No place like home? Home-based chemotherapy for adolescent and young adult sarcoma patients – a qualitative study
Summary
Background: Adolescents and young adults with cancer have special challenges and needs that health personnel should be aware of in order to help them live as normally as possible while undergoing cancer treatment. Home-based chemotherapy is a service that can result in less time spent in hospital. Previous research shows, among other things, that the treatment is safe and feasible. There is, however, a need for more research on patients’ perceptions of home-based chemotherapy.
Objective: The objective is to examine how adolescent and young adult sarcoma patients perceive home-based chemotherapy.
Method: We conducted a qualitative study consisting of semi-structured individual interviews with nine patients aged from 16 to 30. All of them had carried out at least one round of chemotherapy at home. The transcribed data was analysed in accordance with Braun and Clarke’s reflexive thematic analysis model.
Results: Home-based chemotherapy affected the informants psychologically, helped to maintain their social ties and enhanced their physical well-being. The psychological effects were described as both positive and negative, where key findings included increased stress, the need to have an overview and a sense of freedom. The maintenance of social ties concerns relationships with family and friends and opportunities to socialise, such as being able to attend school. Enhanced physical well-being includes sleeping better, increased appetite, less nausea and an increased level of activity when treatment is administered at home.
Conclusion: The informants explained that home-based chemotherapy has both advantages and disadvantages. They experienced different psychological effects, but the maintenance of social ties and enhanced physical well-being appeared to be positive for all informants. The study suggests that home-based chemotherapy is advantageous for adolescents and young adults as it enables them to lead a more normal life while undergoing cancer treatment, but this method of treatment can be optimised.
Cite the article
Bøgseth H, Sandven I. No place like home? Home-based chemotherapy for adolescent and young adult sarcoma patients – a qualitative study. Sykepleien Forskning. 2025;20(98652):e-98652. DOI: 10.4220/Sykepleienf.2025.98652en
Introduction
The number of adolescents and young adults (AYAs) who are diagnosed with cancer annually on an international basis is approximately 1.2 million, which corresponds to roughly 5% of all cancer cases worldwide (1). While the number is growing each year, it is nevertheless an understudied patient group (2–5).
Internationally, the term AYA includes people aged from 15 to 39 (2, 6). In Norway, different definitions apply when the term AYA is used. Patient organisations use the definition to describe patients up to 35 years of age (7). In our data, AYA is defined as patients aged between 16 and 30.
Sarcoma represents roughly one percent of all cancer cases and is an umbrella term for cancer in bones and connective tissues (8). The disease is more frequent among children and adolescents, and it makes up approximately 10–15% of all cancer cases that emerge in childhood and adolescence. In Norway, about 550 new sarcoma cases are diagnosed annually. Of these, 20 to 25 belong to the subgroup of osteosarcoma, which most frequently affects AYAs (9).
The treatment patients receive is lengthy and consists of chemotherapy and surgery (10, 11), which entail spending a great deal of time in hospital (4). AYAs are a vulnerable group. Many of these young people can be lacking in the life experience and coping skills necessary to be able to manage a serious illness, and they require extra attention from the health service (12).
To minimise the effect that cancer and its treatment have on AYAs, it is recommended that health personnel support them so that they can live as normally as possible (13, 14–17). The provision of home-based chemotherapy (HBC) could form a part of this, as well as helping patients to feel they have greater control over the situation (14).
HBC is a service that has been offered to AYA sarcoma patients since 2020. The service allows patients to receive part of their treatment at home (Appendix 1 and Appendix 2, in Norwegian only). Chemotherapy or intravenous fluid is administered to the patient via an infusion pump placed in a special backpack (Appendix 3, in Norwegian only).
Before being offered HBC, all patients must have completed at least one round of treatment in hospital. Patients attend hospital on a daily basis, or every other day, for blood tests and other health checks, as well as to record observations made at home.
International research on HBC has shown promising results, with fewer chemotherapy-related side effects such as nausea, reduced appetite and fatigue (5, 17). In addition, the treatment method may be considered both feasible and safe as there have been no reported serious complications (2, 3, 16, 17). Studies also show that patients were satisfied and that they were able to maintain their daily routines and social lives to a greater degree (4, 18, 19).
