Intranasal dexmedetomidine is of benefit as paediatric premedication – from the perspective of anaestetic nurses
Summary
Background: Nasal administration of the drug dexmedetomidine is increasingly used for children who need sedation and premedication before anaesthesia and surgery. Midazolam, which currently is most widely used, is associated with a number of adverse effects. There is thus a need for alternative paediatric premedication to improve treatment provision.
Objective: To provide new knowledge on the properties of dexmedetomidine and how this drug is suited as premedication for children who will be given general anaesthesia, seen from the perspective of the anaesthetic nurse.
Method: We conducted semi-structured interviews. The sample consisted of six anaesthetic nurses from two day surgery units in two different hospitals. We analysed the data with the aid of qualitative content analysis.
Results: We identified two main topics: 1) Dexmedetomidine as premedication has favourable properties throughout the anaesthetic process. 2) Necessary precautions need to be taken throughout the anaesthetic process to ensure that no complications arise when dexmedetomidine is used as premedication. In general, the findings show that dexmedetomidine provides satisfactory sedation in the form of sleep preoperatively. It is found that the children are easy to wake up from their sedation. This means that the children need minimum exposure to stimulation before and during the induction of anaesthesia. However, the long onset time of dexmedetomidine necessitates interdisciplinary collaboration to achieve an efficient patient flow. The anaesthetic nurses did not describe any serious adverse effects of the drug.
Conclusion: New knowledge from the perspective of the anaesthetic nurses shows that dexmedetomidine is perceived as a suitable alternative to premedication for children. The disadvantages were described as minor when compared to the advantages provided by dexmedetomidine used as premedication, with favourable effects prior to, during and after surgery. The anaesthetic nurses faced some challenges in the use of dexmedetomidine at the start of the introduction process, but experience with the drug’s properties showed that to use it successfully and safely, necessary precautions must be taken throughout the anaesthetic process. The findings show that new procedures should be introduced by way of internal pilot projects.
Cite the article
Berland L, Bakkalia I, Dysvik E. Intranasal dexmedetomidine is of benefit as paediatric premedication – from the perspective of anaestetic nurses. Sykepleien Forskning. 2018;13(71340):e-71340. DOI: 10.4220/Sykepleienf.2018.71340en
The drug dexmedetomidine is increasingly used for sedation and premedication in children (1). Dexmedetomidine enables a saving on analgesic and anaesthetic agents, has a minimal effect on respiration and can be administered by different routes (1–3). The intranasal route is minimally traumatic, and dexmedetomidine is taste-free, odour-free and painless when used on the nasal mucous membrane, and the drug is therefore well tolerated by children (4, 5).
The benzodiazepine derivate midazolam provides good sedation and thus reduces anxiety, and is the most frequently used drug for paediatric premedication (2, 6, 7). The adverse effects of midazolam, such as foul taste, stinging pain when used intranasally, respiratory depression and in some cases increased agitation, nevertheless makes it a suboptimal choice (1, 3, 8). There is a need for an alternative paediatric premedication to improve treatment at the pre-, per- and post-operative stage (9).
Surgery invokes anxiety
Research has estimated that 40–70 per cent of all children of pre-school age experience anxiety in connection with a surgical procedure (1, 3, 8). Anxiety may complicate the induction of anaesthesia, which is stressful for the child, the parents and the anaesthetics team. The parents’ experience at this stage has a significant effect on their satisfaction with the treatment programme (7, 9).
Reducing the children’s anxiety preoperatively helps prevent complications. A high level of anxiety and difficult induction of anaesthetics are a risk factor for post-operative complications such as agitation, more pain and long-term, negative behavioural change such as bedwetting, reduced appetite and temper tantrums. Such complications may delay the departure from hospital and rehabilitation (7, 10, 11).
Teamwork
The anaesthetic nurse and the anaesthesiologist constitute an anaesthetics team that collaborates closely in a complex and dynamic environment, with overlapping job tasks. The doctor holds medical responsibility in the team (12).
The anaesthetic nurse has an independent function and an expanded nursing competence that requires specific technical and non-technical skills. This competence is required to be able to observe, identify and assess different situations and take action to meet the complex needs of the patient who is about to undergo surgery and anaesthesia. The objective is to ensure patient safety and appropriate professional practice (12, 13).
Objective of the study
Literature searches revealed a number of quantitative studies describing the use of dexmedetomidine as paediatric premedication. Various academic articles indicate that dexmedetomidine is well suited as premedication and sedation for children down to the age of one year. Research also shows that the use of dexmedetomidine has positive effects at the post-operative stage, including calmer and less painful awakenings (1, 3, 8).
However, we found no studies that had taken a qualitative approach to this question. Demands for appropriate professional procedures must be grounded in evidence-based practices, meaning that professionals make use of a variety of knowledge sources in the practice of their profession (14–16). For procedures to be changed, they need to be perceived as more suitable than those that are established.
