Team-based organisational structure in the treatment of patients with complex diagnoses. A qualitative study of an obesity team in the specialist health service
Summary
Background: Morbid obesity is a complex and growing problem for which successful treatment requires a multidisciplinary approach. Establishing a comprehensive and cohesive treatment provision for patients with complex diagnoses can be challenging. Various measures have been introduced to break down organisational and professional barriers in health and welfare services. This article highlights the factors needed to facilitate a suitable team-based organisational structure in the treatment of patients with morbid obesity.
Objective: The study aims to contribute to the knowledge base about team-based organisational structures in the treatment of patients with complex diagnoses, in this case morbid obesity. We aimed to shed light on the planning and establishment process, the organisational structure of the team, and the cooperation with local services.
Method: We employed a qualitative research design. The empirical focus of the study was an obesity team in the specialist health service. The dataset consisted of interviews with 14 clinical practitioners who had experience from working in the team, as well as internal management documents. The analysis combined a deductive and inductive approach, and the empirical data were interpreted from an organisational theory perspective. A theoretical framework was used to elucidate the factors needed to facilitate a suitable team-based organisational structure in the treatment of patients with complex diagnoses.
Results: The clinical practitioners in the project group were able to exert influence in the planning of the obesity team, and sufficient time was allocated to attend meetings. The team was composed of a relevant mix of clinical disciplines, and had management support, clear roles and tasks, and a good collaborative culture. Due to the patients’ complex challenges, the team had to be flexible in relation to the standardised care pathway. The informants expressed that there was minimal cooperation with local services. Patients can, therefore, experience difficult transitions after completing treatment in the specialist health service.
Conclusion: A team-based organisational structure in relation to patient groups with complex diagnoses appears to be a suitable organisational structure within the specialist health service.
Cite the article
Grundstrøm C, Fineide M. Team-based organisational structure in the treatment of patients with complex diagnoses. A qualitative study of an obesity team in the specialist health service. Sykepleien Forskning. 2024;19(94809):e-94809. DOI: 10.4220/Sykepleienf.2024.94809en
Introduction
Lack of cooperation and coordination can lead to discontinuity in patient care, particularly for patients with complex diagnoses (1–3). Previous research and literature indicate that specialisation and the division of labour, varying organisational structures and levels, as well as differing disciplinary approaches, can make it difficult to achieve comprehensive solutions in practice, particularly for this patient group (4–8).
In recent decades, a number of solutions have been introduced to break down organisational and professional barriers in the provision of healthcare services and to create comprehensive and cohesive solutions for the individual patient (9, 10). The team-based organisational structure is an example of such a solution (11, 12, 14, 16).
There are various definitions of ‘team-based organisational structure’, but we have used the following: ‘[...] a small, multidisciplinary group with a common purpose, in which members share responsibility for achieving results’ (18, p. 37). Challenges can potentially arise when a multidisciplinary team is given shared responsibility for achieving results, and numerous factors can impact on the success of a team (11, 17–20).
Morbid obesity – a complex diagnosis
Morbid obesity is a complex and growing problem that requires broad expertise and a multidisciplinary approach for successful treatment (22). Research emphasises the importance of cooperation between the specialist health service and local services (12, 13, 20, 22). In 2011, Norwegian hospital trusts were ordered to ensure a comprehensive and cohesive service provision for patients with morbid obesity (25).
The purpose of this study was to increase the knowledge base about team-based organisational structures in the treatment of patients with complex diagnoses. Based on organisational theory, we posed the following question:
‘What factors are needed to facilitate a suitable team-based organisational structure in the treatment of patients with complex diagnoses?’
Inspired by a theoretical framework for analysing teams (21), we shed light on how the obesity team was planned and established, its organisational structure, and the cooperation with local services.
Method
The article is based on a qualitative analysis of data from a collaborative project between a research group and a hospital trust in Norway, hereafter referred to as ‘the Hospital’. The objective was to gain knowledge about new organisational forms, and the obesity team was selected for analysis.
