Use of restraint in the paediatric ward – a survey study
Summary
Background: The term ‘restraint’ has a broad meaning. It is difficult to know what the concept entails, and this can lead to it being normalised and used more often. We know from experience that restraint is frequently used in paediatric wards, and we examine this in the article. Use of restraint can be considered a violation of children’s rights, and it is important to examine the frequency of restraint and the influencing factors in order to be able to reduce its use.
Objective: The purpose of the study was to survey registered nurses’ experiences with the use of restraint in a selection of paediatric wards in Norway. We also investigated which factors influence the decision to use restraint; factors that both support and do not support its use.
Method: The study is a descriptive cross-sectional study. All registered nurses at the selected paediatric wards (n = 250) were invited to participate in the study and were sent a questionnaire. Descriptive analysis was performed using SPSS version 27.1 and Excel version 16.47.
Results: The questionnaire was answered by 117 registered nurses (47% response rate). The analyses show that 96% of the study participants have used restraint in the last twelve months, 47% reported using restraint occasionally, while 43% used it weekly. Restraint is most often used on children below the age of four. Use of restraint was most frequently reported for invasive procedures and urgent procedures, but also in very young children and children with little ability to understand. The most frequently reported measures used to reduce restraint are parental involvement, distraction and information.
Conclusion: The nurses reported that restraint, and particularly physical restraint, is used often. The study shows that the nurses work in the child’s best interest as factors such as heavy workload and understaffing rarely influence the decision to use restraint. We asked whether the participants felt they had the opportunity to reduce the use of restraint, and the majority answered ‘occasionally’. The results show that there is a need to reduce the use of restraint in general, and that more focus is needed on implementing and using methods that can reduce restraint.
Cite the article
Rønningen R, Eilertsen . Use of restraint in the paediatric ward – a survey study. Sykepleien Forskning. 2023;18(91598):e-91598. DOI: 10.4220/Sykepleienf.2023.91598en
Introduction
In 2020, 26% of all Norwegian children between the ages of 0 and 19 visited hospital at least once (1, 2). Children are a vulnerable group, and they often have to undergo multiple procedures in hospital, which they do not always understand. This can make them feel frightened (3, 4).
Many paediatric admissions are emergency admissions. It is therefore difficult to prepare the family in advance. Parents can project their own feelings onto their children, and it is therefore important to provide reassurance for the whole family. The children, parents and siblings can have crisis reactions in connection with hospital admissions (4). Children’s fear of hospitalisation can result in them resisting procedures (3, 4), which in turn can lead to restrain being used as the procedures are often necessary (3).
Background
Results from studies in other countries show frequent use of restraint on children who are hospitalised. Restraint is frequently used as children undergo stressful but often necessary procedures without understanding why (5–7). The method involves holding the child against his/her will (3, 8) and is often used on very young children (6–8).
There are several types of restraint (3): physical restraint involves the child being held still, psychological restraint involves persuasion (3, 9), manipulation or bribery, and clinical restraint is the administration of medication against the child’s will (3).
‘Restraint’ has a broad meaning and is often explained by terms such as immobilisation, restricting movement and holding still. These terms are perceived as less impactful. They make the phenomenon seem harmless and normalise the use of restraint. Consequently, they can increase the frequency of restraint (6, 8, 10). Children’s and parents’ reactions can help us confirm whether the procedure requires the use of restraint or not. Carrying out a procedure on a child showing strong resistance can be described as use of restraint (5, 6, 10).
Healthcare personnel disagree about what actions constitute ‘restraint’ (5, 6, 10). Some feel that they are not using restraint if the procedure is considered necessary, which it often is (7, 10). Uncertainty about the phenomenon can lead to uncertain reporting of its use.
Restraint should only be used when it is in the child’s best interest, which means working to safeguard the child’s autonomy and support its decisions (7, 10, 11). It can be difficult to adhere to this, as children are not defined as competent to consent and often oppose procedures due to uncertainty (3, 4). Restraint is therefore sometimes used independently of consent and is considered by some to be routine when performing procedures (6, 11, 12).