Previous research on HBC on a global basis has either focused on children or adults (2–5, 16–19). Studies also indicate that AYAs have special needs, and that research should focus on this patient group as well (6, 12, 20, 21).
There are calls for more research on this patient group’s perceptions of HBC, both the benefits and the challenges associated with treatment (14, 21). We used Antonovsky’s theory as a theoretical basis for our work. As health personnel, we should focus on promoting the patient’s ability to cope and their health (22).
Objective of the study
The objective of our study was to increase knowledge concerning the perceptions of AYA sarcoma patients aged between 16 to 30 regarding HBC. The research question was as follows: ‘What are the perceptions of adolescent and young adult sarcoma patients regarding home-based chemotherapy?’
Method
Design
We used a qualitative research design and semi-structured individual interviews to obtain detailed descriptions from the informants (23).
Sample and recruitment
We carried out strategic selection to increase knowledge about a specific phenomenon and illuminate the research question in the best way possible (23, 24).
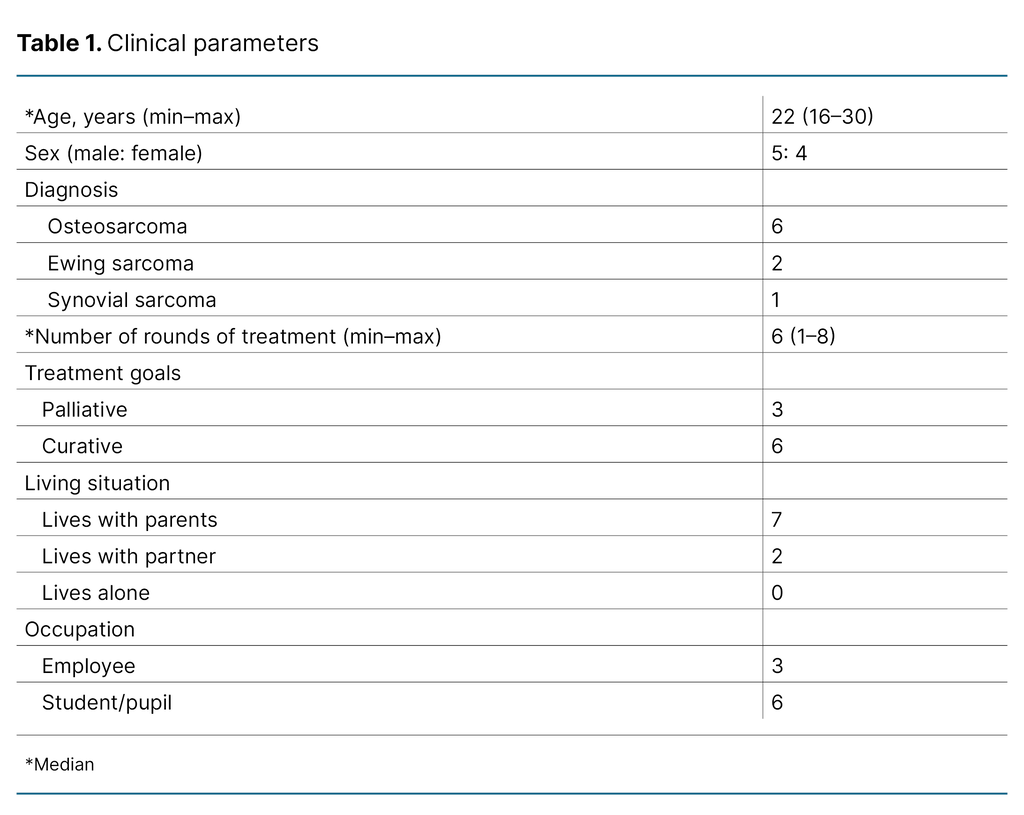
The inclusion criteria were that informants must have been diagnosed with sarcoma, have completed at least one round of treatment at home and be aged between 16 and 30. The patients were recruited at the outpatient clinic and ward of a university hospital in Norway. All of the patients who met the inclusion criteria were given an information letter with a request to participate. Eleven patients were asked, of whom two declined. Nine patients were subsequently included (Table 1).
