Nurses’ working conditions, patient safety and quality – a secondary analysis of cross-sectional data
Summary
Background: Highly qualified staff are crucial in hospitals to ensure efficient operations and patient safety. Ensuring access to qualified staff and maintaining a stable workforce are ongoing challenges. Two different international studies conducted in Europe adopted approaches developed during research in the United States, linked to Magnet hospitals, to develop knowledge about the management of nursing resources.
Objective: The article aims to compare responses regarding nurses’ daily work environment at Lovisenberg Diaconal Hospital in two studies dating from 2009 and 2021.
Method: The data collection included surveys of working conditions, well-being, patient safety and quality. We used questions from established measuring instruments such as the Nursing Work Index and the Maslach Burnout Inventory. Other questions covered patient safety and missed nursing care, as well as individual background variables. The responses from the two surveys were compared using descriptive statistics.
Results: In 2009, 168 (64%) of the nurses included responded to the survey, whereas in 2021, 218 nurses (83%) responded. The nurses described several working conditions more positively in 2021 compared to 2009, including relations with their immediate supervisor and staffing levels. The number of patients per nurse was lower in 2021. The frequency of missed nursing care remained much the same. One exception to this missed pain management, which was higher in 2021. The results in 2021 were more negative in regard to questions about whether the nurses would recommend the hospital to family and friends, the patient’s ability to cope after being discharged and general, ‘on the whole’ type questions regarding quality.
Conclusion: Although some specific working conditions for nurses at Lovisenberg Diaconal Hospital were described more positively in 2021 than in 2009, the general assessments show a slightly negative development. The study provides insight into the daily work environment at the hospital from a nursing perspective, but it has weaknesses in regard to method and sample size. The results cannot be generalised to other Norwegian hospitals.
Cite the article
Sjetne I, Lerdal A. Nurses’ working conditions, patient safety and quality – a secondary analysis of cross-sectional data. Sykepleien Forskning. 2024;19(95607):e-95607. DOI: 10.4220/Sykepleienf.2024.95607en
Introduction
Highly qualified staff are the most important input factor in hospitals. It has been and will remain a challenge to manage human resources to ensure that patients receive high-quality, safe treatment and that public resources are used efficiently (1). The concept of the Magnet hospital emerged in the United States in the 1980s in a study that aimed to identify common features of hospitals that attract and retain registered nurses (RNs) (2).
Since then, the Magnet hospital concept has been examined in a number of studies, almost exclusively in the United States. The common features identified have proven to be beneficial to the hospitals’ overall operation in terms of clinical, financial and organisational outcomes. The latter includes enhancing recruitment and stability of nursing staff levels (3).
The American Nurses Credentialing Center can provide accreditation as a recognised Magnet hospital to individual hospitals, conditional on the fulfilment of criteria that can be summed up in five main principles: transformational leadership; structural empowerment; exemplary professional practice; new knowledge, innovation and improvements; and empirical quality results (4).
Research and method development have primarily been carried out in the United States, and it is relevant to ask whether findings from studies in the United States can be replicated in Europe. Two international, EU-funded studies have used a method developed in the United States to study the management of RNs at hospitals in Europe. Data has been collected regarding RNs’ perceptions of working conditions and well-being.
Furthermore, organisational information on hospitals’ patient outcomes, number of beds and number of stays has been collected. Knowledge that can help underpin efficient management of nursing resources in hospitals is valuable to RNs as a group and to society as a whole, in the light of current and future needs for qualified health personnel.
The Norwegian Nurses Organisation has provided financial support for Norwegian participation in both studies. Lovisenberg Diaconal Hospital, hereafter referred to as Lovisenberg, participated in both studies.
RN4CAST: Registered Nurse forecasting in Europe (2009–2011)
RNs at 486 hospitals in 12 European countries, including 35 hospitals in Norway, participated in the cross-sectional study RN4CAST (2009–2011). The main objective of RN4CAST was to contribute to better planning and management of nursing resources in Europe (5). Compared to the other countries, the national results in Norway were consistently good (6, 7). However, there were large differences between individual hospitals and different types of hospitals within Norway. Among the Norwegian hospitals, the best results were achieved by private hospitals run by non-profit organisations (8).