Recruitment and sample
Table 1 gives an overview of the 14 informants recruited by the Hospital’s management through the project members in the Hospital and the first author. All team members in the obesity team, as well as two surgeons, were asked to participate in a focus group interview. One surgeon could not participate and was therefore interviewed individually.
We also conducted an individual interview with the senior consultant in internal medicine, referred to as ‘Senior consultant 1’, who provided additional information in follow-up telephone calls. Senior consultant 1 played a key role in both the planning and establishment of the team alongside one of the nutritionists. We also conducted an interview with the Hospital’s process facilitator.
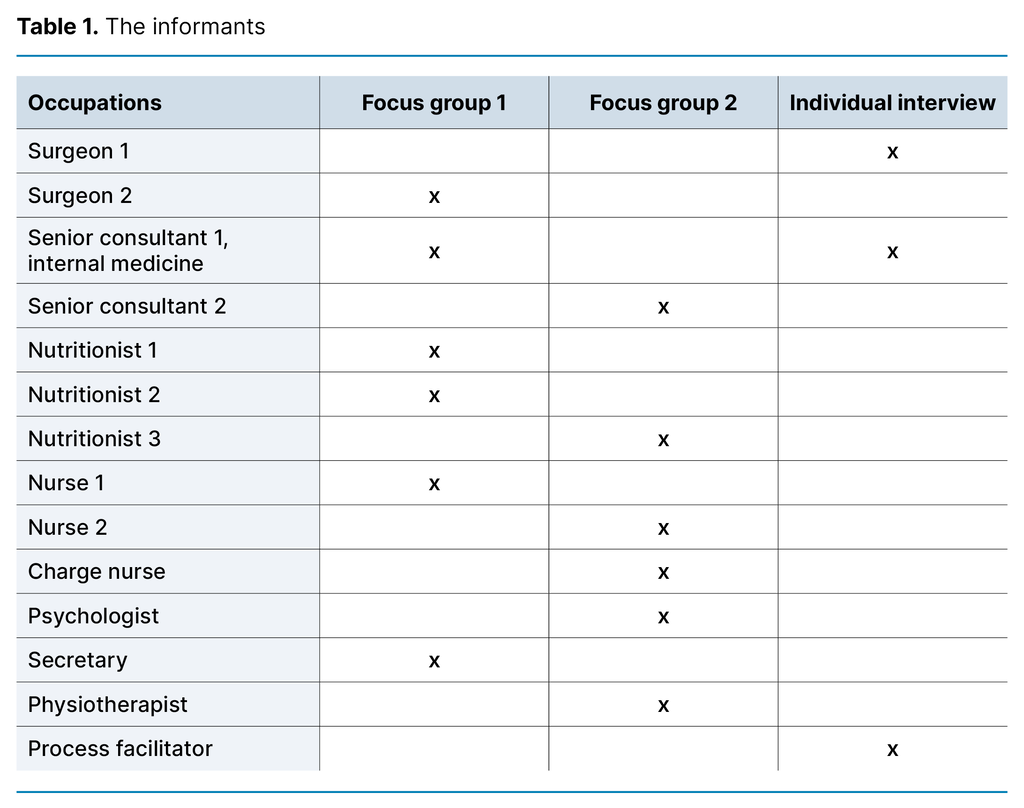
The focus group interview was a suitable method for us to elicit employees’ interpretations of the concept of ‘team-based organisational structure’ through discussion (26). The first author and another researcher in the project conducted the two focus group interviews and one individual interview (with Surgeon 1) at the Hospital between May and October 2018.
Each interview lasted approximately one hour. The interviews were semi-structured, and the interview guide consisted of open-ended questions with themes relating to the planning and organisation of the team. Keywords in the interview guide focussed on why the concept was introduced, what challenges needed to be addressed, how the planning was carried out, and who participated. We also asked participants to describe their work in the team and the characteristics of this organisational structure.