Implementation and data collection
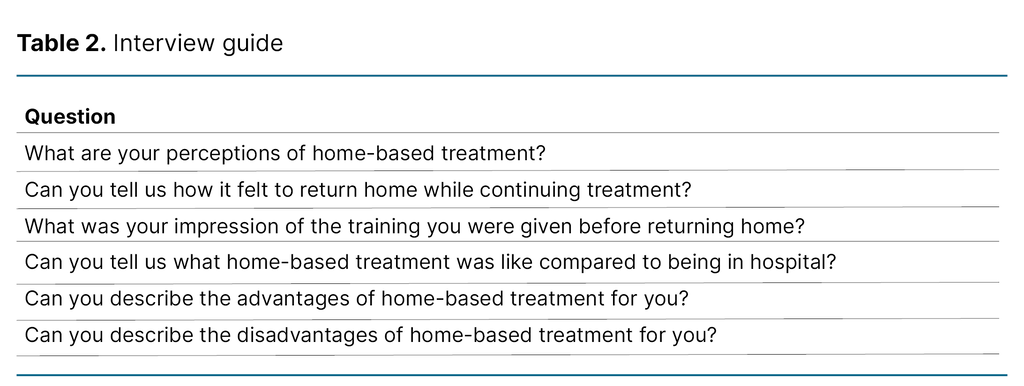
Data were collected in the period from June to October 2023. We used an interview guide (Table 2) with open questions based on previous studies that had been conducted on the same topic, to ensure that our perceptions did not influence the questions and answers provided by the study (4). The interviews were carried out by the last author, who does not have a clinical position and was therefore unacquainted with the informants (26). We recorded the interviews on audiotape and transcribed them.
Analysis
The data were analysed in six steps according to Braun and Clarke’s reflexive thematic analysis model (25). The model’s flexibility was important because the informants differed, both in terms of age and level of maturity. Furthermore, they had different perceptions and experiences of treatment.
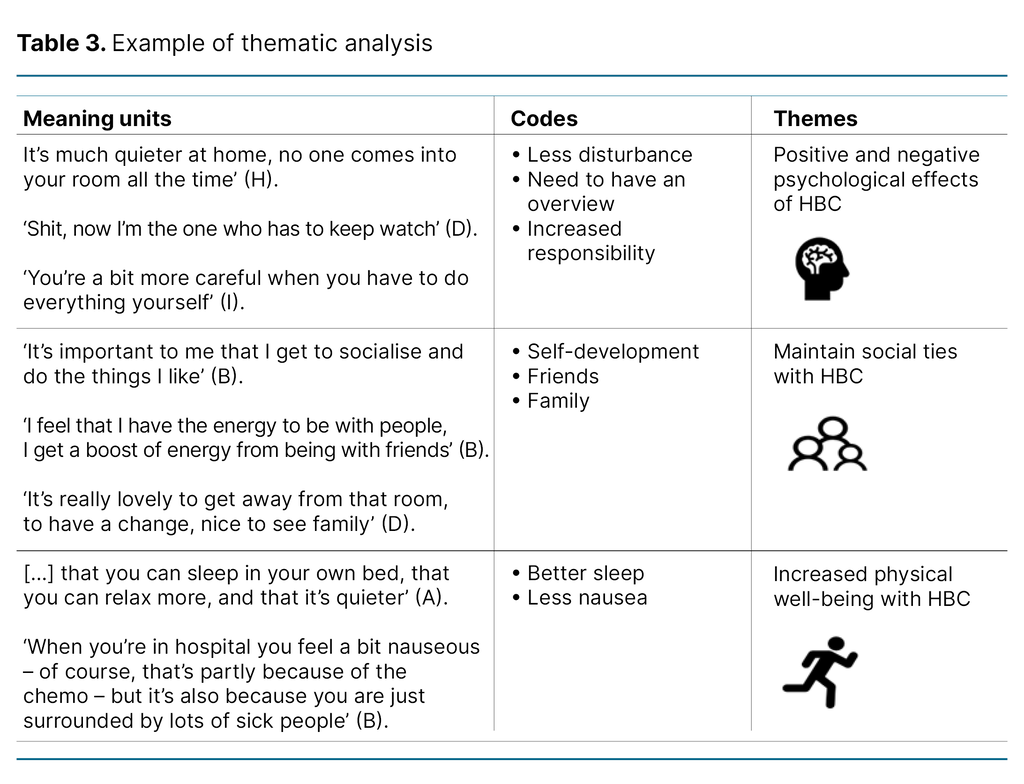
Both authors carried out the analysis, individually and in collaboration, to gain familiarity with the data. Meaning units were extracted from the transcribed data and converted into codes, which then resulted in themes (Table 3).