Magnet4Europe (2020–2024)
In the intervention study Magnet4Europe (M4E, 2020–2024), over 60 hospitals in six countries participated. The intervention consisted of introducing changes in line with the main principles of Magnet hospitals. Each individual hospital decided which of these was to be a priority, based on information from gap analyses in some cases. In the course of the transition process, empirical measurements were gathered, using, for example, employee surveys. A baseline measurement was carried out at the start of 2021, before the intervention began (9).
In M4E, both RNs and doctors (US: physicians) were included in the employee survey. Lovisenberg is the only Norwegian hospital participating in Magnet4Europe, and a research article describes the local interventions that have been implemented (10).
The two surveys collected data on RNs’ assessments of different aspects of the work environment, separated by a twelve-year interval. The aim of this article is to compare the responses of RNs working at Lovisenberg to questions that were posed in both surveys in 2009 and 2021.
Method
Data collection for RN4CAST in 2009 included a comprehensive survey on working conditions, well-being, patient safety and quality. Some of the questions were reused in the M4E study, in which the first of three surveys was conducted in spring 2021 during the COVID-19 pandemic. We compared the questions that were the same in both 2009 and 2021.
A group of eight items were derived from the Nursing Work Index (NWI). The NWI was developed during the early studies of Magnet hospitals in the US. The instrument covers characteristics such as cooperation, development opportunities and management, which the studies of Magnet hospitals indicated were important for a workplace to be a good place for RNs to work. The respondent rates the presence of a particular characteristic at their own workplace, using a scale from 1 (strongly disagree) to 4 (strongly agree).
Signs of emotional exhaustion were measured using the Emotional Exhaustion subscale in the Maslach Burnout Inventory (MBI-EE). The nine questions in the subscale describe feelings connected to work. The response requires the respondent to note how frequently they feel a certain way, from 0 (never) to 6 (every day). The score that is represented here is an average of the nine questions, where there was a response to all questions (12, 13).
In both 2009 and 2021, items concerning patient safety, the frequency of missed nursing care, general assessments and individual background variables were included.
All RNs who had direct contact with patients in the medical and surgical wards for adult patients, including intensive care units, participated. RNs in small part-time positions were excluded. In 2009, the minimum cut-off point was 20% (of a full-time position), while in 2021 it was 30%.
In autumn 2009, the local representative of the Norwegian Nurses Organisation distributed paper copies of the survey. This was followed up by locally initiated measures to increase the response rate. It was not possible to send direct reminders to individuals. In spring 2021, the survey was conducted online. The employees, (including doctors who participated on this occasion), were contacted via email and could register on an Internet-based platform where the questions were presented electronically. The hospital sent three reminders and thank-you messages to all included via email. Various measures were implemented to promote participation and raise awareness concerning the survey. The responses from RNs in 2009 and 2021 were compared using descriptive statistics.
Differences in the respondents’ ages and length of work experience, as well as the results of the patient safety questions, were tested using the Student’s t-test for independent samples. The remaining differences were tested using Pearson’s chi-squared test. We conducted the analyses using IBM SPSS software, version 29. We selected a limit of p ≤ 0.05 for statistical significance.
The data protection routines in RN4CAST were submitted to the data protection officer for research at the Norwegian Centre for Research Data (NSD), now known as Sikt – the Norwegian Agency for Shared Services in Education and Research (reference number 22537). In M4E, some of the questions focused on health. The survey was assessed by the Regional Committee for Medical and Health Research Ethics (REK South-East D, reference number 166980). We obtained relevant data concerning the number of beds and patient turnover from Lovisenberg’s internal records.
Results
Data from the surveys
In 2009, 168 printed questionnaires were distributed, which received a total of 108 (64.3%) responses. In 2021, 218 (82.8%) RNs registered and responded to the survey. Except for the size of the positions of those who worked part-time and the number of years of nursing experience, the differences between the known characteristics of the two groups of respondents were not statistically significant. See the comparison in Table 1. A closer analysis of the data showed that in 2021, the oldest RNs had far more work experience than those surveyed in 2009, and this pushed the average up.
