Managers’ views on the need for advanced nursing competence in the changing home nursing service
Summary
Background: The Coordination Reform has created a need for change in the home nursing service in Norway. More patients are now receiving medical care and follow-up in their own homes. The number of older and younger patients with various diagnoses and health challenges who require home nursing care is growing. Managers in the primary care service are responsible for ensuring that patients living at home receive the required standard of care. They must ensure that home care nurses have the necessary competence so that patients of all ages with complex care needs can manage daily life in their own homes.
Objective: The aim of the study was to explore what nursing competence managers in the health and care service believe is needed in order to provide care and support to patients living at home with complex needs.
Method: The study employed a qualitative approach. Five focus group interviews were held with 24 managers and middle managers in the primary care service in three urban municipalities in Northern Norway during the autumn of 2022 and spring of 2023. The analysis was based on Malterud’s systematic text condensation method.
Results: We identified three main themes: 1) Caring for seriously ill patients of all ages living at home increases the need for advanced nursing competence, 2) Nurses need more than just general clinical competence, and 3) A greater need for responsibility and task allocation in home nursing care.
Conclusion: The managers and middle managers found that patient groups of all ages with complex and multifaceted health conditions require more advanced medical-technical assistance and care in their own homes. They recognise the value of home care nurses having an Advanced Clinical Practice (ACP) qualification when assessing patient needs and allocating tasks. The manager groups emphasised their responsibility to ensure that home care nurses have the opportunity to study for an advanced qualification and specialist education across a range of medical and nursing fields. Further research on managers, middle managers and nurses in home nursing care in other urban municipalities in Norway is needed to explore competency needs and how other local authorities organise their home nursing service.
Cite the article
Halland A, Holand T, Mæhre K. Managers’ views on the need for advanced nursing competence in the changing home nursing service. Sykepleien Forskning. 2025;20(99102):e-99102. DOI: 10.4220/Sykepleienf.2025.99102en
Introduction
The Norwegian Institute of Public Health (NIPH) points out that the competency requirement for managing younger patient groups with psychiatric, somatic or neurological illnesses has changed (1). The Health and Care Services Act determines the framework and content of these services (2).
The Coordination Reform (3) and the Quality Reform for Older Patients (4) have led to a change in local authorities’ scope of responsibility in the health and care service. The primary care service is now responsible for prevention, early intervention, treatment and rehabilitation (3).
The National Audit Office of Norway’s report from 2016 highlighted how patients are discharged earlier from hospitals following the Coordination Reform. Patients receiving home nursing care are more seriously ill than before. There is a lack of competence in the health and care service, and quality targets are not being met (5). The specialist health service expects patients ready for discharge to receive advanced medical care in their own homes (6, 7).
Home care nurses encounter patients with complex needs of all ages, often with multimorbidity (8–10). Multimorbidity leads to reduced quality of life, functional impairment, polypharmacy, increased mortality, longer treatment times and more frequent unplanned medical care (9, 11).
Studies show that higher demands are being placed on home care nurses’ professional competence (12–14). Studies also highlight the growing responsibilities of managers in home nursing care (15), including for prioritising resources (16) and ensuring that nurses have the necessary competence to provide the required standard of medical care to this patient group (15, 17–19).
In our understanding of the concept of competence, we have drawn on Lai (20), who states that competence is the sum of knowledge, skills and attitudes. According to Benner (21), it can take two to three years for a nurse to become a competent and skilled practitioner.
By 2030, an increased demand for advanced medical competence in primary care is expected (10). Today’s nurses must be able to provide advanced medical care such as home dialysis, respiratory therapy, intravenous treatment and pain relief, as well as carry out advanced health assessments and palliative care in patients’ homes (22–24). As early as 2018, researchers found that nurses are often faced with tasks for which they are insufficiently trained (24).
Managers are responsible for safeguarding standards in the health and care service. This means they must ensure that nurses have the necessary competence, resources and tools to manage the challenges they will face.
Objective of the study
The objective of the study was to identify the competencies that managers in the health and care service believe nurses need in order to provide care and support to patients living at home with complex needs.
Method
The study has a qualitative design. Qualitative methods are well-suited for obtaining in-depth knowledge about participants’ experiences with and perceptions of a specific topic (25).
We conducted five focus group interviews with managers and middle managers in three urban municipalities in Northern Norway. Our preunderstanding was that these local authorities organise their home nursing services in a similar way and may have the same competency needs. Focus group interviews are an effective method for fostering dialogue among participants, shedding light on different experiences and revealing areas of agreement and disagreement (25).
