Parents’ experiences of sleep testing in children under the auspices of hospital at home
Summary
Background: Sleep testing is a general term for the investigation of breathing patterns during sleep, and has traditionally been performed in a hospital setting. Testing sleep at home has sometimes been regarded with scepticism because the recordings could potentially be of poorer quality. However, studies show that sleep recordings at home have the same rate of interpretability as in hospital. In this project, the Children and Youth Clinic offered children and their parents the opportunity to carry out sleep testing of the child at home. Sleep testing using polygraphy and transcutaneous oxygen measurement is performed to assess respiratory disturbances in children with a variety of respiratory and sleep problems.
Objective: The objective of the study was to describe parents’ experiences of sleep testing in children under the auspices of hospital at home (HaH).
Method: We applied a qualitative method to obtain data by using individual semi-structured, in-depth interviews. In order to analyse the dataset, we used Braun and Clarke’s reflexive thematic analysis method.
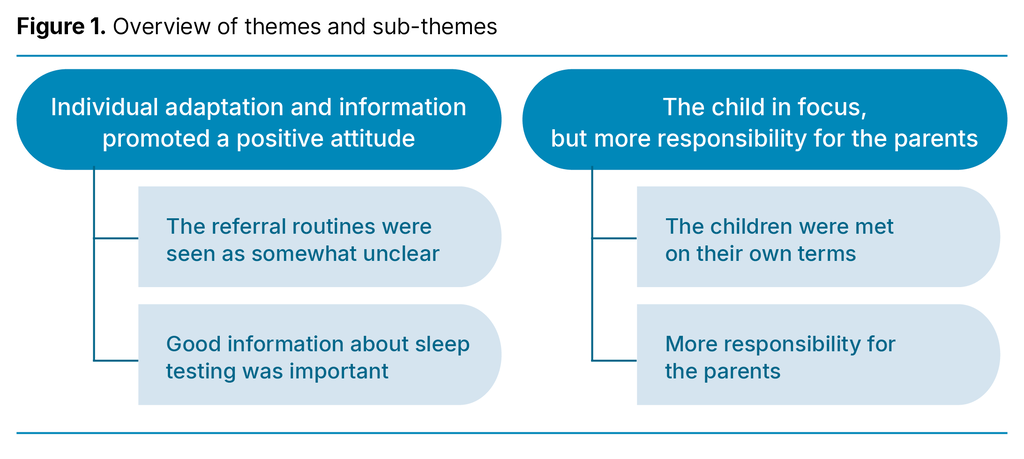
Results: Six mothers were interviewed. We identified two themes with two accompanying sub-themes. The themes were ‘Individual adaptation and information promoted a positive attitude’ and ‘The child in focus, but more responsibility for the parents’.
Conclusion: The mothers in our study found that home-based sleep testing under the auspices of HaH was a good alternative to traditional sleep testing in a ward. This option can help the family maintain a normal everyday life, while accessing health care at home may be less stressful than having to travel to the hospital. Clear information about this option and the procedures can increase parents’ sense of mastery. More research in the field from the perspective of different users is needed.
Cite the article
Granodd M, Beisland E. Parents’ experiences of sleep testing in children under the auspices of hospital at home. Sykepleien Forskning. 2024;19(95158):e-95158. DOI: 10.4220/Sykepleienf.2024.95158en
Introduction
Sleep testing is a general term for the investigation of breathing patterns during sleep (1), and has traditionally been performed in a hospital setting. This project offered the option of sleep testing children and adolescents at home using polygraphy and transcutaneous oxygen measurement of children and adolescents. The objective was to assess respiratory disturbances in children with a variety of respiratory and sleep problems.
During polygraphy, the child is connected to a nasal catheter that measures airflow (2). Two bands are placed round their chest and stomach to monitor their respiratory movement. A finger probe monitors their pulse oximetry, and a box attached to the child’s chest records measurements and makes an audio-recording. Arterial blood gas, pulse and oxygen saturation are measured by means of a sensor attached to the skin (3).
A specialist health service nurse from HaH visited the family, informed them about the equipment and attached it in the evening. The family were informed about the audio-recording and that they had to check the child hourly during the night to ensure that the equipment remained in place.
If problems arose, the parents could call the paediatric respiratory care ward. The following morning, the equipment was detached by the HaH nurse, who transferred the data to analysis software. When a doctor had interpreted the recording, the parents were informed of the results by telephone.