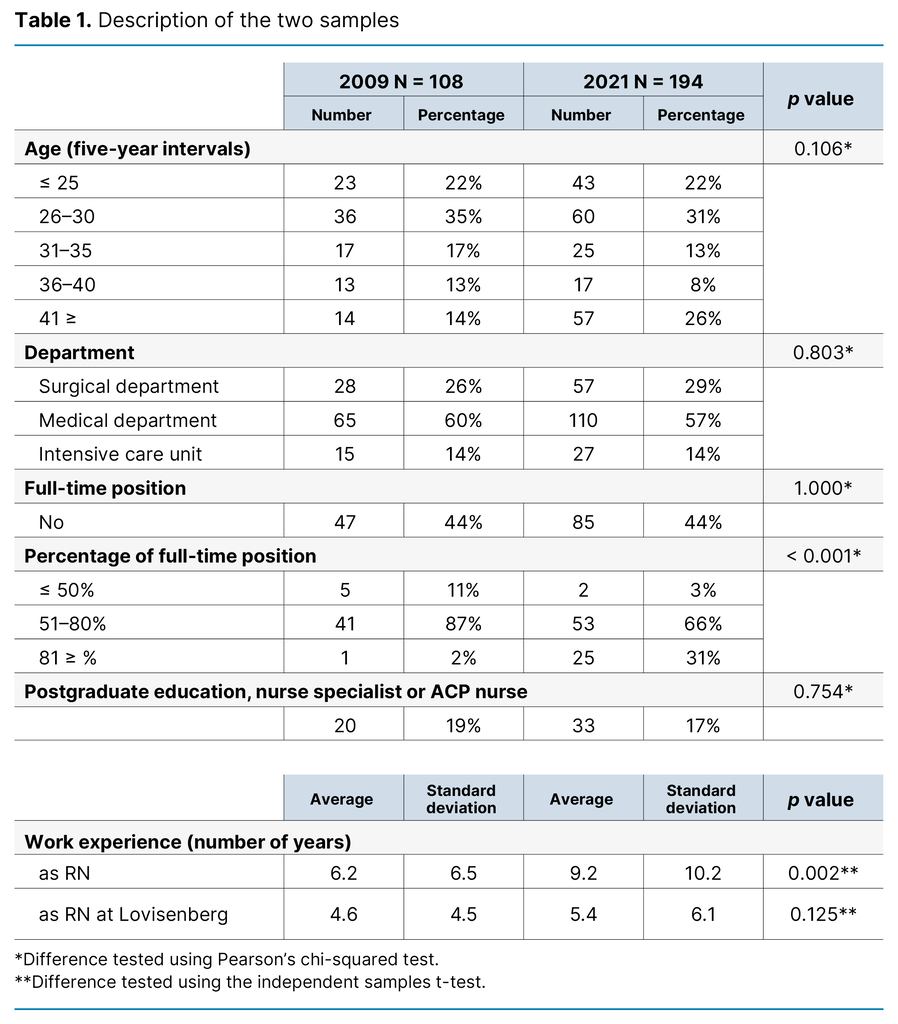
In the responses to the eight items from the NWI, the general tendency is that the proportion of positive answers (completely agree / agree) was largest in 2021 (Table 2). The biggest difference concerned the question about immediate supervisors, with an increase in the proportion of positive responses of 13 percentage points (p = 0.002).
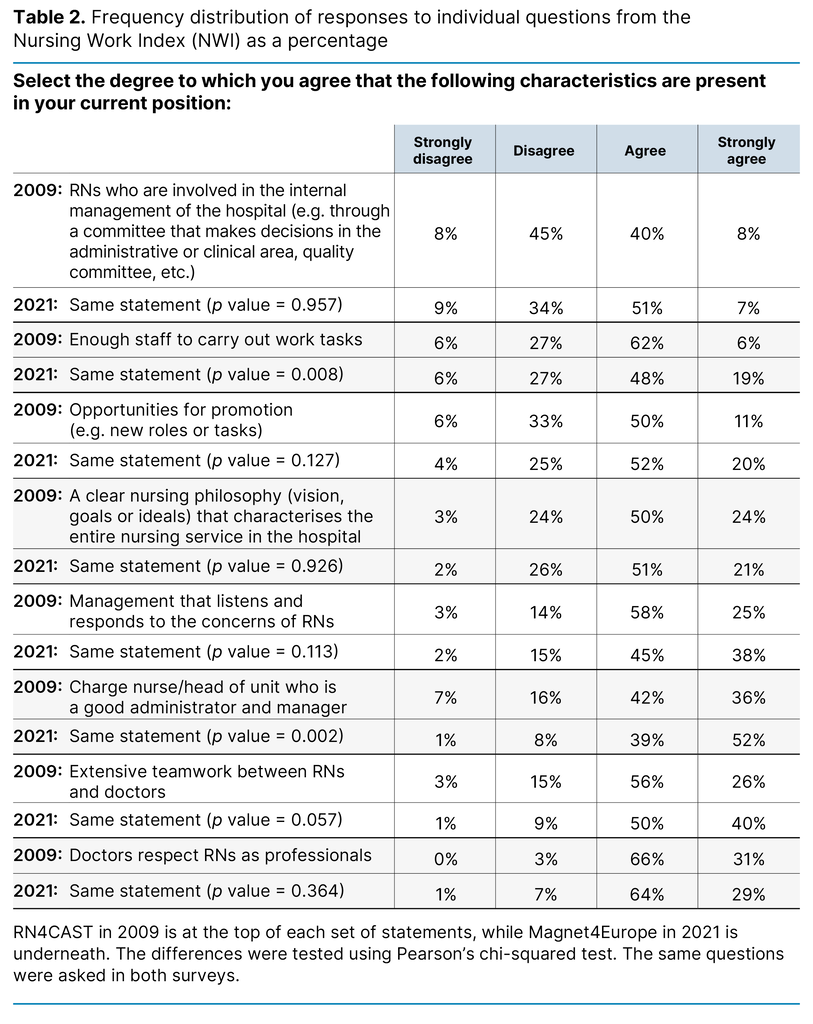
In relation to having sufficient staff to get the work done, the proportion of positive responses was 1 percentage points higher in 2021 than 2009. However, the proportion of respondents who answered ‘strongly agree’ as opposed to ‘agree’, was considerably higher, with an increase of 13 percentage points (p = 0.008). The proportion of positive responses to the question about cooperation between RNs