Based on the above considerations, the objective of our study was to explore the experiences of anaesthetic nurses, in order to contribute new knowledge about the properties and suitability of dexmedetomidine as paediatric premedication. These aspects form the backdrop to the following research question:
- What experiences do anaesthetic nurses have with the use of intranasal dexmedetomidine as premedication at the pre-, per- and post-operative stage in children who will be placed under general anaesthesia?
Method
Design
We used a qualitative, exploratory design that involved semi-structured interviews with anaesthetic nurses. This method is appropriate to capture the participants’ personal experiences by taking an open view (17, 18). The study is based on a phenomenological-hermeneutic tradition, in which reality is described as diverse and subjective, and findings are created in interactive processes. On the other hand, findings must be interpreted in light of relevant studies and the researchers’ preconceptions to obtain a more comprehensive understanding (17).
Sample
The goal of qualitative research is to include participants that can provide the richest possible descriptions in order to elucidate the research question (17). Contact persons in the hospitals recruited the participants based on the following inclusion criteria:
- must be an anaesthetic nurse with at least one year of experience
- works with children on a routine basis
- possesses clinical experience with intranasal administration of dexmedetomidine
- includes both genders
Based on the inclusion criteria, six anaesthetic nurses were asked to participate in the study, all of whom assented. They made up the strategic sample on which the data collection was based. Average clinical experience as an anaesthetic nurse, from work with children and the use of dexmedetomidine as premedication amounted to 14.8 years (3–21 years), 16.3 years (3–21 years) and 2.2 years (0.5–4 years) respectively.
