Critically ill medical patients in the emergency department before and during the pandemic – an observational study
Summary
Background: Potentially critically ill medical patients in the emergency department need a rapid assessment and treatment to improve patient outcomes. We have little knowledge of this patient group in Norway. Nor do we know whether the COVID-19 pandemic affected patient management and patient outcomes.
Objective: We wanted to investigate the characteristics, management and outcomes before and during the pandemic in medical patients in the emergency department (ED) who were potentially in a critical condition, and identify factors associated with admission to intensive care.
Method: This observational study included all ‘medical team’ patients in 2018 and 2021. The data were obtained from the medical team’s quality register at Oslo University Hospital, Ullevål.
Results: A total of 671 patients from 2018 and 601 from 2021 were included. In 2018, the mean age was 58 years, 37 per cent were women and the majority had low somatic comorbidity. The prevalence of patients with a history of substance use and psychiatric history was 23 and 16 per cent respectively. A total of 58 per cent were admitted to the intensive care unit (ICU), and the 30-day mortality was 14 per cent. The most frequent discharge diagnosis was acute poisoning (28 per cent). The percentage of women increased from 37 to 44 per cent from 2018 to 2021. In the same period, the percentage with a psychiatric history and limitation of medical treatment (LOMT) increased. The median length of stay in the ED increased from 95 to 115 minutes, and 30-day mortality increased from 14 to 18 per cent. In addition, fewer non-isolated patients were transferred to the ICU (from 58 to 50 per cent), and length of stay (LOS) there was shorter (from 30 to 20 hours). The most frequent discharge diagnosis in 2021 was a neurological condition (22 per cent). Younger age was only associated with admission to the ICU in 2018, while psychiatric history was only significant in 2021. In both years, a history of substance use, a higher NEWS2 score, critical care medications and critical care interventions were associated with admission to intensive care.
Conclusion: The patient group was relatively young with little comorbidity in both years. Over half were admitted to the ICU. Acute poisoning was the most frequent diagnosis. Patient characteristics changed somewhat during the pandemic. Treatment measures in the ED were relatively unchanged, indicating that the service provision before and during the pandemic was the same.
Cite the article
Jervell S, Vangdal H, Engebretsen S. Critically ill medical patients in the emergency department before and during the pandemic – an observational study. Sykepleien Forskning. 2025;20(98544):e-98544. DOI: 10.4220/Sykepleienf.2025.98544en
Introduction
Critically ill medical patients are a heterogeneous group that may present with complex symptoms and complaints. There is no universal definition of critical illness (1). It is often uncertain whether the patients are critically ill or what their diagnosis is prior to the initial assessment. Patients may have organ failure, and often need stabilising or life-saving treatment (1).
Common complaints are reduced consciousness, neurological symptoms, intoxication, dyspnoea and shock (2, 3). Mortality varies from 16 to 36 per cent (2, 3). Rapid identification and treatment in the ED can improve patient outcomes (4).
The COVID-19 pandemic resulted in a new group of potentially critically ill patients. The virus primarily affected the respiratory system but also other organs (5). Patients in isolation, full ICUs and limited knowledge about the properties of the virus created challenges in the health service (6). A number of institutions introduced criteria for deciding which patients should be treated in hospitals and ICUs (7).
Fewer patients sought help for myocardial infarction and other acute illnesses (8). Delays in elective assessment and treatment may have resulted in increased treatment needs and mortality in the long term, also in patients without COVID-19 (8). There are few studies on patients without COVID-19 and how they were affected by the pandemic (8).
The Norwegian healthcare authorities specify that all emergency departments (EDs) must have routines for assessing patients with critical and time-sensitive conditions (4). There is considerable variation in how critically ill medical patients are dealt with in EDs. Internationally, there are calls for guidelines on identification and assessment of this patient group (2, 9), as is the case for patients with cardiac arrest, stroke and trauma (4, 10). Before such guidelines can be developed, more knowledge is needed about the patient group in general also during a pandemic.