During the analysis process, informants were assigned a letter of the alphabet to prevent them from being identified. The letter is used with the quotations so that no one can be recognised by diagnosis or age in this small patient group. We took an open-minded approach to interpreting the text, and the terms that are used are those of the informants themselves. In the analysis process, we attempted to put aside our own experiences as far as possible. Nevertheless, we are aware that preconceptions are of significance in our interpretation and analysis of the text (24, 26), particularly in discussions in which we actively used our experiences to compare findings with other research and clinical practice.
Ethical considerations
The study is part of a larger research project on HBC that is being carried out at a university hospital in Norway. The main project was submitted to the Regional Committee for Medical and Health Research Ethics (REK), reference number 498856, which concluded that the project was not subject to notification as the objective was not to obtain new knowledge on disease and health. The project was approved by the data protection officer at the university hospital, case number 22/22156.
The informants received an information letter and consent form which had to be signed before the interview took place. All of the informants were informed that they could withdraw at any time without providing a reason.
The data were stored on a research server at the university hospital to ensure confidentiality and anonymity. The audio recordings were deleted after analysis of the data was complete.
Results
The informants had different perceptions of HBC. They experienced various psychological effects, and this emerged as the most central finding. It was positive for all informants to maintain social ties and enhance their physical well-being, and their descriptions of the themes corresponded. The themes influenced each other to a large extent.
Positive and negative psychological effects of HBC
The informants experienced different mental stresses. For some, carrying out treatment at home was positive, while others felt it was challenging to have responsibility for their own treatment.
The sense of freedom reduced the mental stress of undergoing cancer treatment: ‘It’s important for my mental health that I can be at home as much as possible, because then, in a way, I feel better in myself and the others at home perhaps feel a little better’ (E). Many of the informants found that HBC made it possible to relax in a different way than in hospital. The informants pointed out that they experienced less disturbance at home.
Several of them felt confident about the method of treatment and described the feeling of being ‘more normal’ (F) with HBC. They saw the importance of being able to spend more time at home. There was less feeling of being sick compared to being in hospital. Other advantages of HBC were as follows: ‘The good thing about the backpack is that I can hide a little bit, people don’t automatically see that you’re getting chemotherapy’ (D).
Other informants were affected negatively when they were given HBC. They perceived that home was different and therefore felt heightened stress: ‘You take hospital home with you’ (I). They pointed out that the sound from the infusion pump was a negative factor because it was unfamiliar at home.
Some felt a greater sense of responsibility and said that it was frightening not to have health personnel close by. The sense of security was not the same at home as in hospital: ‘It was a bit more demanding than I expected. When you’re at home, you have to think and do everything yourself. When you’re in hospital, the nurses do it’ (I).
Some also felt that their relationship to the health personnel changed because of HBC. They perceived that they did not have the same sense of belonging at the hospital and did not feel prioritised: ‘I felt like I was just left sitting and waiting, and that I was at the back of the queue’ (C). Others experienced the opposite, that health personnel had allocated time for them when they were at the hospital and that they had better contact.
The distance to the hospital may have influenced perceptions of HBC. Those who had a long way to travel found HBC more stressful and the journey tired them. At the same time, they pointed out that there was less disturbance at home and that they saw the value of having the flexibility to be able to choose to go home: ‘It’s a really good service and it’s nice to have the opportunity, if you want to do it’ (C).
Some of the informants who had undergone many rounds of treatment at home found that they gradually became less worried as they became more confident in using the equipment. They explained that what was frightening the first few times, such as the fear of something going wrong, gradually became less frightening. Others found that the stress persisted, and they alternated between being at home and getting treatment at the hospital throughout the course of treatment.
Maintenance of social ties with HBC
The informants believed that it was easier to carry out HBC because it helped to maintain social ties.