The anaesthetic nurses were recruited from day surgery units in two Norwegian hospitals. The units had been established three and seven years ago respectively, and consisted of five to six operating theatres with appurtenant pre- and post-operative units. In general, the personnel was permanently linked to the departments, and surgical interventions included otorhinolaryngology, gynaecology, thoracic and endocrine surgery, orthopaedics and general surgery. Both departments operated on more than 800 children annually, mainly related to ear, nose and throat conditions.
Ethical considerations
The project is approved by the Norwegian Centre for Research Data (NSD) (project no. 50198) and by the heads of research in the hospitals. Prior to the interviews all participants received written information about the project accompanied by an invitation to participate in the study. They were informed about their right to withdraw at any time with no repercussions. They accepted to participate by coming for an interview.
All information about the participants was treated as confidential, in line with the NSD guidelines and principles of research ethics. The participants were coded with random numbers ranging from one to six, and all data were anonymised.
Data collection and analysis
We collected the data in the autumn of 2016 with the aid of personal in-depth interviews conducted in the participants’ workplace. A semi-structured interview guide (Appendix 1) was used to focus the interview and encourage the participants to speak as freely as possible (17). The interviews lasted from 30 to 60 minutes. We used a digital audio device to record the interviews, which were subsequently transcribed.
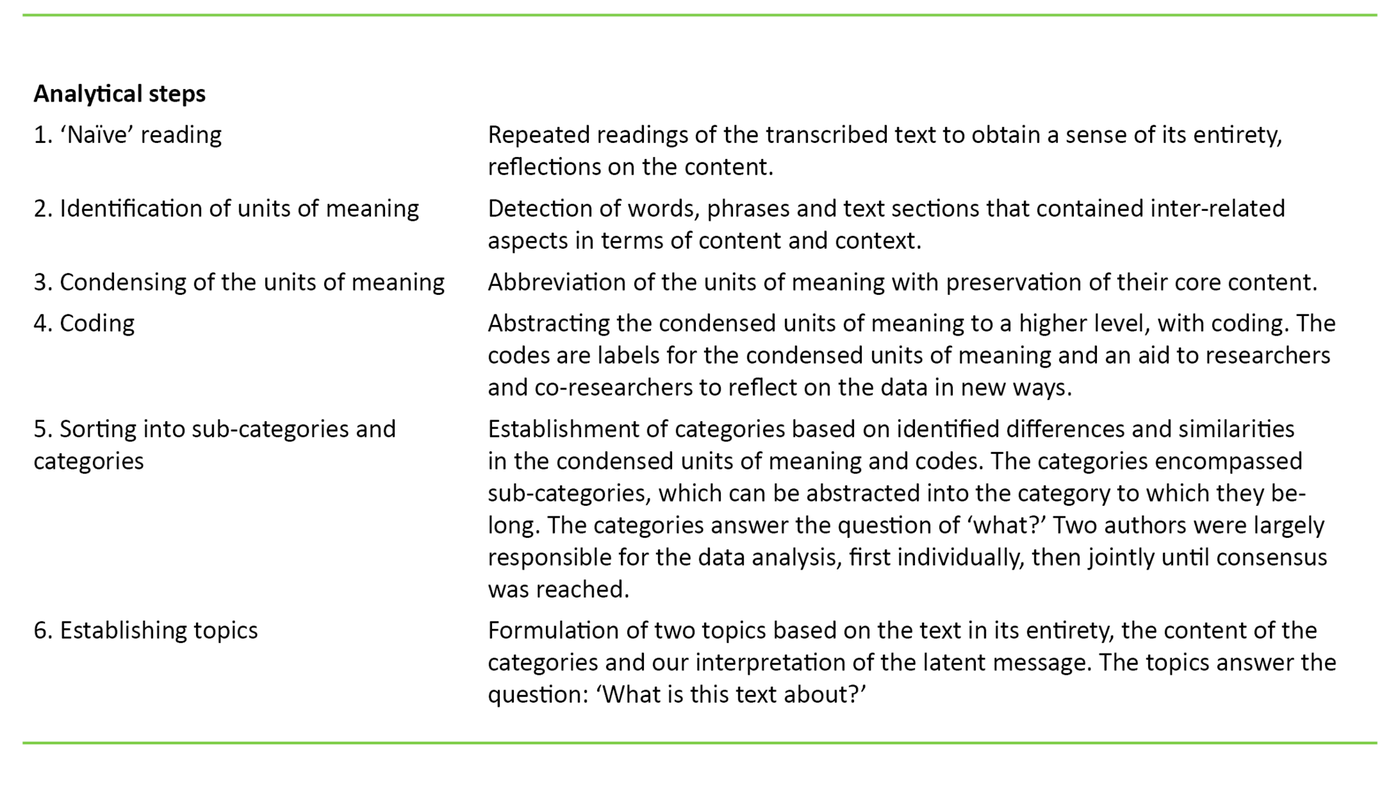
We analysed the data in light of Graneheim and Lundman’s (19) qualitative content analysis through a six-step abstraction process (Table 1). The text was divided into four natural domains in accordance with the three stages of the anaesthesia process plus the induction stage, and these constitute the units of meaning in the text.
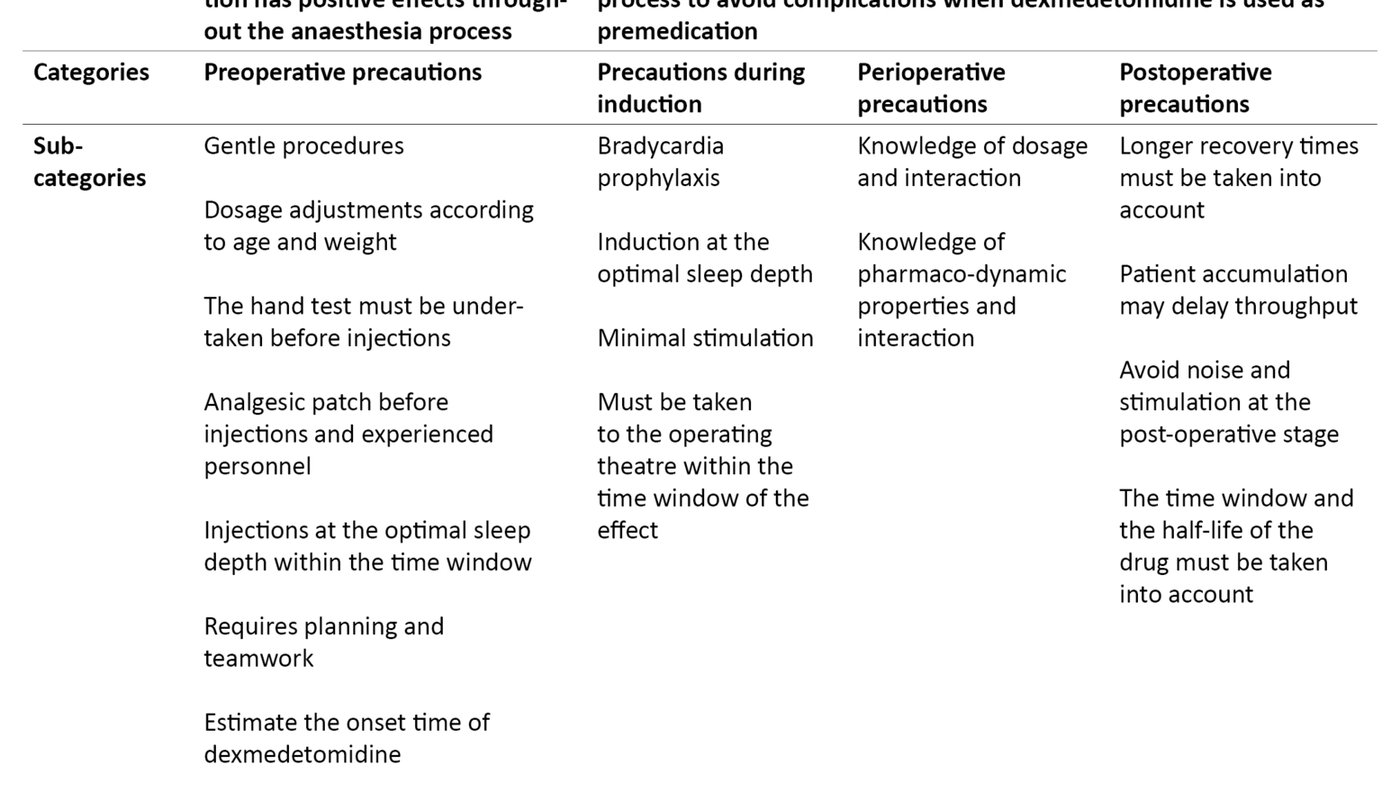
Through this abstraction process two main topics emerged: 1) dexmedetomidine as premedication has favourable properties throughout the anaesthetic process, and 2) Necessary precautions need to be taken throughout the anaesthetic process to ensure that no complications arise when dexmedetomidine is used as premedication (Table 2).