These questions helped shed light on informants’ interpretations of the new way of working. The team’s cooperation with external actors was not included in the interview guide, but the topic was raised by the informants. These data were also analysed.
The first author conducted individual interviews with the senior consultant in internal medicine and the process facilitator after the focus group interviews were completed. The interview guide for these interviews contained the same open-ended questions, but we also included some specific questions to confirm or refute statements made in the focus group interviews. Audio recordings were made of the interviews with the senior consultant and process facilitator.
We obtained 11 internal documents from the manager at the Obesity Clinic, where the team was located, from the project period May to November 2012. These consisted of an internal clinical commissioning policy document from management, minutes from working group meetings and steering group meetings, as well as a final report. The documents and an overview of the care pathway were intended to provide supplementary information to the other data.
Data analysis
The first author transcribed the individual interviews, and the focus group interviews were transcribed externally. Both authors read through all the interviews. According to Jacobsen (26), qualitative data analysis is made up of four components: documenting, exploring, systematising and categorising, as well as linking them together. An abductive analysis is characterised by a combined deductive and inductive approach (27).
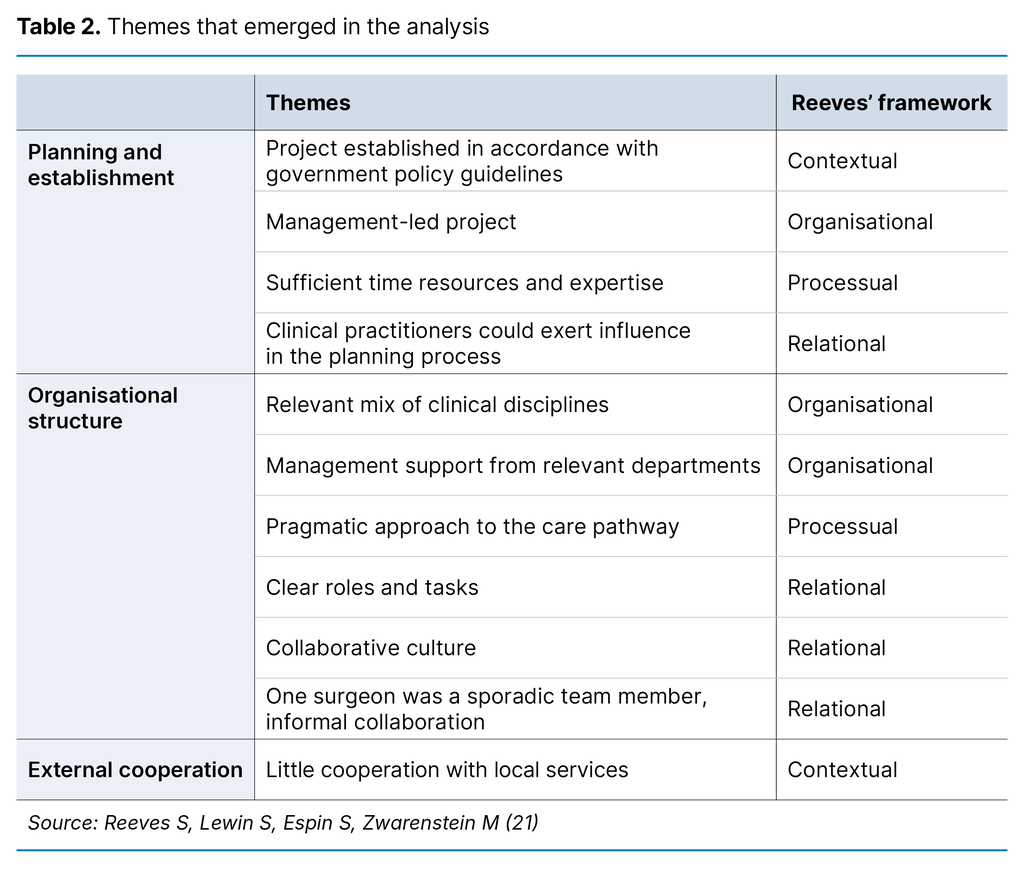
Our deductive approach was primarily inspired by a framework developed by Reeves et al. (21), which operates with four factors for team analysis. Each of the four factors is characterised by different elements, such as team composition and team members’ roles (relational), time, complexity and routines (processual), organisational support and professional representation (organisational) and culture, economics and political will (contextual).