Recruitment and selection
We recruited health and care managers from three urban municipalities in Northern Norway. A and B are medium-sized municipalities and C is a large municipality. In the article, the senior managers responsible for health services in home nursing care are referred to as ‘managers’. Unit managers and departmental managers are referred to as ‘middle managers’.
The managers of the home nursing service were contacted and informed about the project by the last author, who was the project manager. These managers provided names of managers and middle managers that the project manager could contact via email. Information letters and consent forms were attached to the email. Three managers declined and 24 agreed to take part in the focus group interviews.
Two focus group interviews (A1 and A2) were held in municipality A, one (B1) was held in municipality B and two (C1 and C2) in municipality C. Most of the interviewees were nurses. The focus group interviews were conducted in the autumn of 2022 and the spring of 2023.
Focus group interviews
We used a voice recorder app and informed the participants about this in advance. The interviews lasted between 60 and 90 minutes. The last author acted as moderator and guided the participants’ conversation, while the other authors served as secretaries, taking field notes and observing the interaction between participants. The moderator used a semi-structured interview guide inspired by Krueger and Casey (26).
We developed the interview guide ourselves. It was not followed in chronological order but served as a starting point and a background for the interviews.
Analysis
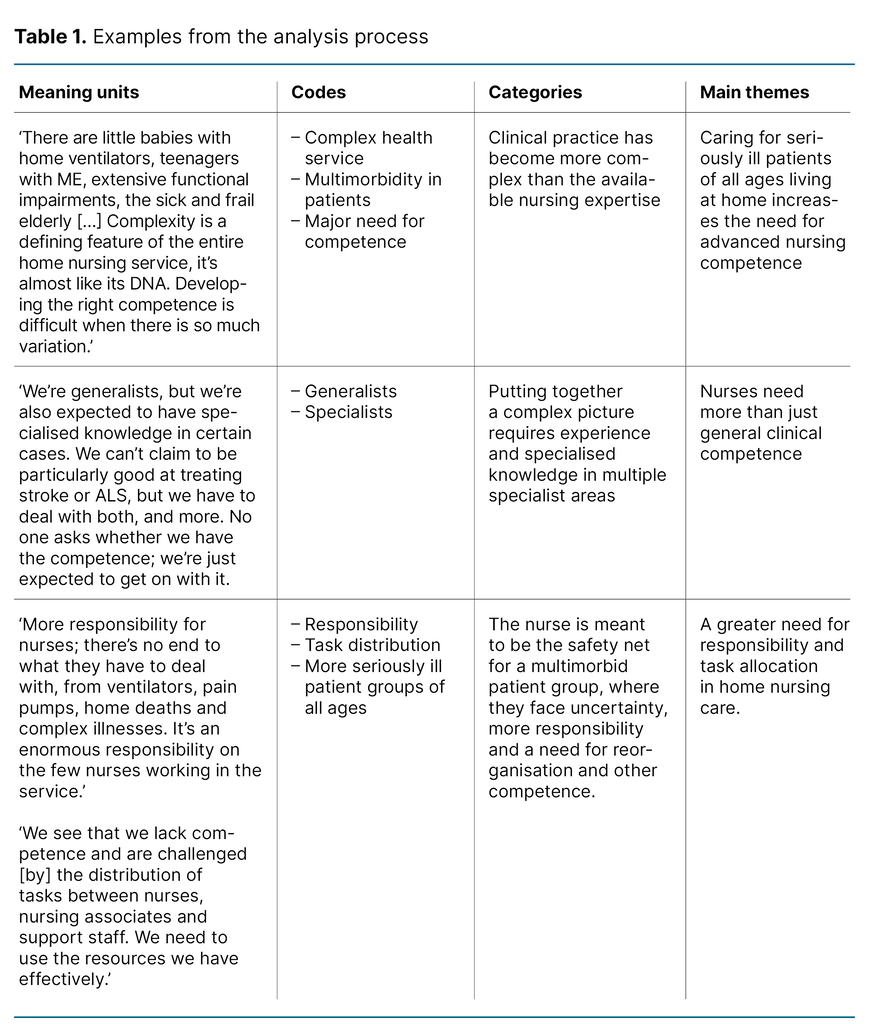
The analysis of the focus group interviews is based on Malterud’s systematic text condensation (27), a method for cross-case thematic analysis of qualitative data, in which the analysis process can be divided into four steps (Table 1).
In the first step, we read the transcribed material individually and then together to gain an overall impression and identify preliminary themes. In the second step, meaning units were identified and grouped into codes, with the content reduced into condensates that included ‘golden quotes’ from the data material. In the third step, we developed code groups by transforming the meaning units from step two into categories. In the fourth and final step, we summarised the findings based on the categories, which resulted in three main themes.