Few prevalence studies have been published on the use of restraint in paediatric wards, which may reflect the uncertainty surrounding the concept. In an international survey, 48% of healthcare personnel stated that they use restraint often (5). Physical restraint is the most common method (9), with a prevalence of 11% to 68% globally (5,7). Use of restraint also depends on the type of procedure: intravenous cannulation led to use of restraint in 72% of cases (8). No data have been found on this in Norway.
The use of restraint can be traumatic for everyone involved (6, 9, 10). In some studies, restraint is described as taboo (6, 10, 12) and should be used as little as possible (5, 7, 10). Children can find the act of being restrained worse than the procedure itself (7). It is difficult to know the consequences of restraint (12), but some research indicates that it can diminish a child’s ability to build relationships (7), and cause psychological distress and a fear of procedures (6, 8).
Children under the age of 16 are not competent to consent, and their parents are therefore responsible for giving permission to carry out procedures (13). This can increase the frequency of restraint as the parents may think it is better to simply carry out the procedure, regardless of the method used. It is recommended that children be informed about health interventions from the age of seven, and that their opinion on this be given weight (13). Consent is rarely sought before restraint is used. The parents are sometimes asked, but only verbally in most cases (5, 7, 12).
Restraint is used for many different reasons: young age of the child and thus little understanding and cooperation, urgent procedures, poor staffing, simplification of everyday practice for registered nurses (RNs) (5–7) and parents’ wishes (5, 7, 11). There are also several options for reducing the use of restraint, for example, preparing the child (9–11), including the child in the procedure or distracting the child (3, 8, 9).
The need for restraint can also be minimised by parental participation (5, 8, 11). Nevertheless, it is often the parents who restrain the child (9, 11, 12). It is recommended that RNs build a relationship of trust with the child before carrying out any procedures, thus reducing the need for restraint (9, 12). Such a relationship can be built by working in a child-friendly way, such as interacting with the child and taking his/her ability to deal with the situation into consideration (9).
The lack of legislation, procedures and guidelines on the use of restraint in children or the lack of knowledge about these can lead to uncertainty among RNs (3, 8, 10). Training and education in the use of restraint should be offered and guidelines devised in order to reduce its use (3, 8, 11).
There is a considerable need to explore restraint more thoroughly. RNs use restraint frequently, and their broad knowledge of the subject means that an emphasis is placed on their perspectives on restraint. In order to prevent and reduce the use of restraint, it is crucial to examine the phenomenon and prevalence of restraint, as well as which factors influence and reduce its use. Point prevalence surveys are considered particularly important as no such studies have been conducted in Norway. Previous research shows that it is possible to reduce the use of restraint (6, 8, 9).
Objective of the study
The objective of the study was to survey RNs’ experiences with the use of restraint in paediatric wards in Norway. The secondary purpose was to examine which factors influence the decision to use restraint, both those that support and do not support its use. Based on this, we formulated the following research questions:
- How often do RNs use restraint in paediatric wards in Norway, according to their self-reporting of the phenomenon?
- What factors affect the decision to use restraint?
Method
Design
The study was conducted as a cross-sectional study, and the data were collected in the spring of 2021.
Sample
The survey was conducted at a regional, university hospital in Norway. The sample was selected through continuous inclusion, where all the RNs in the paediatric department participated. Staff at the neonatal intensive care unit were excluded. The inclusion criteria were RNs who had experience in working with children.
Data collection tool
We used an online questionnaire. Few questionnaires have been developed that deal with the use of restraint on children, and no validated Norwegian questionnaires were found that were relevant to the study. We found two questionnaires from other countries which, with the authors’ agreement, were combined (5, 8). Kirwan and Coyne’s survey has been assessed (8) for face validity.
We tailored the questionnaires according to the guidelines of the International Test Commission (ITC) (14). This involved removing and adapting questions and response alternatives, and making all the questions closed-ended, as recommended for quantitative studies (15, 16). These changes are considered simple adaptations, and the content of the questionnaires is regarded as unchanged.