and doctors was 8 percentage points higher in 2021 than in 2009, while the p value was just above the chosen limit for statistical significance (p = 0.057).
For the whole hospital, the number of patients per RN ‘on their most recent shift’ was 4.5 in 2009 and 3.6 in 2021 (p = 0.010). The average number of patients per RN in the two surveys was 4.8 and 3.4 respectively in surgical wards, 5.2 and 4.2 in medical wards and 1.5 in intensive wards in both surveys. See Appendix 1 [in Norwegian] for more details.
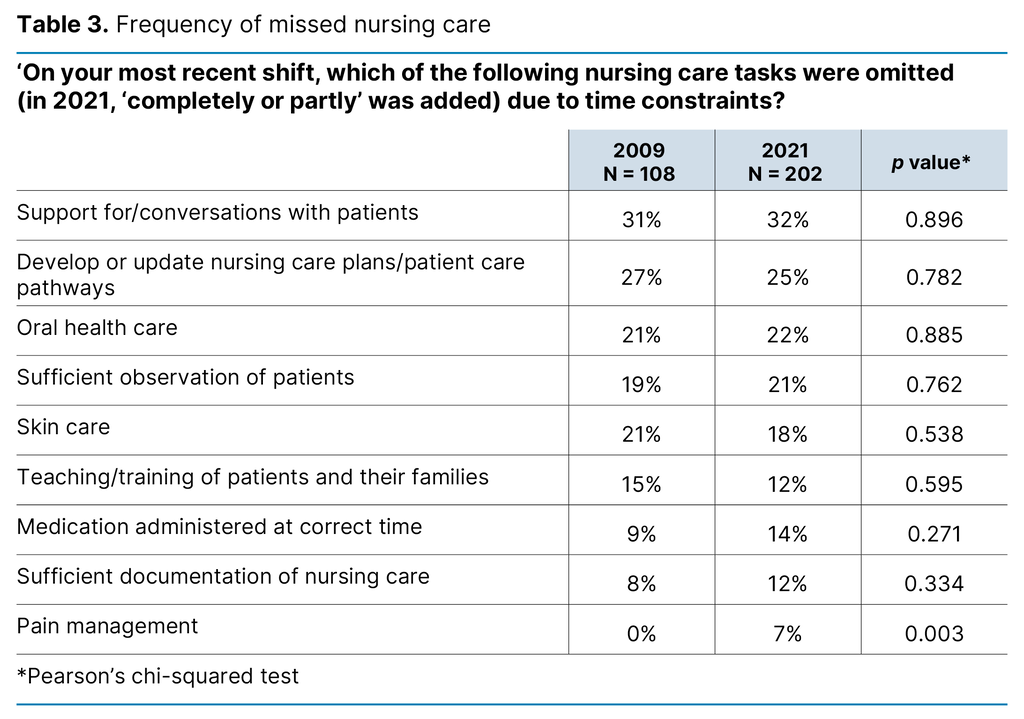
On a common list of nine potential missed nursing care activities, the frequency was quite similar in the two surveys. In 2009, no respondents reported necessary pain management as missed. In 2021, the percentage was 7% (p = 0.003). See Table 3 for a complete list of results.