Results
Pre-operative experience
The anaesthetic nurses in both units described how dexmedetomidine was introduced after an intra-departmental pilot project. Participant 4 emphasised the importance of preparation: ‘It was well accepted by everybody, both in terms of the training and the ‘internal research’, where we compared children who had received dexmedetomidine, midazolam and nothing.’
Some challenges were encountered initially, as described by Participant 2: ‘Of course there was a breaking-in period concerning the dosage and timing, but it was well received. The favourable effects manifested themselves early.’
The anaesthetic nurses believed that the successful introduction of the new drug was largely due to the fact that the process was clinically endorsed by the unit’s anaesthesiologist. Participant 3 noted: ‘It’s essential to have an authority in the professional group when starting something new.’
The anaesthetic nurses had observed that dexmedetomidine induces sleep. Participant 2 gave an account of the following experience: ‘The children receive it, and when it takes effect they fall asleep ... You can insert a cannula, take them to the operating theatre and initiate anaesthesia without them noticing. But little time must elapse once they have fallen asleep.’
All participants found that the children could be woken up and had to be exposed to as little stimulation as possible. Participant 3 described it thus: ‘It’s an art to ensure that they do not wake up ... Having permanent staff who know how this works is an advantage ... It works really well now.’
Positive effects for patient flow
Experience indicated that the onset time for dexmedetomidine varied from 20 minutes up to one hour. This long onset time might delay patient flow in the morning hours. Participant 6 said: ‘The first child in the morning is a challenge. You must take the time needed and wait for the effect. For this you need a well-functioning system ... I nevertheless feel that I have a better daily situation with the children now.’
Participant 5 had the following experience: ‘The optimal time to administer dexmedetomidine is one hour before the surgical procedure.’
The anaesthetic nurses felt that interdisciplinary collaboration was crucial to achieve an efficient patient flow. Participant 2 described it thus: ‘The intensive-care nurses in the post-operative ward administer dexmedetomidine to the children when they arrive in the morning. They call us once the child has passed ‘the hand test’. Then, they are in a deep enough sleep to have an injection.’
Participant 5 gave this description: ‘We have a very good plan for solving this ... Everybody is involved. Collaboration is easy here, compared to in a large department.’
Despite the long onset time, the anaesthetic nurses found that using dexmedetomidine had a positive effect on patient flow. Participant 3 had the following experience: ‘The gain lies in the shorter induction time.’
Negative experiences
Negative experiences gathered by the anaesthetic nurses were associated with some cases of unsatisfactory effect. Participant 3 said that: ‘It would be those who wake up and are agitated. It’s crucial to bring them into the operating theatre within the time window.’
No experiences of serious adverse effects were described. Participant 4 had observed the following: ‘Once they have received the dexmedetomidine, the children turn pale around the mouth. They have a brief drop in oxygen saturation, although it never falls below 95 per cent.’
It was clear that the anaesthetic nurses saw dexmedetomidine as a better alternative than midazolam as a paediatric premedication. This was confirmed by Participant 4: ‘The nurses in the post-operative ward do not want to revert to midazolam.’
Experiences during induction
The anaesthetic nurses perceived the inductions as gentle and safer than with awake and frightened children. Participant 3 described it thus: ‘The induction is perceived as very positive. A calm, sleeping child provides for a much better overview compared to previously, when this often involved quite a struggle. Safety is good ... Compared to previously, it’s a new era.’
A general experience was that most children went from ‘sleep to sleep’, but this was contingent on minimal stimulation. Participant 5 explained: ‘The induction goes very gently. Only a pulse oximeter to begin with. We hold the mask lightly over the face so as not to wake them up. Once they are under full anaesthesia we move them to the operating table.’