The questionnaires were translated from English into Norwegian. The translation was based on a four-step process: two independent translations from the source language to Norwegian, a summary of the result, translation from the target language to the source language, and finally an assessment of all versions of the translation (17, 18).
The questionnaire was then pilot tested by five independent RNs who had experience in working with children. The pilot testing led to some changes in wording, and we added a supplementary study-specific form to elaborate on the purpose of the study. The supplementary form consisted of questions about the age of the participants, whether they believed that steps could be taken to reduce the use of restraint in everyday practice, and how often they themselves used restraint.
Data collection
The survey was sent out via email using an online, anonymous survey tool (Nettskjema). We conducted the survey in collaboration with section heads at the paediatric department.
A total of 250 RNs received an email giving information about the study, and five days later an invitation to participate was sent out. Reminders were also sent out and the study was advertised to generate interest among participants.
Analysis
The data collected were transferred from Nettskjema to IBM SPSS Statistics, version 27.1. We used categorical variables that were named and coded before the data transfer. Descriptive frequency analyses were performed to describe the study’s variables (15, 16).
We created tables in Excel, version 16.47. Two statisticians were contacted for guidance on analysis. We investigated factors associated with the increased use of restraint using a rating scale and a numerical scale in which the influence of the factors was given on a scale from zero to ten. This resulted in correspondingly similar responses, and the results from the numerical scale are presented.
Research ethics considerations
The study was approved by the Norwegian Centre for Research Data (NSD) (reference number 566563) and the hospital’s R&D department before the start of the study. All participants were given information about the study, and answering the questionnaire was regarded as informed consent.
Results
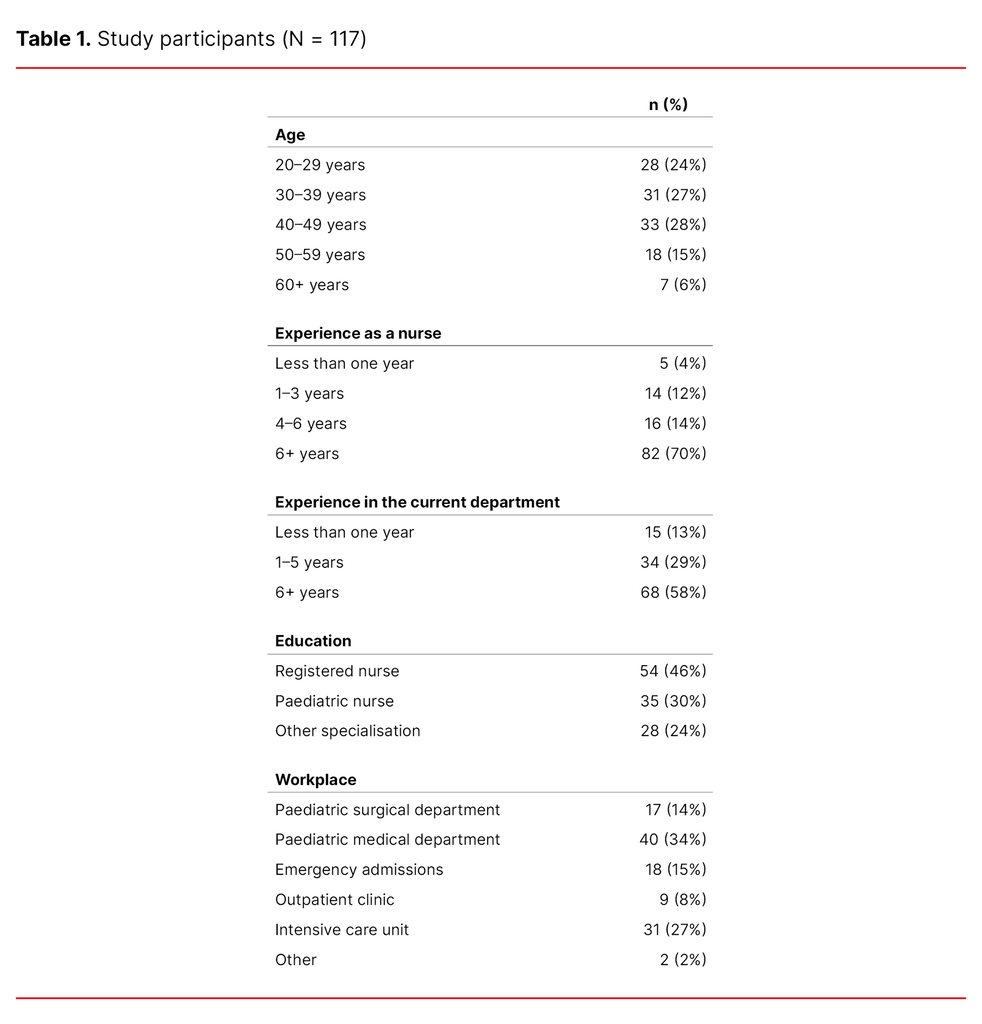
The study had a response rate of 47 (N = 117). The age of study participants was evenly distributed, and the majority had over six years of experience in a paediatric ward. All departments included were represented in the study. Table 1 shows a description of the RNs who participated in the study.