Objective of the study
The objective of the study, therefore, was to examine and compare patient characteristics, management and patient outcomes in potentially critically ill medical patients in the ED before and during the pandemic. We also wanted to examine what factors were associated with admission to the ICU. Moreover, we wished to examine and compare these factors in patients without suspected COVID-19 during the pandemic.
Method
Design, study population and setting
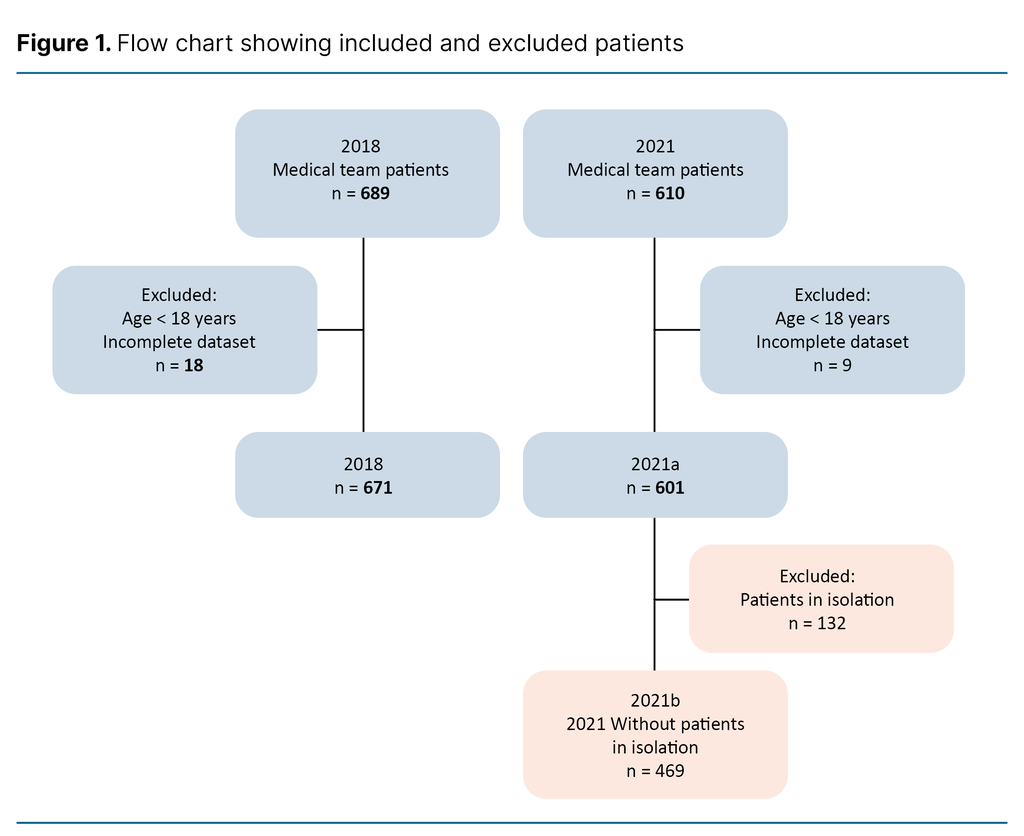
We performed a retrospective observational study from the calendar years 2018 and 2021. We excluded patients with missing data and those under the age of 18 (n = 27, Figure 1).
Oslo University Hospital, Ullevål (OUS-U) is a local hospital for parts of Oslo’s population as well as functioning as a regional hospital for trauma patients and patients with myocardial infarction, among others.
About 15 per cent are potentially critically ill or injured, and are met by different multidisciplinary teams. The remaining patients are triaged using the Manchester Triage Scale (11) and are met by a doctor and a registered nurse (RN). In 2018, the ED received 29 549 patients, and 45 per cent of these had internal medicine conditions. The number of patients remained at the same level in 2021.
Potentially critically ill medical patients are met by a multidisciplinary team referred to as a ‘medical team’, with a total of nine members. Pre-defined criteria are used to identify potentially critically ill patients. The criteria are based on patient presentation or vital signs. In addition, healthcare personnel can activate the team if they are concerned about the patient ( Appendix 1 – in Norwegian).