The participants felt that most parents were satisfied. Participant 1 said: ‘Fewer parents leave the operating theatre in tears, because they feel that we are in control. They see a child who sleeps his or her way into anaesthesia ... I believe they see us as more professional than before ... We provide a system that makes me proud.’
Perioperative experiences
All participants noted that dexmedetomidine can induce circulatory fluctuations, and bradycardia in particular. Participant 2 described it thus: ‘There’s been talk about bradycardia, and we administer Robinul prophylactically during the induction, but I don’t feel that this is a major problem.’
All participants noted the potentiating properties of dexmedetomidine, meaning that this drug amplifies the effect of other drugs, which in turn means that less of these can be used. Participant 6 nevertheless found: ‘It reduces the use of opioids, but I can’t say that I notice anything during the surgery. We use approximately the same TIVA (total intravenous anaesthesia) settings for all patients. It works well.’
Post-operative experiences
The participants described a close, interdisciplinary collaboration in the day surgery units where the children stayed in the pre-, peri-, and post-operative stages. All participants shared the experience that the recoveries were characterised by less crying, agitation and pain. Participant 1 gave the following account: ‘It’s just wonderful. It’s so different. The children are sleeping and are OK ... The goal is for them to sleep through the distressing phase of recovery.’
In the experience of Participant 5, certain precautions nevertheless needed to be taken. ‘Not too much time should elapse from the administration of dexmedetomidine until the child goes into surgery and comes to the recovery unit. And the children must have the opportunity to wake up quietly.’
The anaesthetic nurses had observed that the children slept longer post-operatively after having been given dexmedetomidine as premedication. They did not believe, however, that this entailed any significant consequences for patient turnover. Participant 4 said: ‘The disadvantage is that there may be a backlog in the post-operative ward, but it’s not a major problem.’
Discussion
The objective of this study was to investigate the experiences of anaesthetic nurses at the pre-, peri‑, and post-operative stage with the use of intranasal dexmedetomidine as premedication for children who will be placed under general anaesthesia. In the discussion we will mainly focus on the pre-operative stage, because this stage is considered critical and the most comprehensive findings are also related to this stage.
Pre-operative experiences and experiences during induction
The pre-operative stage is challenging and encompasses the time from when the patient is admitted, premedication is administered and anaesthesia is induced (20). The anaesthetic nurse focuses on observing, identifying and assessing the child’s needs and on implementing measures to ensure that the treatment programme is individually adapted to the greatest possible extent. The objective of these measures includes ensuring patient safety and appropriate execution of tasks, thus to avoid adverse events (12, 13).
The anaesthetic nurses included in this study had observed that dexmedetomidine induced good sleep preoperatively when sufficient time was allotted to let the drug take effect. When it worked as intended, the children slept through the insertion of a venous cannula and the induction of anaesthesia. The informants did not describe any adverse effects in the form of respiratory depression or circulatory disturbances that required treatment.
The anaesthetic nurses reported positive experiences when dexmedetomidine ‘worked as intended’. They nevertheless described a number of challenges associated with dexmedetomidine used as premedication. Issues included absent and variable effects and onset times with identical dosages, especially at the breaking-in stage when the drug was unfamiliar to them. The literature indicates that in order to be effective, premedication should have a rapid and reliable onset (1).
The participants’ experience of varying effects and onset times can be related to the fact that the drug is administered via the intranasal route, which gives a more unreliable onset than intravenous administration, for example. Knowledge about pharmacokinetics and pharmacodynamic properties is therefore essential when anaesthetic nurses administer drugs, including with a view to patient safety (21, 22). Provision of individually adapted dosages and prevention of adverse events should be a goal (21).
Easy to wake up
All of the anaesthetic nurses described how the children could easily be woken up from sedation with dexmedetomidine. For example, they needed to find the optimal time and the best procedure for inserting a venous cannula and starting the induction of anaesthesia without the child waking up. According to the participants, this timing was ‘an art’.
According to Yuen (23), sleep induced by dexmedetomidine resembles regular sleep, and the level of sedation is dose-dependent. Lower plasma concentrations result in lighter sedation. The experience of our participants could also be related to the fact that stimulation ought to happen at maximum plasma concentration of dexmedetomidine (22).
Correct dosages for different children
The anaesthetic nurses had found positive experiences with doses of 2 µg/kg to the youngest children, aged one to four years. They reported that in the beginning they faced some challenges in finding an appropriate dosage for children over the age of four. When the effect was unsatisfactory, they repeated the initial dosage. Some of them also reported that for children weighing more than 12 kg, they adjusted the dosage upwards to 2.5 µg/kg. The time of onset was reported as lasting from 20 minutes to one hour.