The factors provide a basis for a broad approach to studying team-based organisational structures. The theoretical framework provided perspectives for interpreting the meaning of the empirical data (26–28). After coding, categories and themes emerged, which were sorted into a matrix, as illustrated in Table 2.
Ethical considerations
The study was reported to and approved by the Norwegian Centre for Research Data (NSD), reference number 58282. All informants signed an informed consent form for voluntary participation. The data were anonymised in the transcription process, and the audio files were stored on a locked USB drive. The audio files were deleted after the project was completed.
Results
The analysed material is presented in three parts: how the obesity team was planned and established, its organisational structure, and how the informants interpreted the cooperation with local services.
Planning and establishment
Government policy guidelines and directives (25) stating that patients with morbid obesity should be ensured a comprehensive and cohesive service provision were a central contextual factor. The hospital director established a project with a mandate to plan and establish an obesity team and obesity clinic within three months. Our study focuses on the organisational structure of the obesity team.
The steering group consisted of the Director of the Division of Medicine, the section heads in the Department of Internal Medicine and Department of Surgery, the Director of Medicine and Patient Safety, shop stewards from the Norwegian Nurses’ Organisation and the Norwegian Union of Municipal and General Employees, and the project manager. This composition meant that the project was primarily management-led, with close links to the clinical disciplines within the Hospital, which was a key organisational factor.
The project manager had a nursing and economics background and the project group consisted of clinical practitioners from internal medicine, surgical and medical wards, and psychiatry. Project members were released from their regular duties to participate in the project. The informants expressed that sufficient time had been allocated, which was an essential processual factor.
To ensure the quality of planned services and define the function, role and form of cooperation, regular meetings were held with the Learning and Mastery Centre, the Department of Physiotherapy and social services, as well as service user representatives. Visits were made to other hospitals in Norway and Sweden to study work methods and organisational structures. All the hospitals visited had adopted a multidisciplinary approach.
Ensuring the right expertise in the team was therefore crucial:
‘We refused to start until we had a psychologist on board because we believe that interdisciplinary collaboration is crucial, and we didn’t want to have to refer patients to the District Psychiatric Centre for assessment after six months. It was quite difficult to recruit one, and we were under pressure to open because of the large number of patients waiting.’ (Focus group 1)
The above quote suggests that the clinical practitioners had direct influence in the decision-making process, and that management was receptive to input from them, which appears to have been a significant relational factor. Which actors were involved in the planning process seems to play a crucial role in the organisational structure of the team. One informant said that if they had approached the issue of obesity from a purely medical perspective, the organisational structure of the team would have looked different: ‘So we listened carefully to the nutritionist regarding the organisational structure of the team’. (Interview, Senior consultant 1)
The project concluded with an organisational structure consisting of a multidisciplinary obesity team under the Department of Internal Medicine and the Department of Endocrinology, under the name ‘Obesity Clinic’.
Organisational structure
The team consisted of clinical practitioners from the departments of endocrinology, surgery, physiotherapy, medical rehabilitation and medical outpatient clinics. The occupations represented in the team were nurse, nutritionist, senior consultant in internal medicine, physiotherapist and psychologist. Resource priorities for the team appeared to have been clarified in the project phase, and the team was given additional resources after it was established.