Prevalence of restraint
The results show that 96% of the RNs (n = 112) used restraint. More specifically, physical restraint was used by 96% of the participants (n = 112). The figures for clinical restraint and psychological restraint were 86% (n = 101) and 63% (n = 74), respectively.
The majority stated that they use restraint sometimes (47%, n = 55), 42% stated that they use restraint often (n = 49), and 11% very often (n = 13). The percentage who never used restraint was 0 (n = 0). The main group stated that restraint was used weekly (43%, n = 50). According to 81% of the RNs, restraint is sometimes used unnecessarily (n = 95).
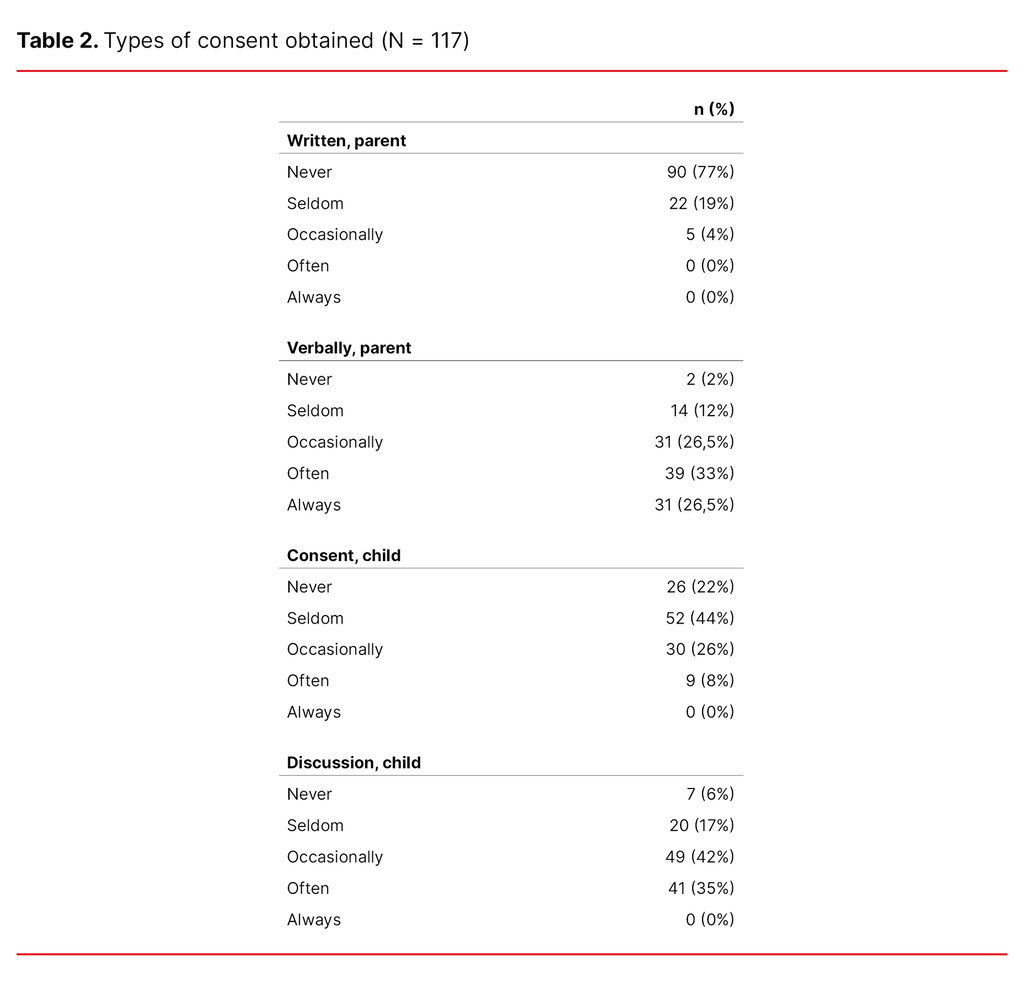
Use of restraint is not documented according to 49% of the RNs (n = 57), while 38% said it is mentioned in the reports (n = 44). Restraint is documented in writing by 24% of the participants (n = 28). Consent is seldom obtained before restraint is used (Table 2).