These findings are largely consistent with the findings in the study conducted by Yuen and collaborators (24). The latter study indicates a time of onset varying from 25–30 minutes after a dosage of 1 µg/kg. The findings in our study corroborate those of Yuen and collaborators (25), which describe how children from five to eight years had a significantly poorer effect of a dose of 1 µg/kg when compared to children aged 1–4 years. They conclude that a dosage of 2 µg/kg results in a satisfactory sedation of children (25).
Our findings show, however, that such premedication for the oldest children more often must be assessed individually. A recent study by Tug and collaborators (26) indicates that dexmedetomidine in doses of 4 µg/kg could be administered to sedate children from one to 10 years for MRI scanning without detection of respiratory depression or circulatory disturbances that required treatment.
The findings in our study corroborate previous research on the challenges involved in finding the correct dosage of intranasal dexmedetomidine (25, 26). These studies nevertheless describe dexmedetomidine as a safe drug, even when used at high dosage.
Collaboration is essential
The anaesthetic nurses believed that the long onset time of the drug might cause problems for patient flow, especially at the start of work in the morning. They said that for the children to benefit from dexmedetomidine as premedication, the drug needed to take effect before they started working with the children. The anaesthetic nurses described interdisciplinary collaboration in the department as crucial to solving logistical challenges.
This practice illustrates Bjørk and Solhaug’s (27) description of how innovations are introduced. This is not a solo task, it depends on collaboration among all members of the ward community to succeed. Some participants emphasised how collaboration across professional groups gave rise to shared ‘ownership’ of the project. This sentiment promoted a proactive approach and a positive commitment in the units, and a focus on the best interests of the child.
Many participants described how efficiency improved when dexmedetomidine worked as intended and planning succeeded. Our findings elucidate the high level of motivation among the staff to succeed with the use of dexmedetomidine, despite the challenges involved. It became clear that the anaesthetic nurses have felt the need for a suitable alternative drug for premedication of children.
The anaesthetic nurses described how the successful introduction of dexmedetomidine depended on collaboration with the department’s anaesthesiologist. The anaesthesiologist’s knowledge about the drug and belief in its suitability as a paediatric premedication meant that the introduction process enjoyed strong support.
Flynn and collaborators (12) emphasise the importance of good teamwork between the anaesthesiologist and the anaesthetic nurse as a factor that ensures provision of appropriate health-promoting measures to patients and improves patient safety. Good teamwork is characterised by mutual trust and respect for the expertise of the other (12). The anaesthetic nurses in our study highlighted exactly this kind of collaboration with the anaesthesiologist.
Bjørk and Solhaug (27) describe that in order to succeed, it is extremely important for professional development projects to be endorsed by the department management or other people in authority. Findings in our study clearly show the complexity involved in introducing new medical routines. Concerns for efficient and safe running of the unit must be prioritised, although the most important factor is the way in which the children and their parents perceive the treatment programme. Developing such projects requires information flow and collaboration between the professional groups in the institution (27).
The drug was not anxiety-inducing
The participants perceived the induction of anaesthesia with the sleeping children as safer than with children who are awake and resist. According to Scully (7), children’s anxiety with regard to the unknown increases at this stage, and the induction of anaesthesia may thus be a negative experience. The risk of anaesthesia-related complications is generally higher at the induction stage. Crying and resistance may increase this risk even further (7, 28). The findings in our study indicate that dexmedetomidine as paediatric premedication has favourable effects at the induction stage of anaesthesia and causes a minimum of complications when the necessary precautions are taken.
Peri- and post-operative experiences
The participants described the perioperative stage as calm and stable. Previous studies indicate that dexmedetomidine may reduce the need for anaesthetic drugs perioperatively and prolong the effect of opioids, which may entail a reduced need for analgesics postoperatively. The studies also indicate that dexmedetomidine as premedication protects better against postoperative agitation than midazolam (3, 8, 29).
The anaesthetic nurses described recoveries that were characterised by less crying, agitation and pain. The participants clearly emphasised that the specialist nurses who monitored the children postoperatively preferred dexmedetomidine over midazolam as premedication. These findings corroborate studies that describe the sedative and analgesic properties of dexmedetomidine (1, 8, 21).
The half-life of two to three hours explains why the children may benefit from the drug at the early postoperative stage after short interventions (3, 8, 21). Our findings corroborate that the premedication has a beneficial effect on the entire course of the anaesthesia process (8).
Methodological considerations
By using a phenomenological-hermeneutic approach we have gained a deeper understanding of the participants’ experiences. These experiences have in turn helped provide an important basis for interpretation and new knowledge about this topic. The intra-sample variation in age, gender, department culture, professional experience and experience with the use of dexmedetomidine produced largely identical data, which is evidence of a high degree of consistency in the data material, which in turn is corroborated by recent research.
We also believe that such intra-sample variation has reduced the risk of biased elucidations of the research question. In our opinion, the study’s sample and informational strength are satisfactory in light of the objective, composition of the sample, theoretical basis, data quality and analysis (30).