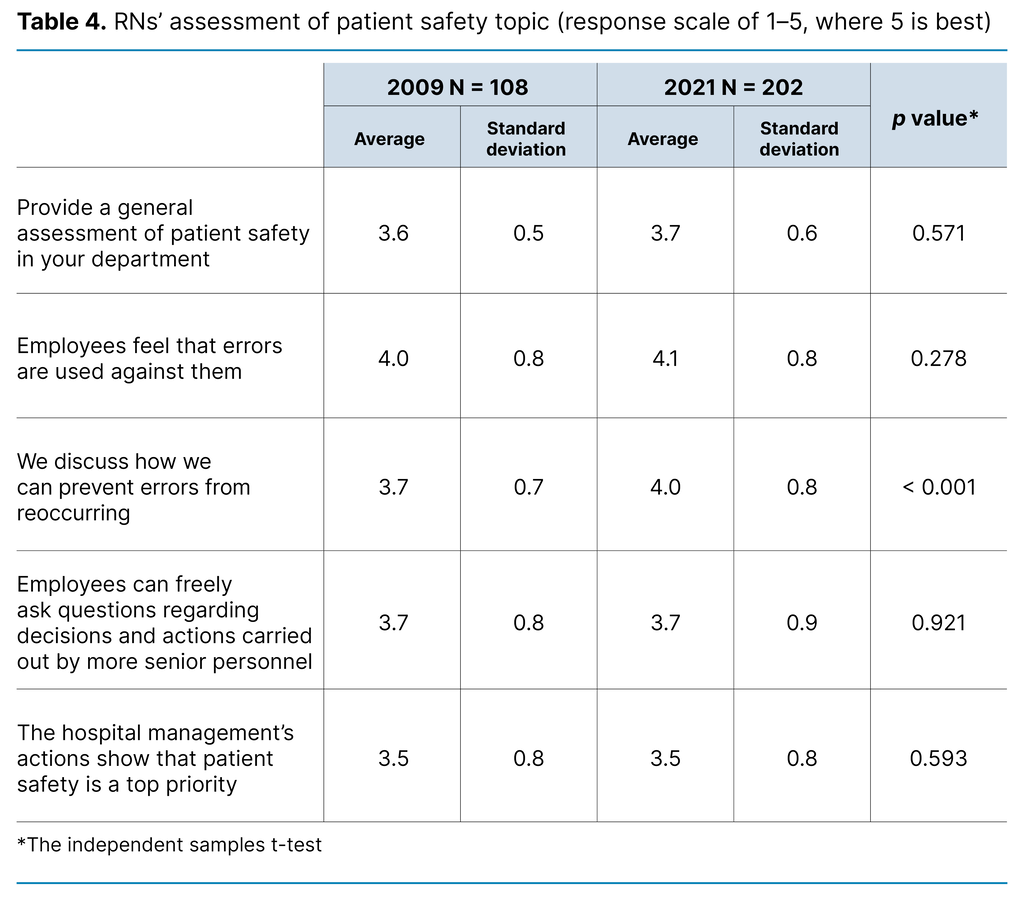
Five questions on patient safety were comparable (see Table 4). The tendency in the mean scores was unchanged or somewhat better in 2021. There was a positive change in terms of discussing errors to prevent reoccurrence, with an increase from 3.7 to 4.0 (p < 0.001).
The level of emotional exhaustion (MBI-EE) was the same. The mean and standard deviation in 2009 was 1.89 and 0.91 respectively. In 2021, it was 1.95 and 1.25 (p = 0.664). The extent of working overtime remained the same for Lovisenberg as a whole, with different results in the individual departments (Appendix 2 – in Norwegian). There was no change in the percentage of RNs who intended to leave the next year (2009: 17.0%; and 2021: 19.0%, p = 0.395), nor was there in the percentage among those who intended to leave Lovisenberg and also quit the nursing profession entirely (2009: 8.7%, and 2021: 11.4%, p = 0.190).