Research ethics considerations
The study was reported to Sikt – the Norwegian Agency for Shared Services in Education and Research (reference number 552291). The informants received an information letter and consent form. We obtained written informed consent prior to the focus group interviews.
Participants were informed of their right to withdraw their consent at any time during the study without giving a reason and without any repercussions. The managers had various job titles but are referred to in the article as ‘managers’ and ‘middle managers’ in order to protect their anonymity.
Results
We identified three main themes: 1) Caring for seriously ill patients of all ages living at home increases the need for advanced nursing competence, 2) Nurses need more than just general clinical competence, and 3) A greater need for responsibility and task allocation in home nursing care.
Caring for seriously ill patients of all ages living at home increases the need for advanced nursing competence
Participants found that home care nurses are having to manage and provide care for more seriously ill patients in all age groups and that they lack competence in many areas. The patient group ranges from small infants to older individuals with complex needs, requiring nurses to have medical-technical competence. A manager in a medium-sized municipality stated the following:
‘There are little babies with home ventilators, teenagers with ME, extensive functional impairments, the sick and frail elderly […] Complexity is a defining feature of the entire home nursing service, it’s almost like its DNA. Developing the right competence is difficult when there is so much variation.’ (B1)
Participants emphasised the importance of understanding what individual patients with physical and mental illnesses need in terms of comprehensive care. A middle manager in a medium-sized municipality expressed it as follows:
‘In mental health care, you need to understand the whole picture for each patient, not get caught up in diagnoses and procedures, as often happens in somatic care.’ (A2)
Managers in the medium-sized municipalities expressed concern that a growing patient group with serious somatic and mental health problems of all age groups is not receiving comprehensive care and support. One manager said the following:
‘We encounter all these patients with different challenges, including in mental health, so what can we do, because everyone deserves good health care.’ (A1)
Some of the participants focussed on the importance of nurses having the competence to assess what the individual patient needs in terms of physical and mental health support.
A middle manager in a large municipality explained it as follows:
‘Patients are forced to care for themselves, a hidden challenge that isn’t talked about much. These are the major long-term challenges we face.’ (C2)
When nurses lack the competence to carry out a comprehensive assessment of the patient’s situation, this also represents a challenge for the managers.
Nurses need more than just general clinical competence
Many of the managers and middle managers pointed out that nurses need skills beyond general clinical competence if they are to provide healthcare services for patients with complex medical conditions. This requires a higher level of education than a bachelor’s degree. A manager in a large municipality explained it as follows:
‘We’re generalists, but we’re also expected to have specialised knowledge in certain cases. We can’t claim to be particularly good at treating stroke or ALS, but we have to deal with both, and more. No one asks whether we have the competence; we’re just expected to get on with it.’ (C1)
The participants found that it takes time for newly qualified nurses to develop clinical judgement and to be able to take responsibility for patients with complex needs. The managers in the largest municipality emphasised the importance of the Advanced Clinical Practice (ACP) qualification. One manager said the following:
‘Observation skills, especially for patients with dementia and in palliative care, require more than just taking measurements. It’s about identifying the tools you need to make the right observations. The ACP training has its advantages, we learn how to carry out a full patient assessment and piece it all together into a holistic picture. I don’t know if you can do that as a novice. You need experience and an in-depth understanding.’ (C2)
The interviews revealed that patients discharged from hospital with complex wounds and seriously ill cancer patients need palliative care and support. There was a shortage of oncology nurses and nurses with expertise in palliative care. The managers with an ACP qualification in the large municipality highlighted the benefits of both them and the nurses having this advanced training.
A greater need for responsibility and task allocation in home nursing care
The managers and middle managers in all the municipalities were concerned that they were placing too much responsibility on newly qualified nurses in terms of patient follow-up. A manager in a medium-sized municipality said the following:
‘The nurse in charge has considerable responsibility; you need to know what to do if you’re assigned that role. We’ve faced some challenges with our own staff, particularly the newly qualified nurses, in terms of taking ownership of this role.’ (A1)
The managers in the medium-sized municipalities in particular found that the health service lacked resources and nursing expertise. A middle manager expressed it as follows:
‘We see that we lack competence and are challenged [by] the distribution of tasks between nurses, nursing associates and support staff. We need to use the resources we have effectively.’ (B1)
The transfer of responsibilities from the specialist health service to primary care has increased the demand for expertise, which takes time to acquire. One of the managers in a medium-sized municipality stated the following:
‘We lack the competence to take patients from the specialist health service. Nurses are worried about not being able to cope with […] the medical follow-up [...] Multimorbidity and complex needs are being shifted from the specialist health service to primary care. They should stay in hospital longer.’ (A2)
The participants all agreed that patients with complex needs are discharged too early from the specialist health service to their homes and before completing their treatment. The unmet demand for competence means that nurses are faced with a huge responsibility to provide the required standard of care for this patient group. The managers in the largest municipality were concerned about the responsibility they place on nurses:
‘More responsibility for nurses; there’s no end to what they have to deal with, from ventilators, pain pumps, home deaths and complex illnesses. It’s an enormous responsibility on the few nurses working in the service.’ (C1)
Several managers emphasised their responsibility to coordinate and assess the patient’s complex needs for care, and that this also requires managers to have the experience and competence to allocate tasks effectively.