The patients are seen in resuscitation rooms with advanced equipment. Healthcare personnel carry out a systematic assessment in order to quickly identify and treat critical conditions. Patients with cardiac arrest, myocardial infarction, sepsis or stroke are met by other teams unless they require assessment and stabilisation by a medical team.
Quality register
The data are obtained from an internal quality register for medical teams at OUS-U that contains retrospective data from the medical records of all patients met by a medical team in the ED. The register was established in 2016, and contains data from 2015 onward. The data are registered manually by a nurse who is familiar the patient group who had received training in registration.
Data from 2019 and 2020 were not registered due to the reallocation of resources and the subsequent halt in registration during the pandemic. After the pandemic, the register owner decided to start registering data from 2021. Consequently, we used data from 2018 and 2021, with the former regarded as a normal year and the latter as one of the pandemic years.
Pandemic
In 2021, the pandemic experienced its third and fourth waves, and mass vaccinations had started (12). Social restrictions varied throughout the year. Patients in the ED with suspected COVID-19 were isolated pending test results. The analysis time for a rapid PCR test was approximately one hour in 2021.
Staffing in the ED was increased but not in the medical team. Dedicated resuscitation rooms were equipped for patients in isolation, where team members worked in full personal protective equipment (PPE). One of the team members was in the airlock lobby and communicated with the rest of the team by telephone, delivering equipment and medications as required.
Data collection
The variables used were limited to the data available in the quality register. The available variables describing patient characteristics, including patient condition, were sex, age, presenting complaint, history of substance use and psychiatric history, the Charlson Comorbidity Index (CCI) original version (13), and the National Early Warning Score 2 (NEWS2) (14).
Presenting complaints were divided into seven categories (Appendix 2 – in Norwegian). The CCI is a scoring system for classifying comorbidity whereby age and various diagnoses such as cardiovascular disease, diabetes and dementia are given point scores. A high score can predict the mortality risk (13). The CCI was categorised as 0 points (p), 1–2 p, 3–4 p and > 4 p (3).
The NEWS2 score is based on the first measurements in the ED and scores respiratory rate, peripheral oxygen saturation, systolic blood pressure, pulse rate, level of consciousness, oxygen treatment and temperature. The score varies from 0‒20 points, and the higher the score, the greater the deviation from normal values (14).
The score is used to detect deterioration in a patient’s condition at an early stage so that treatment can be initiated rapidly (14). Age was a continuous variable while the other variables were categorical. NEWS2 was used as both a continuous and categorical variable (3, 14).
Variables for interventions were intubation, other airway interventions, non-invasive ventilation (NIV), arterial catheter, arterial blood gas, central venous catheter (CVC), other interventions (external pacing, cardioversion and/or chest drain), X-ray of the upper part of the chest (thorax), CT of the head (caput), and focused echocardiography.
Furthermore, we used variables for acute medications administered: antibiotics, antiarrhythmics, anaesthetics, sedatives, vasopressors and blood products (Appendix 3 – in Norwegian) as well as the following LOMT: ‘do not resuscitate’, ‘do not intubate’ and ’not for ICU’. In 2021, we also used data on isolation and confirmed COVID-19. All variables were categorical.
For patient outcomes, we used the variables: length of stay (LOS) in the emergency department, in the ICU and in hospital, destination after the ED, main discharge diagnosis and mortality. The destination after the ED is categorised as ICU, ward or other (other hospital/institution or dwelling), or death in the ED. Discharge diagnoses are categorised in the same way as the presenting complaint and are based on ICD 10 codes on discharge (Appendix 2 – in Norwegian).
Mortality has two variables: 24 hours and 30 days after arrival in the ED. Variables for LOS are continuous, the remainder are categorical.
In multivariate analysis, the variables intubation, other airway intervention, NIV, arterial catheter, CVC and blood products were combined into one dichotomous variable called ‘critical care interventions’. Variables for antiarrhythmic drugs, anaesthetics, sedatives and vasopressors were combined under ‘critical care medications’ (3). ‘Do not resuscitate’ and ‘do not intubate’ were combined into the variable ‘LOMT’.