Factors associated with increased use of restraint
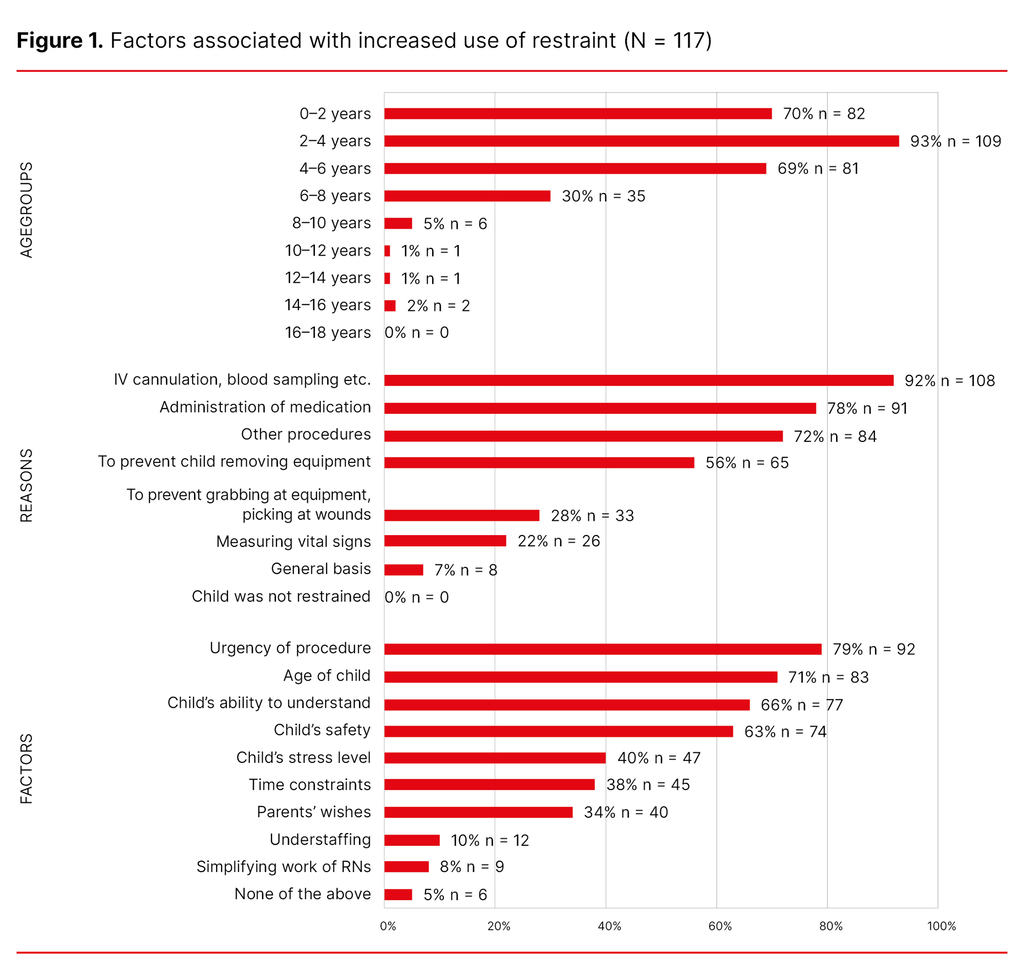
As shown in Figure 1, invasive procedures, administration of medications and performance of other procedures were ranked as the main reasons for using restraint. The highest ranked factors for increased use of restraint are if the procedure is urgent, and if the child is very young and thus has little ability to understand. Restraint is most frequently used on children below the age of four.
