD 84, CI 159–220). The registered time varied from 20 to 363 seconds. The scrub nurses spent an estimated average of 256 seconds (SD 124, CI 172–340). The registered time varied from 50 to 449 seconds.
The scrub nurses spent 35% more time than the surgeons (RoM = 1.35; CI 0.95–1.90). There was no difference between the occupational groups (p = 0.090).
Technique
Figure 1 shows the level of adherence to each step in the NIPH guidelines for surgical hand antisepsis (5). The correct technique was used by 21% (n = 16) (CI 11–31). A total of 57% did not dip the fingertips of their opposite hand in the antiseptic solution, 45% did not splay their fingers and rub the back of their hands, 68% did not rub the backs of their fingers from side to side, 28% did not rub their thumbs using a rotating movement, and 34% did not repeat the steps.
The estimated probability of carrying out the correct technique was 3% (CI 0–8) for the surgeons and 38% (CI 21–56) for the scrub nurses. The odds of carrying out the technique correctly were 23 times higher for the scrub nurses compared to the surgeons (OR = 22.5; CI 2.6–196). There was a difference between the occupational groups (p= 0.005).
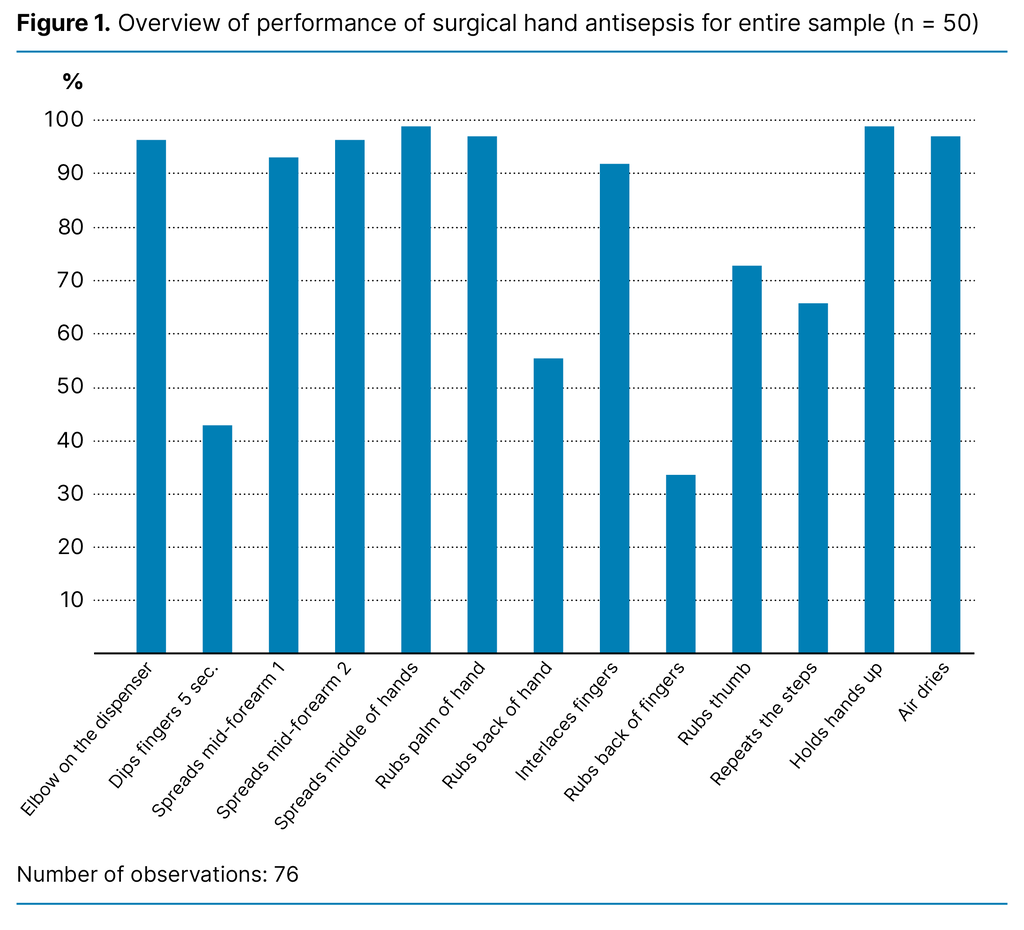
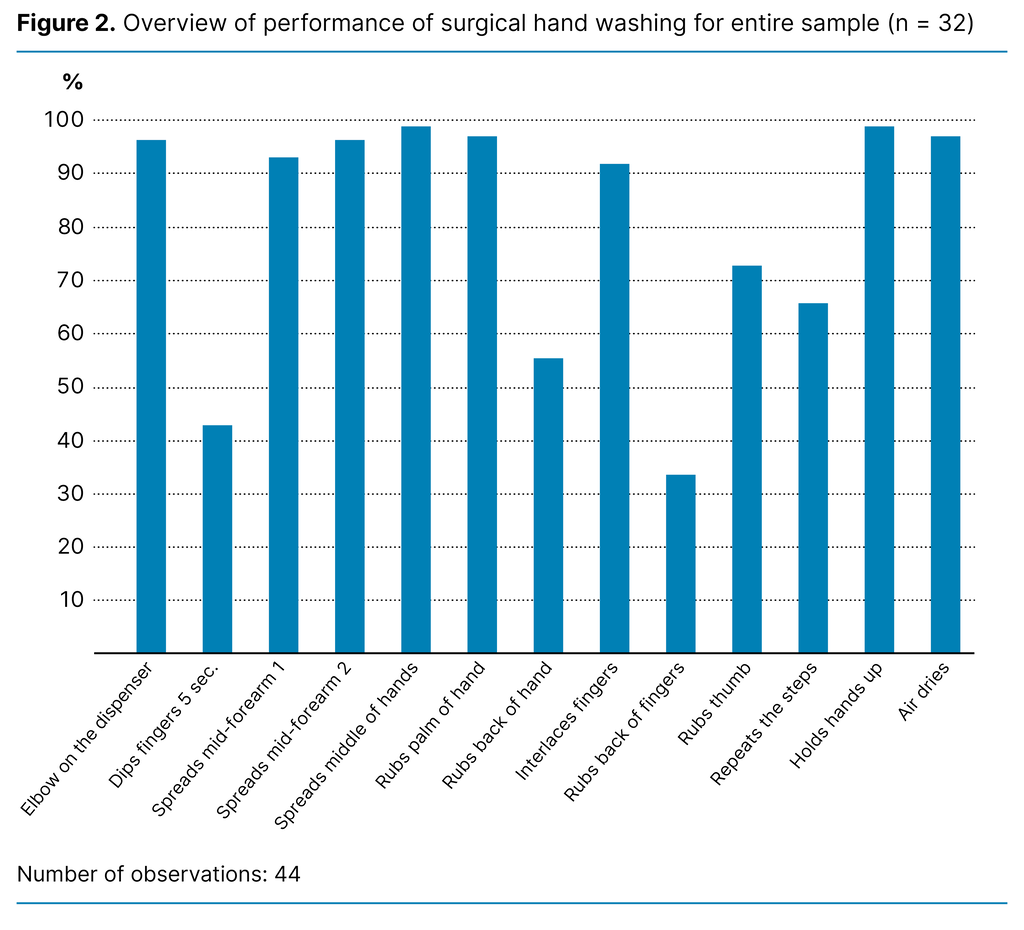
Figure 2 shows the level of adherence to each step in the NIPH guidelines for surgical hand washing (5). The correct technique was used by 34% (n = 15) (CI 20–49). Nail brushes are only used when necessary and were not included in the technique assessment. According to the results, 39% did not splay their fingers and rub the back of their hands, 48% did not rub the backs of their fingers from side to side, 18% did not rub their thumbs using a rotating movement, and 14% did not wash their forearms.
The estimated probability of carrying out the correct technique for surgical hand washing was 26% (CI 9–49) for the surgeons and 54% (CI 31–77) for the scrub nurses. The odds of carrying out the technique correctly were 3 times higher for the scrub nurses in our sample (OR = 3.35; CI 0.9–12), but there are wide confidence intervals and there is no significant difference between the occupational groups (p = 0.059).
Is surgical hand preparation carried out in accordance with the guidelines in terms of time spent and technique used?