The surgeon was an occasional member of the obesity team and only attended team meetings in which surgery was a relevant topic. This was referred to as problematic in one of the focus group interviews: ‘It could be said that if anything is problematic, it’s probably in the communication between the medical and surgical team members’. (Focus group 2)
It emerged that this was due to the large physical distance between the Obesity Clinic and the surgical department. In the individual interview, the surgeon reported that the collaboration worked well. However, the senior consultant at the outpatient clinic confirmed what was said in the focus group interview, noting that the collaborative cultures in the two departments differed, but that there was a lot of informal collaboration on patients in the form of phone calls and in-person meetings.
The team appears to be composed of a relevant mix of clinical disciplines, which was a key organisational factor. The variety of organisational affiliations can in itself hinder the team’s decision-making. This issue was not discussed by the informants other than in relation to the surgeon’s sporadic attendance at team meetings.
Involvement of the clinical practitioners in the obesity team seems to be both desired and accepted by the managers of the relevant departments. This is a significant organisational factor. In our interpretation, the management support can be a result of the collaboration between clinical staff and management in the planning and establishment process.
The Hospital had devised a normative care pathway that described the entire work process, from the assessment by a general practitioner (GP) to the completion of treatment. Multidisciplinary consultations and interdisciplinary evaluations were two core activities for the team and are described in the care pathway.
Table 3 gives an overview of the roles and tasks performed by the various clinical practitioners in individual consultations with patients, referred to as multidisciplinary consultations in the care pathway.
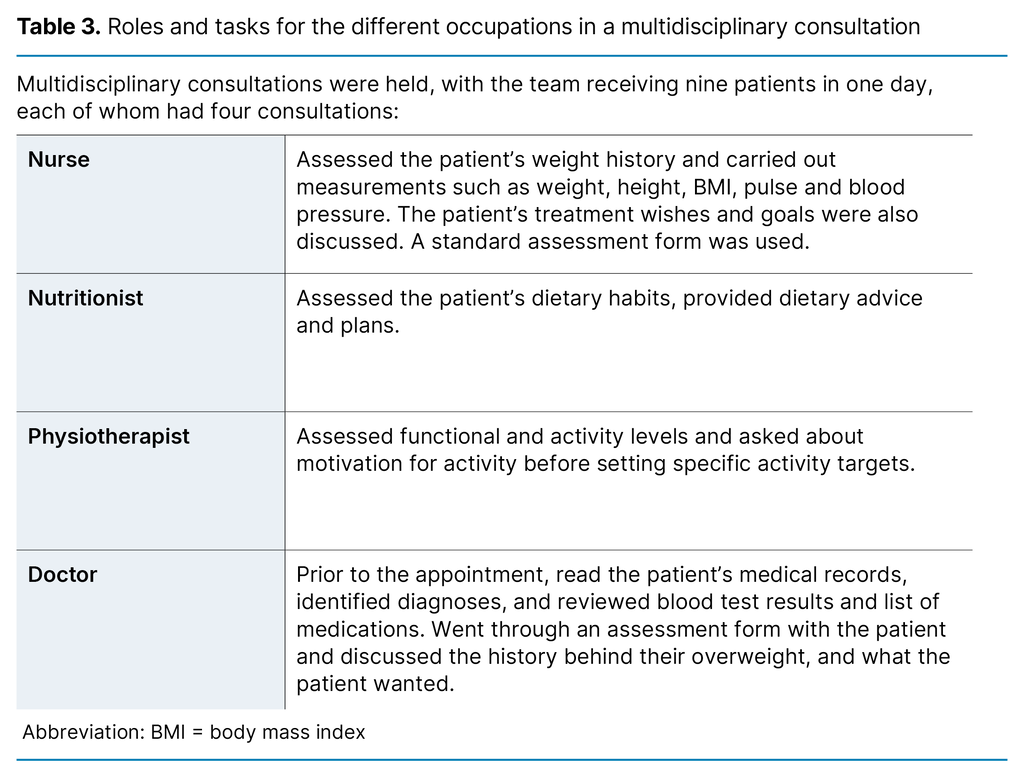
The psychologist did not hold patient consultations but conducted a separate assessment based on medical records. The psychologist then created a summary, which was used at the team meeting.