All of the informants said that it was essential to maintain social ties while they underwent cancer treatment. They pointed out the benefits of being together with their family and participating in daily activities just like they did when they were well, for example, lying on the sofa watching a film. ‘You have a bit more social contact, it makes it all a bit more positive. It’s easier to get an energy boost than if you’re just in hospital, both physically and mentally, actually’ (E).
Some of them felt lonely when they were in hospital and could not be together with others. For this reason, they considered HBC as valuable in a prolonged course of treatment. The special backpack gave them a sense of freedom, and several experienced an energy boost by socialising with friends and family.
Adolescents of school age and students pointed out that it was important to be able to participate in class to maintain social ties and for learning: ‘I think it’s fun to be able to go to school and learn things, it’s fun to be able to do things, and to be able to do things you have to learn things’ (B). Being able to participate at school some of the time made them feel a part of the classroom community and that they had a natural meeting point with friends.
Enhanced physical well-being with HBC
The informants pointed out that their physical well-being was enhanced when they were given HBC. They experienced fewer side effects of treatment at home compared with hospital treatment.
All of the informants slept better when they were able to sleep in their own beds: ‘Nothing is better than sleeping in your own bed’ (C). Several of them explained further that it was important for them to be able to relax, and that they got an energy boost by being at home. In addition, the informants said that they had a better appetite and less nausea. They ate more when they were able to eat the food they liked, together with others.
When they compared being hooked up to a traditional drip stand, the informants said that it was better to have a backpack and be able to move around freely: ‘It gives me the freedom to do whatever I want’ (G). All of the informants described having freedom of movement as positive, so that they could participate in everyday activities when they were at home.
Discussion
The study’s informants experienced different psychological effects as a result of HBC and possibly more negative effects than previous publications have reported. In previous studies, most of the patients were content with being able to spend time at home. The same applied to the parents of children who received HBC (2–5, 16–19). At the same time, our informants felt that it was positive to be able to maintain social ties and physical well-being with HBC.
Adolescents and young adults receiving cancer treatment at home – the advantages and disadvantages
The informants perceived that the psychological effects varied. Some of them found HBC stressful and regarded it as a heavy responsibility. Measuring diuresis, using the infusion pump and administering medication were stressful. However, several informants said that this improved when they felt more confident and had been through this at home a number of times. Previous research also shows that confidence increases with experience (5, 17).
Only a minority in our sample did not want HBC due to this responsibility, but some chose to undergo some rounds of treatment in hospital to avoid the responsibility and stress. Others found, however, that they were able to relax and were subject to less disturbance when they were at home and therefore chose HBC as often as they could. Some of the informants felt that the pump made a lot of noise and that the sound was more prominent at home.
Another important aspect to take into consideration is how the informants perceived bringing the hospital home with them. For some, this meant that their home, which was their sanctuary, became filled with illness and treatment, which felt invasive and therefore created a barrier to accepting HBC. This finding corresponds with previous research, which shows that patients had similar challenges with HBC (18).
Other research conflicted with this, finding that it was easier for patients to adapt to the situation if they received treatment in their own home (4). Our findings and previous research show both similarities and contradictory results. These aspects should be subject to focus in further work on HBC.
The psychological effects informants experienced may create barriers to HBC, so measures such as more training and patient involvement prior to discharge should be a priority. The same findings emerged in previous studies (4, 12, 16, 17, 19).
Our experience indicates that a good relationship with health personnel can be an important resource for AYAs undergoing cancer treatment. This relationship would probably be affected if they were not at the hospital. In our data there are different perceptions of this.
Some informants found that time had been allocated for them when they were at the hospital, while one informant felt that patients receiving HBC came last in the queue. This informant said that there was no time allocated for HBC patients and that follow-up at the hospital was random. It is important to be aware of this when improving HBC, so that everyone who receives this treatment feels that they are being looked after.
The distance between the informants’ homes and the hospital emerges as a relevant factor in our study. Those with farthest to travel had the greatest level of stress. This finding is important for determining a limit on how far away the patient can be from a clinic when they are undergoing chemotherapy at home. In other words, the research indicates that it is necessary to set a maximum distance to enable HBC to be carried out safely and effectively. Even though some of the informants lived close to the hospital, they still felt that the journey was a strain.