The estimated probability of adhering to the guidelines for surgical hand antisepsis was 3% for the surgeons (CI 0–8). For the scrub nurses, the estimated probability of adhering to the guidelines was 20% (CI 7–34). The odds of carrying out the technique correctly were 9 times higher for the scrub nurses compared to the surgeons (OR = 9.3; CI 1–84). There was a difference between the occupational groups (p= 0.047).
The estimated probability of adhering to the guidelines for surgical hand washing was 19% for the surgeons (CI 4–34). For the scrub nurses, the estimated probability of adhering to the guidelines was 23% (CI 7–39). The odds of adhering to the guidelines were 25% higher for the scrub nurses in our sample compared to the surgeons (OR = 1.25; CI 0.4–4), but with wide confidence intervals and no difference between the occupational groups (p = 0.712).
It was not possible to compare the sexes among the scrub nurses as there were only female participants. Among the surgeons, it was only possible to compare the sexes in relation to surgical hand washing. There was no statistically significant difference in this regard between the surgeons of different sexes (p = 0.100).
Discussion
The objective of the study was to examine whether surgical hand preparation is carried out according the NIPH guidelines. The results showed a low level of adherence to these guidelines.
Choice of method for surgical hand preparation
The NIPH guidelines recommend surgical hand antisepsis as the first choice for surgical hand preparation (5). In our study, 75% of the scrub nurses and 46% of the surgeons chose surgical hand antisepsis, while 25% of the scrub nurses and 39% of the surgeons chose surgical hand washing. Our findings correspond with the results of Schwartz et al. (19), in which the majority (68%) chose surgical hand antisepsis.
We could not find any research examining the choices of the occupational groups. Scrub nurses and surgeons in Norway are trained according to the NIPH guidelines (5), but the reason why surgeons chose surgical hand washing more often may be due to previous training and force of habit.
Surgical hand washing is an older and more established procedure, and newly qualified surgeons may be influenced in their choice of method if they learn this procedure from more experienced surgeons. This may also be a matter of preference because surgical hand antisepsis can leave your hands feeling sticky when dressing under sterile conditions. After surgical hand washing, hands are dried with sterile paper, which simplifies the process of putting on sterile gloves.
Time spent on surgical hand preparation
The results showed that 26% adhered to the recommended length of time for surgical hand antisepsis, and 34% for surgical hand washing, which corresponds with previous research on WHO’s recommendations (10, 18).
In our study, the average time spent on surgical hand antisepsis was 90 seconds. The recommended time is 120 seconds. There is a difference between the occupations: scrub nurses carried out the procedure for 46 seconds longer than the surgeons. The findings correspond with the results of Laurikainen et al.’s study (10).
The average time spent on surgical hand washing was 209 seconds. The recommended time is 240 seconds. We did not find a statistical difference between the occupations; however, the scrub nurses spent more time on the procedure than the surgeons. The number of observations of scrub nurses was so low that we consider the result uncertain.
Our study does not reveal the reason for the small amount of time spent, but research shows that attitudes to infection control, eczema and hand sores can affect the length of time spent (10). Other reasons might be a lack of knowledge and skills regarding correct practice (17, 18).
Simulation exercises and skills training in order to observe and raise awareness about how long the procedure takes may improve the standard. Furthermore, knowledge about the consequences may increase adherence, even though it is difficult to determine the extent to which it affects the incidence of surgical site infections. Incorrect surgical hand preparation and perforations in surgical gloves are just two of several factors that can result in surgical site infections.
If surgical hand preparation is carried out randomly and unsystematically, using the correct length of time is no guarantee for clean hands. Pan et al. found that even if healthcare personnel spent more time on hand preparation, certain areas on the hands were repeatedly omitted (30). If areas on the hands and forearms are not washed or disinfected thoroughly enough during surgical hand preparation, pathogenic micro-organisms may remain. We believe that training in the correct technique for surgical hand preparation will make it easier to follow the recommended time.
Practising the correct technique for surgical hand preparation
We found somewhat better adherence to the correct technique for surgical hand washing (34%) than for surgical antisepsis (21%). Schwartz et al. (19) also found that there were more participants that used the correct technique for surgical hand washing (31%) than for surgical antisepsis (12%).