After the patients had attended the four consultations, the team met later in the day for an interdisciplinary evaluation, in which decisions were made about which treatment options the patient should be offered. The options were conservative treatment or bariatric surgery. Prior to surgery, conservative treatment was always given in the form of lifestyle change education, and some of the instructors were nurses.
The team took into account the patient’s wishes, goals, abilities, challenges and motivation, which were assessed using different methods by both a nurse and a doctor. If the team disagreed with the patient, an individual session was held with the psychologist for further assessment, before the team collectively decided on the form of treatment.
The informants reported that the patient could exert a relatively significant amount of influence on the decision regarding the form of treatment, and that the patient’s preference carried the most weight. Several claimed that the patient’s motivation and their influence on which treatment was offered could impact on the outcome of the treatment decision.
Several informants said that the flat decision-making structure worked well. It was mentioned several times in the interviews that the team made decisions based on the team members’ experiences and expertise. Our impression was that they agreed that all team members had an equal influence on the treatment decision.
However, one of the senior consultants believed that this was not quite true, since the doctors bore the clinical responsibility, and thus greater accountability and authority. Nevertheless, it was evident from the interviews that a collaborative culture existed in which trust and respect were important factors for a good relationship and communication. This suggests that the doctors in the team were receptive to input from the other healthcare professionals. This reflects central relational factors.
It emerged that the different treatment needs of patients did not always align with the described care pathway: ‘We have a template [care pathway] for the course of treatment, but there’s no one-size-fits-all solution. Individual assessments are always carried out because we have as many solutions as we have patients’. (Focus group 2)
This quote illustrates how the team demonstrated the necessary flexibility to meet the patient’s needs. They utilised their specific professional knowledge in the individual patient assessments and used this knowledge in the team’s interprofessional decision-making process. However, the informants also recognised the value of working together on this patient group, who had wide-ranging and complex problems spanning many years: ‘Due to the complexity, it’s difficult for one person to work alone with this patient group, no matter how skilled they are in their field’. (Focus group 1)
The informants said that they had much to learn from each other, and that the team-based organisational structure facilitated high-quality patient care. In our interpretation, the team had established a collaborative culture in which members shared responsibility for achieving good solutions for the patients.
Cooperation with local services
The patient’s GP and local services, such as Healthy Life Centres and rehabilitation units, were highlighted as key actors for patients ready to be discharged. The informants indicated that guidelines stated that the Hospital must advise the primary care service on the follow-up of patients ready to be discharged. However, it was unclear who there was cooperation with and how the patient was followed up: ‘What is there locally? And that’s the problem. […] so we find ourselves in the situation where we have to decide, if there is no [service provision], what do we do then?’. (Focus group 1)
The informants said that the patient needed follow-up after discharge but that there was no protocol for local follow-up in relation to obesity and mental health.
Summary of findings
Here we summarise the results in line with the four dimensions of the theoretical framework for analysing teams (21). Relational factors consisted of the influence of the clinical practitioners in the planning process. They had clear roles and tasks and a good collaborative culture. The processual factors were sufficient time resources and the right expertise in the planning process.
Due to the complex challenges faced by patients, the team had to adopt a pragmatic, flexible approach to the standardised care pathway. Organisational factors consisted of management support and a relevant mix of clinical disciplines. Contextual factors consisted of the establishment of the project in accordance with government policy guidelines and the limited cooperation with local services.
Discussion
The results showed that a range of factors played a role in establishing a team-based organisational structure that is appropriate for the treatment of patients with complex diagnoses. The fact that this was a multidisciplinary team in which all team members had the same ‘parent organisation’ may have been beneficial (11).
Implementing new ways of working
Implementing new ways of working can be extremely challenging, and a gap can arise between the concept of a team-based organisational structure and practice (11, 13, 29, 30). The involvement of relevant managers, different clinical disciplines within the project team, and employee organisations in the planning process may have helped clarify possible organisational and profession-specific challenges. Domain conflicts between professions can arise during the planning process and within the activities of the team (4).