None of the authors had any affiliation with the hospitals from which the participants were recruited. This may have helped provide distance and an ‘outsider’s’ view of the data. In addition, the first author, who also conducted the interviews, had prior experience with dexmedetomidine through a pilot project undertaken at her own workplace involving children who were to undergo an MRI scan while under anaesthesia.
The preconceptions that the first author brought with her into the study may have had an effect on our choice of research questions, how the interviews and analyses were conducted and the findings that we present. The authors’ long-standing experience of this research field as professional anaesthetic nurses may have helped provide unique insights that enabled the identification of patterns and complexities that would have been less obvious to outsiders (18).
To ensure credibility we included the voices of the participants, described the analytical steps and made the abstraction process transparent. The first and third authors have primarily undertaken the data analysis, first individually and then jointly to achieve consensus on the categories chosen and the design of the topics, and to prevent biased interpretations of the data material (17).
Our findings may be transferable to other departments where anaesthesia personnel are working with children, if the department culture and context are taken into consideration. Data collection methods and analyses may also be transferable. The findings must nevertheless be interpreted in light of their basis in the experiences of a small sample of anaesthetic nurses with a permanent workplace.
Implications for practice
The findings show that the anaesthetic nurses administer a drug which is well suited as premedication, provided that the given precautions are taken. Dexmedetomidine has helped provide better treatment options for children and is evidently safe in use. The sleep-inducing properties of this drug can be made use of to undertake simple and less painful procedures on children. The findings indicate that such systematic change processes should be introduced by way of internal pilot projects.
Implications for further research
We suggest that further research ought to focus on ways in which the potentiating effects of dexmedetomidine with regard to analgesics and anaesthetic drugs could be exploited in multimodal treatment and be included in general anaesthesia for an individually adapted treatment programme.
We also recommend that further research be undertaken on how these sleep-inducing properties can be exploited to enable various procedures and examinations. Finding the correct dosage of dexmedetomidine has proven to be a challenge, and we recommend further research related to age, weight and dosage.
Conclusion
The study provides new knowledge from the anaesthetic nurse’s perspective on the properties and suitability of dexmedetomidine as paediatric premedication. The anaesthetic nurses’ experiences are generally of a positive nature, and dexmedetomidine has a beneficial effect on the pre-, peri- and post-operative anaesthesia process in children.
Successful use of dexmedetomidine requires that special and individual precautions be taken at all stages of the anaesthesia process. We nevertheless regard the disadvantages as minor when compared to all the advantages that we have shown.
References
1. Sun Y, Lu Y, Huang Y, Jiang H. Is dexmedetomidine superior to midazolam as a premedication in children? A meta-analysis of randomized controlled trials. Pediatric Anesthesia. 2014;24(8):863–74. DOI: 10.1111/pan.12391.
2. Felleskatalogen. Dexdor. Available at: https://www.felleskatalogen.no/medisin/dexdor-orion-573728(downloaded 24.03.2017).
3. Pasin L, Febres D, Testa V, Frati E, Borghi G, Landoni G, et al. Dexmedetomidine vs midazolam as preanesthetic medication in children: a meta-analysis of randomized controlled trials. Pediatric Anesthesia. 2015;25(5):468–76. DOI: 10.1111/pan.12587.
4. Ghai B, Jain K, Saxema AK, Bhatia N, Sodhi KS. Comparison of oral midazolam with intranasal dexmedetomidine premedication for children undergoing CT imaging: a randomized, double-blind, and controlled study. Pediatric Anesthesia. 2017;27(1):37–44. DOI: 10.1111/pan.13010.
5. Neville DNW, Hayes KR, Ivan Y, McDowell ER, Pitetti RD. Double-blind randomized controlled trial of intranasal dexmedetomidine versus intranasal midazolam as anxiolysis prior to pediatric laceration repair in the emergency department. Academic Emergency Medicine. 2016;3(8):910–7.
6. Mountain BW, Smithson L, Cramolini M, Wyatt TH, Newmann M. Dexmedetomidine as a pediatric anesthetic premedication to reduce anxiety and to deter emergence delirium. AANA Journal. 2011;79(3):219–24.
7. Scully SM. Parental presence during pediatric anesthesia induction. AORN Journal. 2007;96(1):26–33. DOI: 10.1016/j.aorn.2011.07.020.
8. Peng K, Wu S, Ji F, Li J. Premedication with dexmedetomidine in pediatric patients: a systematic review and meta-analysis. Clinics. 2014;69(11):777–86. DOI: 10.6061/clinics/2014(11)12.
9. Wolf AR, Rosenbaum A, Kain ZN, Larsson P, Lönnqvist P-A. The place of premedication in pediatric practice. Pediatric Anesthesia. 2009;19(9):817–28. DOI: 10.1111/j.1460-9592.2009.03114.x.