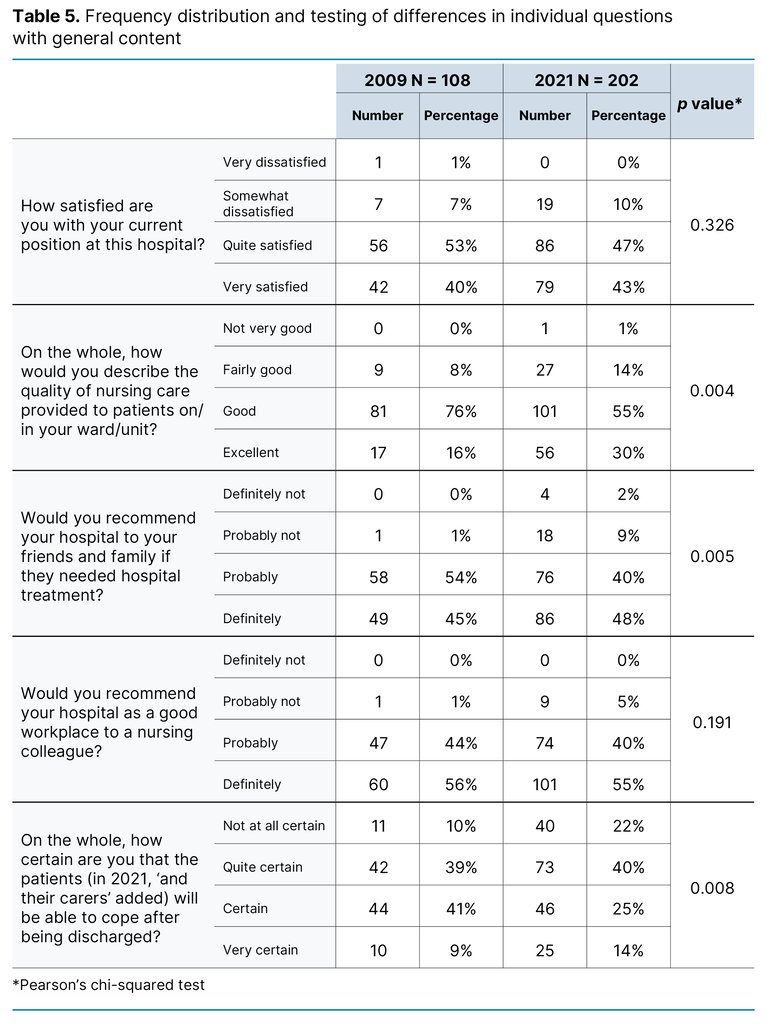
In regard to the five ‘on the whole’ questions (Table 5), there was a general tendency towards a lower score in 2021 than in 2009. In the respondents’ general assessment of the quality of nursing care, the proportion positive responses was 7 percentage points lower in 2021 than in 2009 (p = 0.004), and in regard to whether they would recommend the hospital to family and friends, the proportion was 11 percentage points lower (p = 0.005). In response to the question about how certain the respondent was that patients would be able to cope after being discharged, the proportion positive responses was 11 percentage points lower in 2021 than in 2009 (p = 0.008).
Data from other sources
Registration practices have changed during the period, which makes it difficult to compare figures that relate to operation in the two years in question. The standard number of beds was 158 in 2009 and 153 in 2020 (the closest year with complete figures); in both years, 12 beds in the palliative care unit were included. The number of admissions to the hospital was 10,208 in 2009 and 10,252 in 2020. In the surgical clinic, the average length of stay fell from 3.2 in 2009 to 2.0 in 2020, and there was a corresponding drop in the medical clinic from 5.6 to 3.9.
The hospital’s personnel data information system cannot provide comparable information regarding the number of full-time equivalents for RNs in 2009 and 2021 (or the closest year).
Discussion
In this secondary analysis of survey data, we have compared responses from RNs at Lovisenberg in 2009 and 2021. The results are mixed and do not confirm that everything was better before or that everything is better now.