A manager in a large municipality stated: ‘As a manager, you also need to have the ability to see things from a coordination perspective, to identify and possess the expertise to assess the complexity. You need to be good at a lot of things in the home nursing service.’ (C2)
Since the Coordination Reform, several informants have found that the responsibility for ensuring that the required standard of care is provided in their municipality has become greater. The pressure on nursing resources is considerable, and more specialised nursing competence is needed. The managers therefore believe it is necessary to redistribute responsibilities and tasks. In the largest municipality, the managers had taken more decisive steps and reorganised the home nursing service and the division of tasks. This made it easier to recruit and retain nurses.
Discussion
The objective of this article was to examine the experiences of managers and middle managers in home nursing care regarding the need for nursing competence. Following implementation of the Coordination Reform, patients are now discharged earlier and have more extensive care needs (1).
In line with government white papers (3) and other studies (12, 18, 28, 29), our study shows that home care nurses are required to care for not only older and multimorbid patients, but also younger patients in various life situations and with a wide range of diagnoses, all receiving care in their own homes.
Nurses need expertise in multiple specialist areas to care for patients with complex medical needs
In addition to our study, several other studies (8, 19, 28, 29) show that home care nurses lack medical and nursing competence. Several managers and middle managers in our study were concerned that the necessary expertise was lacking in many specialist areas.
The managers were aware that they are not only financially responsible for running the home nursing service, but also for ensuring that patients receive the care they need. This includes making sure that nurses have the necessary competence to provide the required standard of care.
The specialist health service expects home care nurses to handle complex medical challenges and advanced medical-technical tasks after patients are discharged from hospital (6). Participants in our study found that nurses can feel unsure when required to perform unfamiliar and advanced medical procedures, and this is also reflected in other studies (22–24, 31).
Our study also revealed that nurses had problems dealing with advanced medical-technical equipment, such as home ventilators. Several middle managers pointed out that nurses with more clinical experience in home nursing care are better equipped to handle such challenges, which aligns with Benner’s (21) description of the five stages of clinical competence.
As in our study, other studies (12–14, 18, 22) have also noted that nurses must have the expertise to provide comprehensive care in areas such as psychiatry, palliative care, geriatric care and care for individuals with intellectual disabilities. Our study also highlighted a need for competence in caring for the youngest patient groups with complex needs.
The managers and middle managers believed it was challenging for nurses to take a comprehensive view of the patient’s needs and assess what each patient requires in terms of physical and mental support. When patients do not receive the medical care they need, they are forced to take responsibility for their own health and illness.
The managers and middle managers believe that the nurses need skills beyond general clinical competence
The bachelor’s degree in nursing gives nurses general clinical competence (32). In the study, we asked managers and middle managers what type of nursing competence they believe is needed in home nursing care. Other studies (15, 17) have also identified a need for a higher level of competence in recognising patient deterioration and assessing nursing interventions for patients living at home.
The participants in our study pointed out that specialised nursing skills are needed to carry out systematic clinical examinations and assessments, make decisions and implement nursing interventions for patients with complex needs. Our findings show that home care nurses need more advanced knowledge than that provided by a bachelor’s degree in nursing (21, 32). Newly qualified nurses have little clinical experience.
Having responsibility for patients with complex needs is challenging in a home nursing context, where nurses are often alone in bearing that responsibility. Previous studies (23, 33, 34) highlight the need for home care nurses to have an Advanced Clinical Practice (ACP) qualification. As part of their training, ACP nurses develop advanced clinical expertise and strong decision-making skills, enabling them to deliver the required standard of care for different patient groups in all age groups facing a wide range of health challenges (7).
According to Lai (20) and Benner et al. (21), changes in the condition of patients with complex needs require expert-level knowledge, skills and personal qualities in order for nurses to deliver comprehensive care – and these take time to develop.