Statistical analysis
We analysed the data using SPSS version 29.0. Continuous variables are presented as mean and confidence interval (CI) or median and interquartile range (IQR), categorical variables in numbers and percentages.
For comparison, we used the t-test or the Mann-Whitney test for continuous variables and the chi-square test or Fisher’s exact test for categorical variables. The results are given as p-values where p < 0.05 is regarded as statistically significant. Data from 2018 were compared with the 2021 data, both the total number (2021a) and a sub-group that excluded those in isolation (2021b). Missing data are reported as missing in the tables.
To identify factors associated with admission to intensive care, we carried out a forward Wald multivariate logistic regression analysis for both years. Clinically relevant variables and variables with a low p-value in bivariate analyses were included, i.e. sex, age, CCI, history of substance use, psychiatric history, NEWS2, LOMT, critical care interventions and critical care medications.
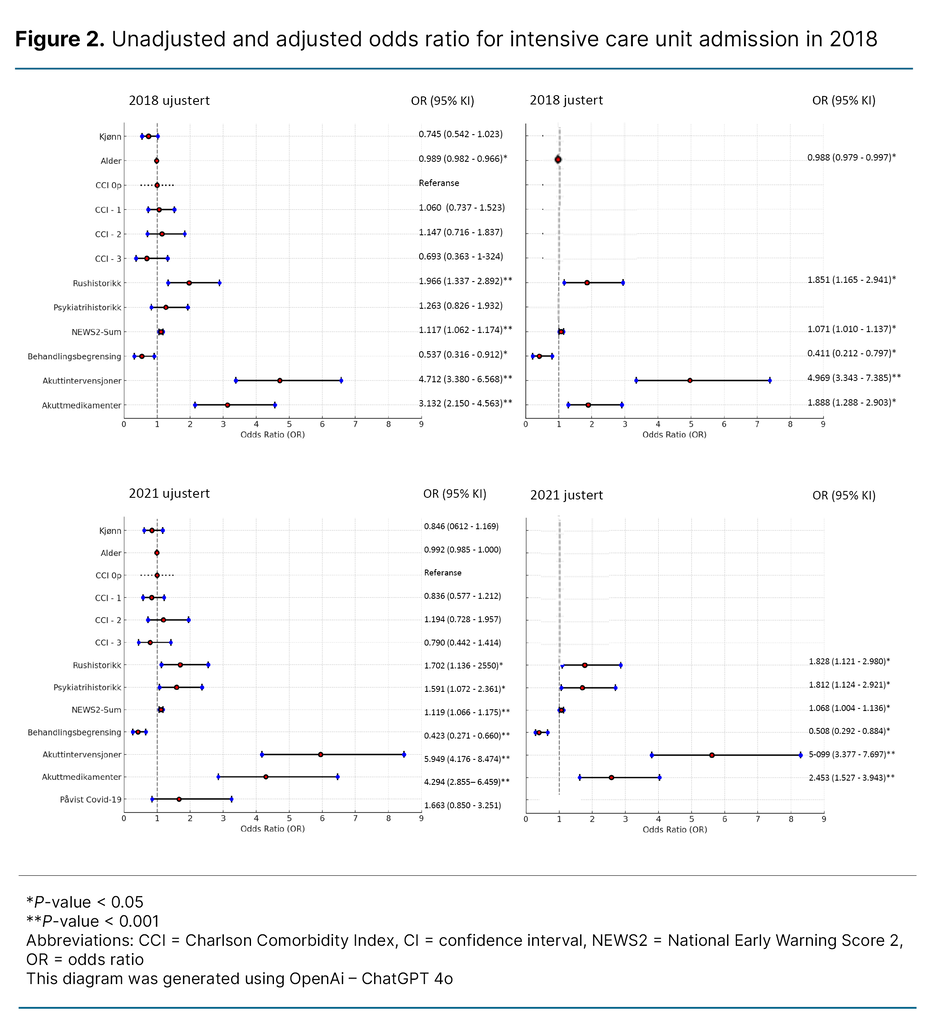
In 2021, we also included confirmed COVID-19. The results are presented in a forest plot, as both unadjusted and adjusted odds ratio (OR) with CI and p-values, providing an overview of how the factors affect the outcome alone and together. For adjusted OR, we show only statistically significant variables.