Working conditions and working hours
Responses to the questions from the NWI showed that RNs felt that working conditions were better in 2021 in relation to specific matters such as cooperation with doctors and their immediate supervisor, and staffing levels (Table 2). The responses to the number of patients per RN (Appendix 1 – in Norwegian) indicate that staffing levels have also increased. We have not been able to find administrative figures to support this, but the impression of increased staffing levels at the local level corresponds with the national tendency in the development of the larger occupational groups in the specialist health service, although the figures here too are uncertain (1, Chapter 4.2.3).
In 2017, the hospital introduced a leadership training programme consisting of four seminars over a nine-month period. The target group includes the managers of the clinical departments. This initiative perhaps partly explains why the RNs were more satisfied with their immediate supervisor in 2021 than in 2009.
The percentage of RNs working overtime at Lovisenberg as a whole remained unchanged. It is worth noting that the 2021 survey was conducted during the COVID-19 pandemic, when the hospital had a higher level of preparedness. This may have influenced the results, but we have no information to assume how. At department level, it appears that there has been a change, but the differences between 2009 and 2021 are not statistically significant (Appendix 2 – in Norwegian).
Missed nursing care
In relation to missed nursing care (Table 3), the situation remained unchanged except for pain management. The increased frequency of missed pain management in 2021 may be connected to the fact that pain management options were more advanced and resource-intensive than in 2009, or that RNs’ knowledge and/or their expectations regarding efficient pain management had increased.
The similarity in the ranking of the various missed nursing care tasks is thought-provoking. In both surveys, comfort/talk with patients was the activity most frequently reported as missed (in 2021, completely or partly missed) on the most recent shift, while missed pain management was reported by the lowest number of respondents. Whether this is an indication of the normalisation of missed nursing care in the daily work at the hospital is an open question. When time is insufficient, is comforting/talking with patients the first activity that is omitted, followed by developing or updating patient plan of care/care pathways or oral hygiene as numbers two or three?
The introductory text to the question on missed nursing care was as follows: ‘On the most recent day/shift you worked, which of the following nursing care activities were necessary but left undone (in 2021, added ‘fully or partially’) because of time constraints? Mark all that apply…’ It is not known whether the addition to the text in 2021 influenced the responses.
Burnout
The burnout level (MBI-EE) measured among RNs at Lovisenberg was unchanged and is lower than previously reported scores using the MBI variant Human Services Survey (13). Recent international findings indicate that burnout among RNs increased during the COVID-19 pandemic (14, 15).
Patient safety and general quality assessments
During the patient safety campaign (2011–2013) and patient safety programme (2014–2018), systematic interventions were implemented to reduce the frequency of patient injuries. In the surveys, the responses to the questions on patient safety remained unchanged from 2009 to 2021, with one exception (Table 4). Any possible explanations for this are speculative. For example, it may be that patient safety per se has improved between 2009 and 2021. At the same time, RNs have a more acute awareness and higher expectations of good patient safety, which makes it less likely that they will give a positive description.
The RNs reported better working conditions in 2021 than in 2009. Nevertheless, the responses to three of the five ‘on the whole’ questions were poorer in the most recent survey (Table 5). We do not have the data to enable us to interpret this observation, and explanations may be both numerous and complex. We cannot rule out the possibility that the results were affected by differences in how the survey was conducted. It may also be the case that the understanding of responsible nursing practice has actually changed in the interval between surveys.
The available resources for providing nursing care services were perceived as better in relation to important aspects. With regard to RNs, we can say with certainty that there was a larger proportion of older RNs, and therefore RNs with more work experience, at Lovisenberg in 2021 than in 2009. The proportion of RNs with a postgraduate education was the same. We have some data on the activities that RNs carry out using available resources.
The objective of the Coordination Reform in 2012 was to enhance cooperation between the specialist and primary care services. Shorter stays in hospitals in 2021 meant that patients in wards had not progressed as far in their care pathways and had a more extensive need for nursing care when they were discharged than was the case in 2009. Faster patient turnover means more frequent discharges, and a greater need for follow-up leads to a need for better organisation of necessary nursing care and treatment after discharge. Moreover, the collection of data in spring 2021 occurred after almost a year of emergency preparedness across the entire health service in connection with the COVID-19 pandemic.