Children are to be admitted to hospital if medical care cannot be ensured in the home or at an outpatient clinic (4). The earliest types of HaH were established in the Nordic countries in the 1990s. HaH offers children and their parents the option of receiving specialist health services at home (5). Since that time, the model has been adopted in most of Norway’s major hospitals, and the patient group is constantly expanding (6).
The Norwegian National Health and Hospital Plan uses the term ‘outreaching hospital’, and HaH is seen as an important measure for achieving the goal of treating patients at home to the greatest extent possible (7).
Family-centred care is central in the field of paediatric nursing, and is based on reciprocal cooperation between families and health personnel in the case of children’s illnesses (8, 9). The family is seen as an important resource for the young patient, and the special needs of family members are emphasised. When specialist health services such as HaH come to the patient’s home, the family is on home ground. A main premise for examining and treating the child in their home is that more responsibility falls on the parents (5).
Earlier research
In some cases, home-based sleep testing has been met with scepticism because the recordings can potentially be of poorer quality (10). However, the study shows that sleep testing carried out at home has the same rate of interpretability as in hospital (11–13). A high percentage of families were very satisfied that the testing could take place at home. One study estimates that sleep testing at home is less than half as expensive as carrying it out in hospital (11).
Although there are international studies on home-based health services to children in general, many of these stem from the primary health service. This makes it difficult to transfer the results to the Norwegian context, where HaH is part of the specialist health service (5). Aasen et al.’s study at Akershus University Hospital suggests that HaH is a safe treatment option for children with many different diagnoses and support needs. The researchers call for further studies of the HaH from different perspectives.
A Danish study found that families were largely satisfied with the opportunity to stay at home as long as the tasks assigned to them were manageable (15). Parker et al. (16) stated that more research is needed on the psychosocial needs of children and family members who receive home-based health care.
The scope of HaH is set to increase in the years ahead (5), and sleep testing will become a diagnostic tool that can be used at home (17).
The objective of the study
The objective of the study was to describe parents’ experiences of sleep testing under the auspices of HaH.
Method
The study has a qualitative descriptive design as we wished to describe the parents’ experiences of home-based sleep testing (18). We applied the recommended criteria for reporting qualitative research by using the ‘Consolidated Criteria for Reporting Qualitative Research’ (COREQ) checklist (19).
The study stems from a pilot project on HaH at a Norwegian university hospital that commenced in spring 2020. Patients suitable for HaH follow-up had to be in a stable phase, and HaH was an optional alternative to admission to a traditional ward. The patients were formally admitted and could return to hospital if necessary. The child’s paediatrician had medical responsibility.
Sample and recruitment
The inclusion criteria were: parents of children between the ages of 0 and 18 years where the child had undergone sleep testing in the home during the previous six months with the support of HaH, irrespective of the reason. The parents had to be able to speak Norwegian.
We included informants on a rolling basis. The project manager gave the informants oral and written information about the project. The first author called informants who gave informed consent to set a date for the interview. We asked thirteen sets of parents and all six who consented were included. No one withdrew in the course of the project.
Data collection
The dataset was obtained through six individual semi-structured, in-depth interviews carried out by the first author. On the basis of the research question, we devised themes for the interview guide in line with Kallio et al.’s framework (20). The interview guide was pilot tested. The first author conducted the interviews, which lasted 30–45 minutes, in the informants’ homes. We made audio-recordings and transcribed the audio files verbatim and anonymised them.