A surprise finding in our study was that managers with an ACP qualification – all from the largest urban municipality – reported that their advanced training had given them a deeper understanding of the areas where nurses may lack competence. They had also become more aware of their responsibility as managers for building competence and organising health services, as outlined in the regulations on leadership and quality improvement in the health and care service (30).
We observed a change in the managers during the focus group interviews, from being primarily concerned with finances to focussing on their responsibility for ensuring that the required standard of care is provided. They recognised the need for nurses to have the opportunity to study for an advanced qualification and specialist education across a range of medical and nursing fields.
Advanced nursing competence can also make it easier to assess complexity and implement the necessary nursing interventions for patients with complex needs. Maintaining and acquiring new competence may also help retain nurses in home nursing care. Insufficient competence can pose a threat to patient safety – something the managers in our study were concerned about.
The responsibilities and division of tasks in home nursing care are changing
As part of the Coordination Reform, nurses were assigned greater responsibility (3) for patients of all ages with somatic and psychosomatic conditions. This means that managers and middle managers, who have overall clinical responsibility, must ensure an effective distribution of tasks (30) and adapt to changes in the health service (15–17). Our study shows a need for a more specialised division of responsibilities and tasks in home care services, where nurses are assigned nursing duties that match their qualifications and cannot be delegated.
As with our study, other studies (14) also show that home care nurses often have sole responsibility for a wide range of tasks in patients’ homes. These nurses must have wide-ranging clinical competence, enabling them to provide care regardless of diagnosis or context. Other studies (35) point to a gap between what older patients with complex needs require and what the health and care service can provide.
In our study, participants expressed concern about whether they will be able to coordinate and provide home-based patients with complex needs the care they require when there is lack of nursing competence. This issue was more pronounced in the medium-sized municipalities. The managers further pointed out that the problem goes beyond a mere lack of resources; healthcare personnel and resources must be deployed effectively, in the right place at the right time. This requires a redistribution of responsibilities and tasks and a reorganisation of the service.
In another study (2), nurses reported that they were not using their expertise and were instead assigned tasks that less qualified healthcare personnel could carry out. Our study found that recruiting and retaining nurses is a challenge, although it appears to be easier in the largest municipality.
The managers in our study did not have specific suggestions for how the division of tasks could be addressed, and more research is needed on this. However, several of the managers and middle managers felt there was a need to reorganise the home nursing service. The largest municipality was more focussed on digital solutions to address the resource challenges in the service.
Nurses are needed who have a higher level of education than a bachelor’s degree. They must be offered advanced training to enhance their skills in providing health and care services for patients with complex needs.
Raising competence levels in home nursing care will be an expense in local authorities’ health and care budget. However, in the longer term, operating costs for health and care services for home-based patient groups will likely decrease when nurses have attained the necessary medical and nursing expertise.
Strengths and limitations of the study
When focus groups include managers and middle managers from different levels, participants can be reluctant to discuss difficult or controversial issues. In our study, the dialogue was good between the different management groups. However, after one of the interviews, one of the middle managers disagreed with the managers’ solutions to the nursing competence challenges, something they had not expressed during the focus group interview.
Participants found it beneficial to meet and discuss the competence needs in home nursing care. Conducting focus group interviews with management groups who had responsibility for the health and care service in three Northern Norwegian municipalities was a strength of the study. We believe that a group of participants with a management perspective can reveal different insights into the need for advanced nursing competence than a group of home care nurses.
Another strength of the study is that managers and middle managers participated in the same focus group to discuss the competencies nurses need to care for patients living at home with complex needs. We have extensive experience in primary care and in research in this field. We have therefore been careful to ensure that our own preunderstanding did not influence the study. The limitation of the study is that we did not interview the home care nurses.
Conclusion
In managers’ and middle managers’ experience, patients of all ages with complex and multifaceted conditions require more advanced medical-technical assistance and care in their own homes. When nursing resources are scarce and nurses lack clinical experience and advanced training, patients may not receive the medical care they need. The managers recognise the benefit of a nurse having an ACP qualification when conducting a needs assessment and allocating tasks in the home nursing service.
During the focus group interviews, the management groups became aware of the need to strengthen nursing resources and competencies. They also need to ensure that home care nurses have the opportunity to enhance their competencies in several medical and nursing fields. Patient safety can be comprised when nurses do not have the necessary competence.
Further research involving managers, middle managers and nurses in the home nursing service in other urban municipalities in Norway is needed to explore competency needs and how other local authorities organise their home nursing service.
Acknowledgements
We would like to thank UiT The Arctic University of Norway and the management of the Department of Health and Care Sciences at UiT (IHO) for their financial support and the opportunity to conduct the study. We would also like to extend our thanks to the managers and middle managers who participated in the focus group interviews.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge

Comments