Factors associated with reducing the use of restraint
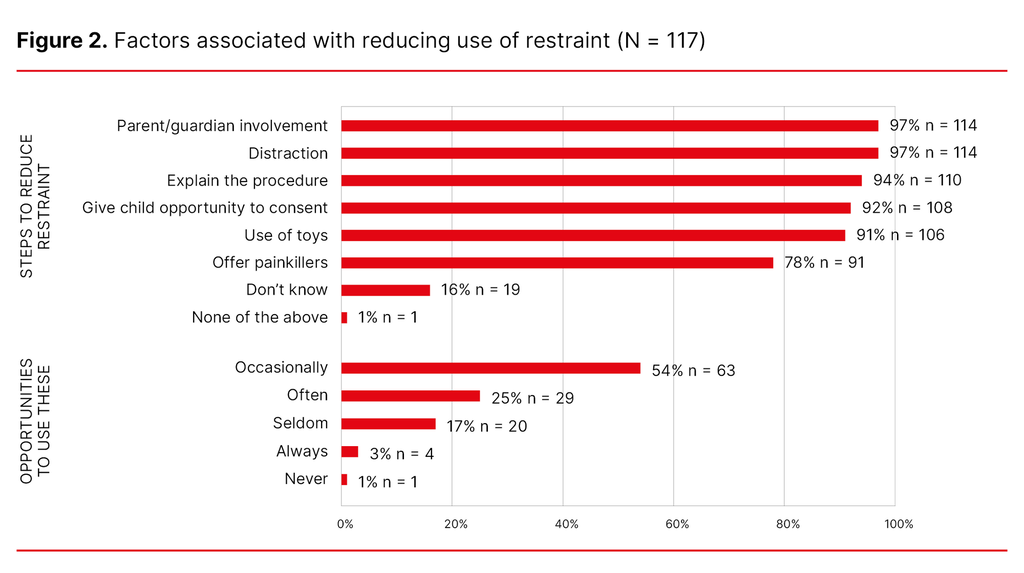
Factors associated with reducing the use of restraint and the opportunities to use such methods are shown in Figure 2. Parents are often present when children are restrained, according to 55% of the RNs (n = 64), and 36% stated that the parents sometimes participate in the restraint (n = 42). Sixty-seven per cent stated that when the child has to be restrained, the healthcare personnel and the parents work together (n = 78). Parental participation was perceived as positive by 60% of the participants (n = 70).
Fifty-three per cent of the RNs (n = 62) were unaware of any guidelines explaining the use of restraint on children, and 40% had not familiarised themselves with procedures and guidelines on the use of restraint (n = 47).
Mapping tools are considered useful by 73% of the participants (n = 86), while 87% do not use them (n = 102). Eighty per cent (n = 94) reported having no training in the use of restraint, and 90% think that training should be provided (n = 105).
Discussion
The study shows that restraint is used frequently, and it gives us a good insight into which factors increase and decrease its use. It also shows that consent is seldom obtained.
The study participants reported that they are unsure what the term ‘restraint’ entails. Previous research shows that the term has a broad meaning (6, 8, 10). This and the fact that the subject can be considered taboo (6, 10, 12) are challenges to the study and may compromise the credibility of responses.
The results of our study show that restraint is mainly used when it is needed and when it is in the best interests of the child. This finding is not consistent with other research, which describes frequent use of restraint regardless of need (6, 11, 12).