Individual patient consultations prior to the team meeting can create professional disagreements in the team because each team member brings their specific professional expertise to the team. However, the informants in our study seemed to be more concerned with complementing each other’s expertise than protecting their own (knowledge) domain.
It therefore appears that the clinical staff and management worked ‘hand in hand’ throughout the planning process. This ensured a close link between the concept of a team-based organisational structure and its establishment. Thus, there may be a correlation between how the planning was carried out, including which actors participated, and whether the solution, i.e. the establishment of the team, functioned as intended.
Need for tailored solutions
We have seen how national guidelines and the literature support team-based organisational structures as a potential solution in the treatment of patients with complex diagnoses, where teams can break down existing organisational barriers and create flexibility within the organisational structure (11). Parallel to establishing the obesity team, team members were expected to work in accordance with the care pathway for obesity, using standardised protocols (11, 31).
We see here two contradictory government policy guidelines: one where there is a need for flexible and tailored treatment options through establishing teams, and the other where there is a need to standardise work processes through a care pathway. Mintzberg’s (32) thesis is that developing and applying standardised work processes is an important coordination mechanism where there are high levels of division of labour and specialisation. However, standardisation is not always a good solution (32).
This is highlighted by our finding that informants did not use the care pathway because the patient’s needs required tailored solutions. We have not collected data on which clinical protocols the team members used, but in the individual consultations, standardised assessment protocols were used. These protocols can serve as important decision support tools, which can significantly aid the functioning of the team (33). We see here that the team’s flexibility in a specialised and standardised hospital setting was dependent on non-rigid adherence to the standardised care pathway.
Difficult patient transitions
The final aspect we want to highlight is the risk of difficult patient transitions between the Hospital and the local services. Admittedly, the team’s focus was on internal collaboration within the specialist health service, but patients only receive treatment in the specialist health service for a limited duration. According to the intentions of Norway’s Coordination Reform in health care, most of the patient care and follow-up is to be carried out where the patient lives (34).
Patients with complex and multifaceted problems will mainly require simultaneous efforts from various services, often from the specialist health service, their GP and the primary care service. This in turn will require shared and overlapping responsibilities (12, 13). Patients are often referred by their GP, who plays a key role before, during and after treatment in the specialist health service (35).
In our study, the team-based organisational structure appears to have helped break down organisational and professional barriers within the specialist health service. However, there are strong indications that more focus should be placed on creating organisational solutions throughout the health service for patients with complex needs. Team-based organisational structures may be a solution here, but there may also be other measures that can help create comprehensive and cohesive solutions for the individual patient.
Strengths and weaknesses of the study
Data were only collected from one team at one hospital, which means that the findings should be interpreted with caution. It may be a weakness of the study that the hospital itself primarily recruited informants. The invitation to participate was openly extended to all team members and key personnel, and is not therefore considered to have impacted the design and results of the study.
We have further developed the theoretical framework by Reeves et al. (21) by also using it to analyse the planning and establishment process in addition to analysing the team. This helped us to form a deeper understanding of the importance of an effective planning and establishment process for the functioning of the team.
Conclusion
The study revealed that clear objectives, a detailed project plan, sufficient resources from clinical disciplines and sufficient influence by clinical practitioners in the planning process were important factors for successfully creating multidisciplinary teams.
We would argue that clear roles and tasks, a good collaborative culture, management support and a relevant mix of clinical disciplines are factors that are needed to facilitate a suitable team-based organisational structure in the treatment of patients with complex diagnoses. The study also showed that the individual needs of patients required the team to adopt a pragmatic approach to the standardised care pathway. By doing so, the team was able to be flexible in its efforts to meet the patients’ treatment needs.
The informants reported that there was little cooperation with local services. Difficult transitions between the specialist health service and local services, such as the patient’s GP, are also conceivable.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge






Comments