10. Holm-Knutsen R. Præoperativ vurdering og forberedelse av barn og forældre. In: Henneberg SW, Hansen TG, eds. Børneanæstesi. 2. ed. Copenhagen: FADLs Forlag; 2015. p. 97–105.
11. Ghali AM, Mahfouz AK, Al-Bahrani M. Preanesthetic medication in children: A comparison of intranasal dexmedetomidine versus oral midazolam. Saudi J Anaesth. 2011;5(4):387–91. DOI: 10.4103/1658-354X.87268.
12. Flynn FM, Sandaker K, Ballangrud R. Aiming for excellence – A simulation-based study on adapting and testing an instrument for developing non-technical skills in Norwegian student nurse anaesthetists. Nurse Education in Practice. 2017;22:37–46.
13. Jeon Y, Lahtinen P, Meretoja R, Leino-Kilpi H. Anaesthesia nursing education in Nordic countries: Literature review. Nurse Education Today. 2015;35(5):680–8.
14. Lov 2. juli 1999 nr. 64 om helsepersonell m.v. (helsepersonelloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-64?q=helsepersonelloven(downloaded 24.03.2017).
15. Lov 2. juli 1999 nr. 63 om pasient- og brukerrettighetsloven (pasientrettighetsloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-63?q=pasientrettighetsloven(downloaded 24.03.2017).
16. Nortvedt MW, Jamtvedt G, Graverholt B, Nordheim LV, Reinar LM. Jobb kunnskapsbasert. En arbeidsbok. 2. ed. Oslo: Akribe; 2014.
17. Polit DF, Beck CT. Nursing research. Generating and assessing evidence for nursing practice. 9. ed. Philadelphia: Wolters Kluwer, Lippingcott, William & Wilkins; 2012.
18. Thagaard T. Systematikk og innlevelse. En innføring i kvalitativ metode. 4. ed. Bergen: Fagbokforlaget; 2015.
19. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–12. DOI: 10.1016/j.nedt.2003.10.001.
20. Sheta SA, Al-Sarheed MA, Abdelhalim AA. Intranasal dexmedetomidine vs midazolam for premedication in children undergoing complete dental rehabilitation: a double-blinded randomized controlled trial. Pediatric Anesthesia. 2014;24(2):181–9. DOI: 10.1111/pan.12287.
21. Li A, Yuen VMY, Goulay-Dufay S, Kwok PCL. Pharmacokinetics and pharmacodynamics of dexmedetomidine. Drug Development and Industrial Pharmacy. 2016;42(12):1917–27.
22. Iirola T, Vilo S, Manner T, Aantaa R, Lahtinen M, Scheinin KT, et al. Bioavailability of dexmedetomidine after intranasal administration. European Journal of Clinical Pharmacology. 2011;67(8):825–31. DOI: 10.1007/s00228-011-1002-y.
23. Yuen VMY. Dexmedetomidine: perioperative applications in children. Pediatric Anesthesia. 2010;20(3):256–64. DOI: 10.1111/j.1460-9592.2009.03207.x.
24. Yuen VM, Hui TW, Irwin MG, Yao TJ, Wong GL, Yuen MK. Optimal timing for the administration of intranasal dexmedetomidine for premedication in children. Anaesthesia. 2010;65(9):922–9. DOI: 10.1111/j.1365-2044.2010.06453.x.
25. Yuen VM, Hui TW, Irwin MG, Yao TJ, Chan L, Wong GL, et al. A randomised comparison of two intranasal dexmedetomidine doses for premedication in children. Anaesthesia. 2012;67(11):1210–6. DOI: 10.1111/j.1365-2044.2012.07309.x.
26. Tug A, Hanci A, Turk HS, Aybey F, Isil CT, Sayin P, et al. Comparison of two different intranasal doses of dexmedetomidine in children for magnetic resonance imaging sedation. Pediatric Drugs. 2015;17(6):479–85. DOI: 10.1007/s40272-015-0145-1.
27. Bjørk IT, Solhaug M. Fagutvikling og forskning i klinisk sykepleie. En ressursbok. 1. ed. Oslo: Akribe; 2015.
28. Berg T, Hagen O. Forebygging og behandling av anestesirelaterte komplikasjoner. In: Hovind IL, ed. Anestesisykepleie. 2. ed. Oslo: Akribe; 2011. p. 280–306.
29. Yao Y, Qian B, Lin Y, Wu W, Ye H, Chen Y. Intranasal dexmedetomidine reduces minimal alveolar concentration of sevoflurane for laryngeal mask airway insertion and emergence delirium in children: a prospective, randomized, double-blind, placebo-controlled trial. Pediatric Anesthesia. 2015;25(5):492–8. DOI: 10.1111/pan.12574.
30. Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: Guided by information power. Qualitative Health Research. 2016;26(13):1753–60. DOI: 10.1177/1049732315617444.

Comments