The concept of ‘the child’s best interest’ is easy to understand (7, 10, 11). ‘Simply carrying out’ the procedure without distracting the child may also be justifiable under this principle, as to do so enables RNs to carry out the procedure more quickly, which in turn means that the child will be less impacted.
Prevalence of restraint
The majority of RNs in the study used restraint, and the majority used it weekly. This frequency is supported by Bray et al. (5), but the proportion who reported using restraint in our study is larger. As many as 48% of the participants in our study reported using restraint frequently.
Over half of the RNs in the study (63%) confirmed having used at least one type of restraint, including physical, psychological or clinical restraint. Physical restraint was used the most. The study participants reported that restraint was typically not used in all patients regardless of need, but that it was used when it was in the child’s best interest. However, they also reported that children were sometimes restrained unnecessarily.
It is difficult to know what the consequences of restraint might be (12, 13), but it has been shown to affect some children’s ability to build relationships (7). Children can find the act of being restrained worse than the procedure itself (7). This means that it should be used as little as possible, particularly in instances where RNs consider it unnecessary.
The results from this study show that parental consent was seldom sought, and when it was, it was only done so verbally, which is supported by previous research (5, 7, 12). In addition, the RNs reported that they rarely ask for consent from the child, which is also seen in previous research (5, 7, 12).
There are several reasons why consent is seldom obtained, such as lack of knowledge about the subject, but also difficulties in respecting the answer if the procedure is necessary. The consent process for the use of restraint on young children is difficult, as they are not competent to consent. Consequently, the responsibility for consent falls to the parents (13), and it can be difficult to know what the child wants.
Factors associated with increased use of restraint
The frequency of restraint increases if the procedure is urgent, or if the child is very young and thus has a reduced ability to understand and cooperate. These factors can also influence each other. The RNs also described how some parents want to carry out the procedures using restraint without trying to take steps to avoid it, which may be an indication that the parents want the procedures to ‘simply be carried out’ (5, 7, 11).
In addition to this, previous research also placed an emphasis on RNs’ habits, understaffing and simplification of RNs’ everyday practice (5–7). In our study, we did not find support for these factors, but the RNs stated that they did little to prepare the children and parents before procedures. This finding can appear contradictory and could be interpreted as the RNs being somewhat uncertain about their own use of restraint. Whether preparations are under-prioritised in a hectic working day can be debated.
The emphasis on the factors associated with increased use of restraint shows that the RNs in the study work for the child’s best interests and support the child’s autonomy, as they state that external factors such as understaffing and heavy workloads rarely influence whether restraint is used or not. The RNs reported that restraint was mostly used on very young children, often under the age of four, which the research supports (7, 8, 10).
Invasive procedures such as blood sampling, intravenous cannulation and such like are most often associated with increased use of restraint, and this is supported by Kirwan and Coyne (8).
Factors associated with reducing the use of restraint
Among the factors that can reduce the use of restraint, the study participants placed most emphasis on parental involvement and distraction, which is confirmed by other research (3, 9, 11). Information, preparation of the child (9–11) and inclusion of the child in the procedure (3, 8, 9) are further emphasised in the study and in other research. As described, parental participation is the most important factor in reducing the use of restraint.
The RNs in the study reported that the parents are often present during procedures, and that they sometimes help to restrain the child. Physical restraint is often carried out by healthcare personnel and parents together. Many parents dislike this task (10–12), which the RNs in the study respect to some degree.
The majority of the RNs reported that parental participation has a positive effect on the restraint situation, which can be interpreted as a distraction, as the parents know which measures will best distract their child and thus also reduce the use of restraint. This finding is supported by other research (5, 8, 11), while some studies indicate that parental participation can have both a positive and negative impact on procedures and use of restraint (5, 10, 11).
The RNs reported that preparing the child for the procedure is essential for avoiding the use of restraint, as supported by previous research (3, 8, 9). Nevertheless, the study shows that one-fifth of the RNs rarely discuss the use of restraint with the child in advance. The main group of admissions at the hospital in the study are emergency admissions. There is therefore less opportunity to prepare the child in advance, which could perhaps minimise the use of restraint. Using restraint without mentioning it first can break the relationship of trust between RNs, parents and the child.