Analysis
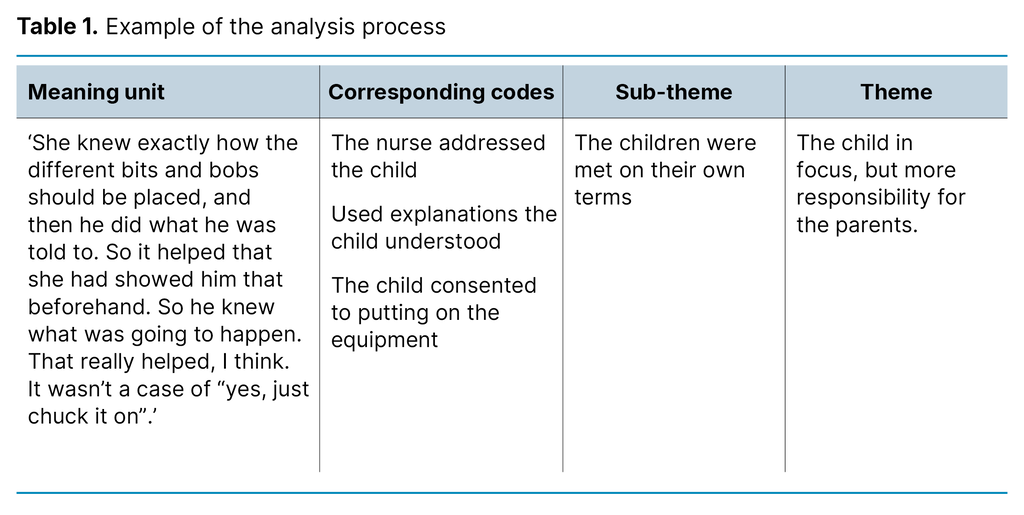
The dataset was analysed in accordance with Braun and Clarke’s reflexive thematic analysis method (21–23). In line with the six steps of the analysis, we started by familiarising ourselves with the data by reading the transcriptions carefully. In step two, we noted the codes that described the different phenomena in the dataset. In steps three, four and five, codes with similar meanings were sorted and synthesised into different sub-themes (Table 1).
Together, we reviewed and discussed the sub-themes and generated main themes. Step six involved reporting, where the content of the final analysis table was presented in text. Both authors played an active part throughout the analysis, and we met regularly for discussion and reflection. We used an iterative process in which data and context were interpreted in relation to each other to ensure that the presentation of the informants’ perspectives was as accurate as possible (18) (Table 1).
Ethical considerations
All informants signed consent forms before the interviews. We pointed out that participation was voluntary and that if they did not participate, it would not impact on further follow-up. All audio files and transcriptions were treated confidentially and stored on the research server at the Western Norway University of Applied Sciences.
The main project was approved by the Regional Committees for Medical and Health Research Ethics (REK) (reference number 155486) and was reported to the Norwegian Centre for Research Data, now known as Sikt – the Norwegian Agency for Shared Services in Education and Research (reference number 625117).
Results
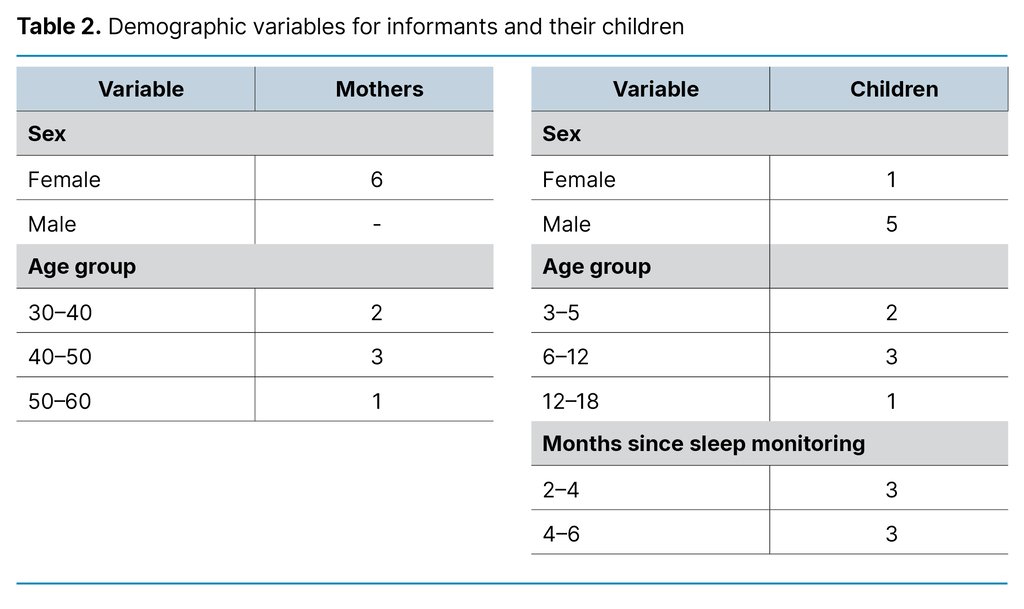
The children whose sleep was monitored had different and complex health challenges as grounds for the procedure. Four of the children were monitored for the first time, while two had undergone the procedure several times, both in hospital and at home. All the children were monitored using polygraphy, and one child was also monitored using transcutaneous oxygen measurement. Table 2 shows demographic variables.