Strengths and weaknesses of the study
A strength of the study is that the surveys captured the perspectives of RNs. Many other surveys on working conditions have been developed for employees in general. Subsequently, the approach here means that the collected data is more relevant in relation to the challenges faced by RNs in their daily work environment.
In secondary analyses, the collected data is used for other purposes than the initial one. This means that the data is rarely the most relevant for the problem statement in question. The questions in RN4CAST/Magnet4Europe have international origins. Furthermore, it has been concluded previously that there is a need for a closer assessment of the relevance of the translated instruments in a Norwegian context, such as the NWI in these two surveys (16).
When data is collected using translated instruments, it may mean that the data is not of optimal relevance for bedside RNs in Norwegian hospitals. Analyses based on such data may still have value if there are no better alternatives. From a research ethics point of view, it is positive to use data that has already been collected in order to illuminate further hypotheses, where possible. A key objection to the study is that there are only two measuring points with a twelve-year interval.
We have not collected data that might have made it possible to examine how representative the respondent groups were. The response rate in the survey is good or very good compared to surveys involving similar topics and target groups. One review article referred to 675 studies of patient safety culture, in which the authors found that the response rate varied between 4.2 and 100%, with an average of 66.5% (17).
The surveys have small samples, with only 108 respondents in 2009. For example, responses to the question on the number of patients per RN were based on the most recent shift (Appendix 1 – in Norwegian). Staffing levels vary between departments and shifts – day, evening and night – and the responses could have been grouped accordingly. However, this would have resulted in such small groups of respondents that the results would have been too uncertain to have any value.
We cannot rule out the possibility that RNs have responded strategically to questions, for example, regarding nurse staffing levels. The question was framed in the same way in both surveys, and any tendency to respond in a way that suits the group best would probably apply in both cases. There are no comparable ‘objective’ statistics for these two years, a factor that may have provided more reliable and detailed information.
We have found evidence that staffing levels and management are better than before, but at the same time, RNs have described quality in general as poorer. There may be many explanations for this and they may be complex. We cannot rule out the possibility that the results were affected by differing data collection routines in the surveys in 2009 and 2021. It may also be the case that the norms for acceptable practice have changed in the interval between surveys. The high (and increasing) level of documentation required for treatment and nursing care is often described as a time thief that steals time from interactions with patients.
The findings in the study cannot be generalised as valid for other Norwegian hospitals. Lovisenberg is operated on a non-profit, charitable basis in line with its contract with the South-Eastern Norway Regional Health Authority, and it is run according to diaconal principles. All surgery carried out is elective. The medical clinic has the role of local hospital for districts in inner Oslo and has special competence in palliative care. Lovisenberg’s results in RN4CAST were in the top tier of Norwegian hospitals.
As far as we know, this is the only study that compares results over a period of time using descriptions of RNs’ daily work environment in hospitals in Norway. The study itself indicates indirectly a general lack of information that can help to inform good decision-making within human resources management. With today’s technological solutions, it should be possible to establish a national representative sample to monitor the situation in occupational groups that are indispensable in the health service. Monitoring should be based on information that is relevant to the respective groups’ daily work environment, not just the health authorities’ financial bottom line.
The complete data set from Lovisenberg in 2021 will be used together with the two follow-up surveys from spring 2022 and autumn 2023, in line with the main objectives of Magnet4Europe (9).
Conclusion
To compare snapshots of RNs’ daily work environment at Lovisenberg in 2009 and 2021, we have used data collected during two international studies. We found that the description of many of the factors were the same in the two surveys. Some working conditions were described as being better in 2021 than in 2009, but where differences were found, the ‘on the whole’ assessments were somewhat poorer in the most recent survey.
Acknowledgements
Thanks to all the RNs who responded to the surveys, to RNs Christine Raaen Tvedt PhD and Monica Bukkøy Kjetland for their indispensable efforts in data collection in 2009 and 2021 respectively. Thanks to Per Arne Holman for operational data on Lovisenberg and to peer reviewers for valuable input to the manuscript.
Funding
The international studies were funded by the EU. RN4CAST: Framework Programme 7, Grant Agreement 223468. Magnet4Europe: Horizon 2020, Grant Agreement 848031. The Norwegian Nurses Organisation (NSF) has contributed with financial support to RN4CAST and Magnet4Europe. NSF has not played a role in the design, execution or reporting of the studies.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge

Comments