Building relationships of trust prior to the procedure is considered essential (9, 12), and the RNs in the study only seem to partially comply with this. This finding shows one of the dilemmas of using restraint, as the RNs do not always have the opportunity to carry out the work as they wish. A possible reason for this could be their hectic working day. Nevertheless, the RNs in the study refute the idea that their hectic working day with little time to spare influences their decision on whether to use restraint or not. This inconsistency makes it unclear whether restraint could have been avoided to a greater extent.
The study did not directly examine the use of alternatives to restraint, but the RNs reported that they only occasionally have the opportunity to use such alternatives. A correlation can be seen between limited use of alternatives to restraint and lack of procedures and guidelines. RNs have a duty to familiarise themselves with such instruments. The majority of participants are experienced nurses who should recognise these restraint-reducing factors.
The study participants reported that there is little legislation and few procedures and guidelines on the use of restraint on children, which is confirmed in previous research (3, 8, 10). The majority of the RNs described that they were not aware of guides, guidelines or procedures on the use of restraint. The study results show that the majority of the participants use restraint, which may be linked to the lack of legislation and consequent uncertainty among healthcare personnel (3, 8, 10).
The majority of the RNs stated that they do not use a mapping tool for the use of restraint. The majority believe that such a tool would be useful and could limit the use of restraint, and this is also supported by previous research (5, 7, 11).
It can be difficult for RNs to use such tools if they have not been implemented in the department, but use and/or identification of needs can lead to such tools being implemented. The majority of the participants reported that they had had no training in the use of restraint and believed that they should have done. Training can reduce the use of restraint (3, 8, 11), and discussions should be held on whether such training should be given.
Methodology
This is a descriptive study, and the results cannot necessarily be generalised. Nevertheless, the findings provide a good overview of the phenomenon that may be of significance to future studies (15, 16). Questionnaire surveys provide an abundance of information (16), but the findings can be affected if participants do not give honest answers (15).
The study was conducted anonymously, which is a strength and increases the possibility of obtaining honest answers. It is recommended that validated questionnaires are used (15), but we did not manage to identify any such questionnaires. The survey used was pilot tested, which can also strengthen the reliability of the study (15, 16). We chose to include older literature as there is not much research in this field.
In the study, we included participants from different paediatric departments, which is considered a strength. The study was only conducted at one hospital. It would have been interesting to conduct the survey at several hospitals in order to strengthen the study and obtain broader knowledge of RNs’ experiences with this subject.
The response rate of the survey was 47%. Research shows that RNs can find the topic of restraint and discussions on this traumatising (6, 9, 10), and it is considered a taboo subject (6, 10, 12).
Attitudes on the subject can affect the participants’ ability to give honest answers. This phenomenon may also partly explain the low response rate, but a 50% response rate is considered normal in surveys (15). Unfortunately, the data were collected during a very busy period for the RNs, which may have affected the participation rate.
Conclusion
The RNs reported that restraint is used in paediatric wards at the hospital in the study. The majority of the RNs use restraint on a weekly basis. Physical restraint is used most frequently, and children under the age of four are most likely to be restrained. Invasive procedures and the administration of medication are the procedures that are mostly commonly associated with restraint. The factors that are most commonly associated with restraint are that the procedure is urgent and the child is very young, and thus also has little ability to understand.
Parental involvement, preparation and distraction are the most essential factors in limiting the use of restraint. These factors show that the RNs use restraint as a measure to safeguard the child’s best interests, and not on a general basis as previous research may suggest. The RNs reported that they only occasionally have the opportunity to use alternatives that can reduce the use of restraint. Changes are therefore needed to RNs’ working day.
The RNs at the hospital in this study are considered to be comparable to RNs in other hospitals in Norway. The knowledge generated in the study will also have value in other paediatric departments in Norway. Further research is needed into how alternatives to restraint can be implemented so that its use can be reduced. In addition, the importance of procedures and guidelines should be investigated.
The authors declare no conflicts of interest.
The Study's Contribution of New Knowledge

Comments