Through the analysis process, we identified two themes, each with two sub-themes (Figure 1).
Individual adaptation and information promoted a positive attitude
The referral routines were seen as somewhat unclear
Some of the mothers said that they were completely unaware that their child was to be referred for sleep testing. They had either not received any information about this during the consultation with their GP or had not understood the information. Several also said that they did not know that sleep testing could be carried out at home with HaH. Others had carried out the procedure at home previously and wondered if the child could do the same again. Two of the mothers described how they were quite surprised when told that the child’s sleep was to be monitored at home:
‘So we just received a phone call, and I was sort of thinking: “What are we talking about here?” I thought it was a bit strange. And then she began to sort of explain.’
No one appeared to be unwilling to carry out the procedure at home, and several said that they were glad of the opportunity.
Good information about sleep testing was important
Most people felt that they had received good information about what sleep testing entailed for them and the child. One mother, on the other hand, had not been informed that she would have to get up every hour to check the equipment, and she had not had time to ask for a day off work the following day.
The mothers used the information to prepare the child and explain the procedure in words that the child could understand. Some used examples from a time when one of the parents had undergone sleep testing, something the child remembered. One family had shown photographs from a previous occasion when the child’s sleep had been monitored:
‘We had a few photos from the other times. So we just showed them and said that someone would be coming along with some equipment that he would have to have on during the night, and he was fine with that. Think it helped that he’d seen it, because it’s difficult for him to understand if we only describe it in words.’
The information helped ensure that the parents felt secure enough to carry out the procedure at home with the support of HaH. A doctor gave the parents the results of the testing in a telephone call later. Most found that being given the information via telephone was straightforward and efficient, and that they received full information.
Two mothers felt it took a long time to get the results. One of them had also called to remind them to send an answer. Another felt that things happened quickly. One mother said she had been informed that the testing had not been completely successful, and she felt that the hospital questioned whether they had done it correctly. Another mentioned that they had been excited about whether they had managed to do it correctly, and it was good to have that confirmed.
The child in focus, but more responsibility for the parents
The children were met on their own terms
Several of the mothers highlighted the advantage of the child being able to have a normal day with normal everyday tasks. One mother said that her child had spent a lot of time on hospital appointments, and that they wanted to reduce these to a minimum:
‘Now he could be out playing with the other children up until about ten minutes before they arrived. So he could enjoy the whole of the afternoon, which he couldn’t have done if we’d had to go in there (to hospital). So that was amazing.’
The HaH nurses were described as calm, friendly, fond of children and pleasant. The informants emphasised that the nurses were clearly used to working with children and families. In a family with siblings, the mother described the experience as problem-free. The mothers said it was crucial that the health personnel talked to the child and took good time to show the equipment and explain its use before it was attached. One of the mothers talked about how she experienced the atmosphere:
‘The nurse who came was very calm and pleasant, easy to talk to and she joked with him a bit. So there was a very good atmosphere here. It wasn’t chaotic and busy as it can be at the hospital where they have to hurry on to the next patient.’
Several said that their child was a bit sceptical but that the nurses used humour when attaching the equipment. Some of the mothers pointed out that the child thought it was exciting and fun, and that they appreciated the present they were given later. Most found that their child generally slept well during the night, and that this was because they were sleeping at home in their own bed. Some mentioned that the child had been restless in their sleep but claimed that this would probably also have been the case in hospital.
The length of time the child had previously spent in hospital varied. Most were not afraid of being in hospital, but all the waiting could be very boring. Two mothers described how their child had had unfortunate experiences in hospital and for that reason it was good to get help at home:
‘He’s much more scared [at the hospital] and hates having blood tests. We’ve had to work a lot with hospital-related anxiety since he was tiny. So I found that when he was at home, I didn’t see as much of that. Here at home, I don’t believe he thinks about the blood tests, or anything like that. So I really think it’s an excellent solution.’
More responsibility for the parents
Parents found that the task of having to check the equipment during the night was manageable. The only thing that was a bit of work was fixing the equipment if it slipped out of place during the night:
‘He slept well the whole night, …that wasn’t a problem. It was worse for us parents, we were really tired the day after because we had to get up so many times just to check the equipment. He slept very restlessly so part of the equipment fell off during the night and we had to fix it. But that would happen in hospital as well.’