There are many advantages with HBC for AYAs. If health personnel can remove the barriers to this treatment, the provision of HBC could benefit more patients in the future.
The social needs of AYA sarcoma patients are looked after
The informants in the study lived with their parents or partners. They received good support from their families and considered social contact with them to be important. Several of them explained that socialising gave them an energy boost. Social ties and choices while undergoing treatment are important for coping with cancer treatment (6, 12, 19–21, 27).
The findings in our study suggest that HBC contributes to less social isolation for AYAs while undergoing treatment. Our findings and previous research indicate that HBC is positive because it allows AYAs to be at home more often and participate in normal daily life with family and friends, as well as the social circle of their peers.
For AYAs, a meaningful daily life is essential, and the maintenance of normality was a key reason to choose HBC. Normality seems to revolve around two different aspects: living with family and friends and avoiding being different. Both aspects are easier with HBC. Previous research shows that it is crucial to socialise with friends, attend school and maintain family contact (3, 6, 12, 17, 19–21). By supporting AYA cancer patients to live as normally as possible, the effects of cancer treatment on their psychosocial well-being can be reduced (14).
The suicide rate among AYAs undergoing cancer treatment is higher than in the general population. One reason for this may be the greater mental stress caused by treatment. Sarcoma patients are included among those at greatest risk of suicide (28). HBC can help to reduce the mental stress by reducing the extent to which patients feel alienated.
Managing chemotherapy-related side effects
The informants had a better appetite with HBC than when they were in hospital. Adequate food intake increases the likelihood of the patient being able to carry out cancer treatment and can therefore affect survival. Undernutrition is a known negative prognosis factor in cancer treatment that can result in dosage reductions, more side effects and complications (29).
The informants reported having less nausea, which can reduce the level of feeling sick and have a positive effect on appetite. Nausea is described as one of the most unpleasant side effects associated with chemotherapy (30). It would be beneficial if AYAs could avoid this during their course of treatment. Being able to cope with side effects can have a positive effect on life quality, nutrition and the total burden of the illness and treatment.
Increased activity and freedom of movement were also positive for the informants. This is another advantage of HBC, as patients that stayed active had fewer side effects during treatment. The benefits of physical activity while undergoing cancer treatment may include increased energy, a better self-image, limited muscle loss and reduced nausea, stress and anxiety.
Another important finding that has been little referred to in previous research was that informants believed that there was a big difference between sleeping in their own bed and in a hospital bed. They slept much better at home. The stress that many patients experience can affect their sleep, and the fact that this can be ameliorated by HBC was one of the advantages perceived by the study’s informants.
The informants felt that they were more content and had a better quality of life, which emerges as an important finding although the data is limited. Previous studies on HBC have also attempted to address well-being and quality of life, but have failed to find clear correlations (2, 12, 16).
Strengths and weaknesses of the study
The informants had different treatment goals and there was a wide spread of ages, which enriched the data. The basis for comparison was unique because all of the informants had received some treatment at the hospital.
Our preconceptions can be seen as both a strength and a weakness of the work. Familiarity with the field of research makes it possible to develop questions for the interview guide that are relevant to the research question. At the same time, proximity to the field could affect analysis of the data. For example, something that is obvious to us might not be expressed as a finding. We were conscious of this during the analysis and used meaning units to ensure that what the informants told us is what is presented in the findings. This approach was also discussed at the master’s seminar and with the supervisor to increase the study’s reliability.
The fact that we only recruited informants from one hospital is a weakness (24). We could not include a broader selection because no other hospital in Norway offers HBC to AYA sarcoma patients.
Conclusion
The study’s findings indicate that HBC has advantages and disadvantages for AYAs. The psychological effects differed. Some experienced increased stress and responsibility, while others had a sense of freedom and were better off mentally when they spent more time at home. One important finding was that multiple rounds of treatment at home increased the informants’ confidence.
For those who received HBC, it was vital to maintain their social ties. They were able to be with their friends and family, which gave them an energy boost. Enhanced physical well-being, which entailed better sleep, less nausea and a better appetite, was an advantage experienced by all informants.
The study suggests that HBC is advantageous, but that the method of treatment itself can be further developed and improved. There is a need for more research in the field to optimise the method of treatment, so that it can benefit more patients.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge

Comments