When we compared techniques, the same areas were omitted in the case of both surgical hand antisepsis and hand washing. Common mistakes were that participants failed to splay their fingers and rub the backs of their hands, rub their fingers from side to side and rub their thumbs. In the case of surgical hand antisepsis, it was also relatively common to fail to dip the fingertips of the opposite hand in antiseptic solution. When observing surgical hand washing, there was a small percentage who did not wash their forearms. Similar results have been found in recent research (9), in which 47% of the participants did not wash their forearms according to the correct procedure.
Our study shows a difference between the occupational groups in relation to using the correct technique for surgical hand antisepsis, but not for surgical hand washing. Previous research also indicates an association between doctors and men and lower levels of adherence to both general and surgical hand preparation (8, 10). The reasons could be differences in educational programmes, work flows and workloads. Scrub nurses are to carry out infection prevention measures directly related to equipment, patients and personnel (20). Healthcare personnel have a duty to follow the guidelines, as well as to implement and comply with correct infection control measures (21).
Personnel with long experience have probably learned different techniques due to changes in practices and guidelines over time. The extent to which training and implementation of new guidelines are adequate may be another reason for variation in different techniques. We see that there may be a need to involve all occupational groups in order to improve practices, with a view to lasting change.
Adherence to recommended times and techniques for surgical hand preparation
The results show that there was a low level of adherence to the guidelines in regard to both surgical hand antisepsis and hand washing at the hospital in question. There was also a difference between the occupational groups in relation to surgical hand antisepsis, but not for surgical hand washing. The results of the study may have been influenced by the Hawthorne effect (23). Therefore, we had expected better results, as the participants knew that observations of surgical hand preparation were being conducted.
Gloves cannot be considered a secure physical barrier as microscopic perforations before and during use can result in the transmission of micro-organisms (11). Undetected perforations can increase the risk of transmission of infection. It is necessary that the surgical team knows this in order to understand the importance of surgical hand preparation as an infection prevention measure. By carrying out surgical hand preparation in accordance with the guidelines, healthcare personnel can help to maintain patient safety and prevent surgical site infections.
Strengths and weaknesses of the study
A strength of the study is that we present a comprehensive assessment of surgical hand preparation. Previous research has either assessed surgical hand antisepsis or surgical hand washing, and time spent or technique used, whereas we surveyed time spent and technique used in relation to both methods.
The sample was representative as we took a random sample of the population. We intentionally did not collect data on surgical specialties to protect the anonymity of the participants. The observation form was tested several times beforehand. During the observations, we attempted to maintain a distance from the subject to reduce researcher influence as much as possible.
We carried out the analyses in collaboration with a statistician. We interpreted and described findings in collaboration. It is a strength that regression models were used to adjust the CI and p-value based on cluster data. Thus, the result was not affected by multiple observations of individual participants.
We carried out open and direct observations, in which the Hawthorne effect may have resulted in participants modifying their behaviour and performing differently under observation (23). The observers may also have observed and recorded observations somewhat differently. Bias may have occurred due to the simultaneous demands of filling in the form and timekeeping.
A weakness of the cross-sectional study is that it does not examine causal relationships. Therefore, we cannot explain why the occupational groups adhered to the procedures differently, or why one particular method was preferred to the other. During the observations, both surgeons and doctors undergoing specialisation were monitored in the same group. We could not register this as we did not want to communicate with the participants. If we had registered this, experience may have been considered as an explanatory factor.
The study has a relatively small sample, which may cause statistical uncertainty. We also had a disproportionate sample, in which surgeons were overrepresented. The reason for this was that for each operation we observed, there were usually two surgeons and one scrub nurse who carried out surgical hand preparation.
Conclusion
The study shows that there was a low level of adherence to recommended surgical hand preparation practice. Scrub nurses had a higher probability than surgeons of following the recommended time and technique in relation to both methods.
We did not examine the reasons for the low level of adherence, but training, implementation, knowledge and time constraints can impact on correct practice. A joint understanding of the guidelines through thorough training could contribute to improved adherence. Surgical hand preparation is an inexpensive, quick and easy measure to combat surgical site infections.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge


Comments