Otherwise the parents mostly felt secure and found the extra responsibility worthwhile because the child could stay at home. One mother said that she could not get in contact with the personnel when she had some questions after they had left. Another mother said that she was positively surprised that the nurse returned to help when technical problems occurred before the child went to bed.
The mothers described being at home as comfortable, practical and time-saving. They appreciated that not everything could be done at home but were positive to getting help at home when it was possible. One mother mentioned that on one occasion the nurse did not seem to be confident about using the equipment.
Discussion
Information and preparations for parents and children
The results may indicate that information about referral and the option of carrying out sleep testing at home is not always presented well enough to the parents. Health personnel are required to give information about the types of health care available in addition to different examination and treatment methods (24). The amount of information the families had received about the procedure itself also varied. Good information and preparation of the procedures beforehand are a source of mastery and security, for both children and parents (8, 25).
Aasen et al. (14) found in their study that the parents of children receiving health care via HaH had a strong need for information in the form of active involvement. Park et al. (26) found that information was an important measure in family-centred care.
The mothers felt that they received too little information at times. Nevertheless, they were positive to carrying out sleep testing at home because it saved them both the time and stress that hospital admission entails: they often have to travel, take time off work, kindergarten or school. The offer of sleep testing at home means that their wish to avoid these could be met. An important principle in the family-centred approach to care is that the family’s overall needs and wishes are given a high priority (8).
The Patients’ Rights Act (27) makes it clear that the patient has the right to be involved in the implementation of the health care given. The closest relative of children under the age of 16 has the right to be involved together with the patient, but it is made clear that the child’s opinion carries most weight.
Children may feel insecure when people they do not know enter their home (28). They need preparations that are suited to their developmental level (25). It emerged that the mothers themselves had prepared their children by using explanations that the children could understand. Studies of the parents of premature children who had received support from HaH show that being allowed to participate activates the family’s resources and normalises family life (29).
The fact that the parents themselves give information appropriate for their child prior to a procedure could perhaps be used as a more deliberate information strategy when offering such services in the home. If so, this would mean that the parents should receive information well before the procedure is carried out.
Health care on the family’s terms
The mothers highlighted the importance of the nurses taking good time to talk to the child and showing them the equipment before it was attached. This finding is in keeping with the findings of other Nordic studies. (14, 15). While the best interests of the child must be the primary consideration for all healthcare (4, 30), it is a moot point whether it is right to place responsibility for carrying out various procedures at home on the parents (14, 16, 31).
Family-centred care supports the family’s central role in a child’s life (8, 9). Sleep testing at home can be performed as long as the parents find it a good alternative. The mothers in our study stated that they would prefer sleep testing to be carried out at home even if they were given more responsibility. Earlier qualitative studies of HaH have pointed out that being able to stay at home strengthens family and everyday life (28, 32).
This finding was confirmed by the mothers in our study. They highlighted the importance of the family having the most normal everyday life possible, with the child able to go to school or kindergarten and be together with their siblings and friends. Several of the mothers said that the child slept well at home. Having the most normal everyday life possible and sleeping in familiar surroundings can promote good sleep. Having fixed routines is an important principle for good sleep (33), and in return can facilitate sleep testing that reflects the child’s normal sleep.
Strengths and weaknesses of the study
We have given the most accurate and precise description possible of the project’s method in order to strengthen the study’s credibility. A larger and more complex sample might have provided greater breadth in the dataset. Meanwhile individual interviews are regarded as a robust data collection method because they elicit the nuances of the informants’ experiences (21).
The different perspectives that emerged during the interviews demonstrate the information power of the data, and in our view, the research question was answered (34). In addition, we found that earlier research supports the empirical data. Both authors performed the analysis, and this strengthens the findings (18).
Conclusion
The mothers agreed that carrying out sleep testing at home under the auspices of HaH was a good alternative to traditional admission to a hospital ward. They found the referral routines somewhat unclear. The information they were given was crucial for them assuming responsibility for carrying out the procedure at home. They felt it was safe to do this even though it meant staying awake at night and being responsible for the equipment. In their view, the fact that the HaH nurses took the time to develop a relationship of trust with the child was essential for a positive experience.
Our findings can help shed light on parents’ experiences of sleep testing at home. In future studies, interviews with children and siblings can be an important source of information in the future development and planning of health services to children and their families.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge



Comments