Ethics
The study was approved by the data protection officer at Oslo University Hospital with no requirement for informed consent (reference number 23/02877). The Regional Committee for Medical and Health Research Ethics assessed the study as not subject to approval (reference number 585260).
Results
A total of 1272 patients were included: 671 from 2018 and 601 from 2021. Of the 601 patients in 2021 (2021a), 469 were not put in isolation. These constitute 2021b (Figure 1).
Patient characteristics
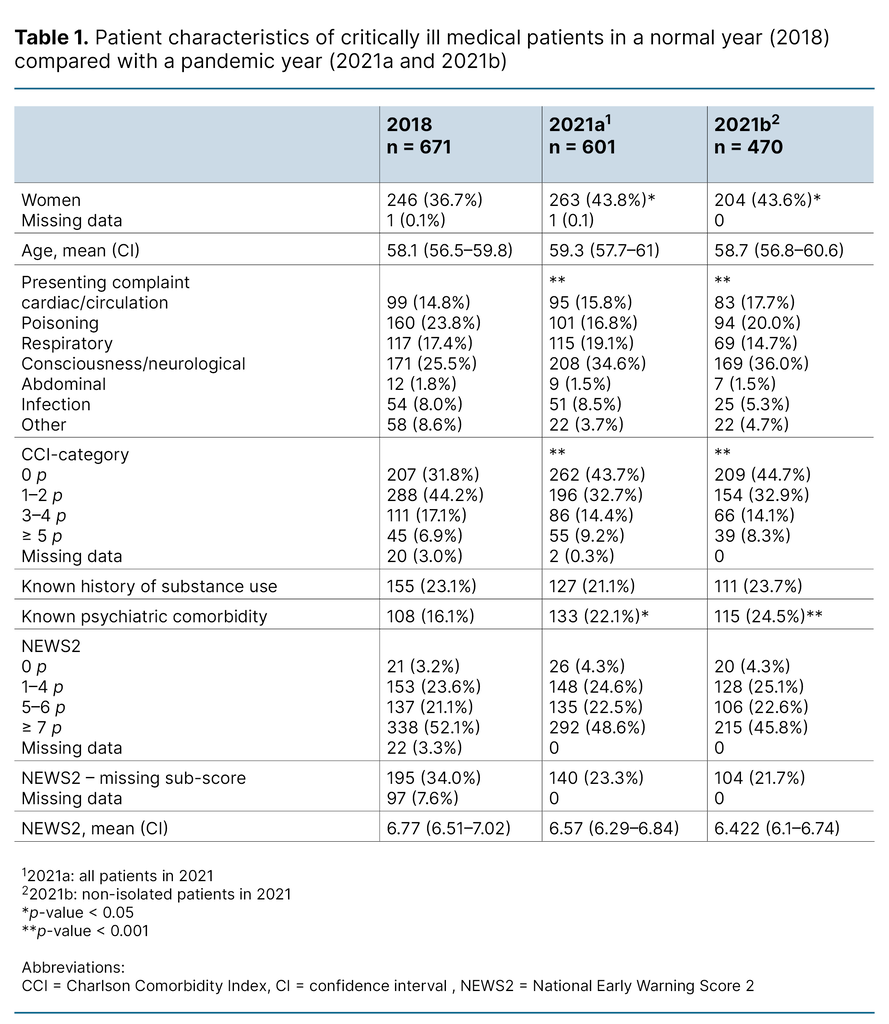
Table 1 shows patient characteristics in 2018 and 2021. In both years, there were more men than women who received care from the medical team. The patients were relatively young, with low somatic comorbidity measured using the CCI. The most common presenting complaint in both years were poisoning and problems related to consciousness or neurology. The proportion with infection as a reason for admission was low.
NEWS2 was relatively high in both years and approximately three-quarters scored five or higher. In 2021, the percentage of women was higher, and the patients had better somatic health, but more had a psychiatric history. There was also an increase in consciousness or neurological conditions, and a decline in acute poisoning as reason for admission.
Management
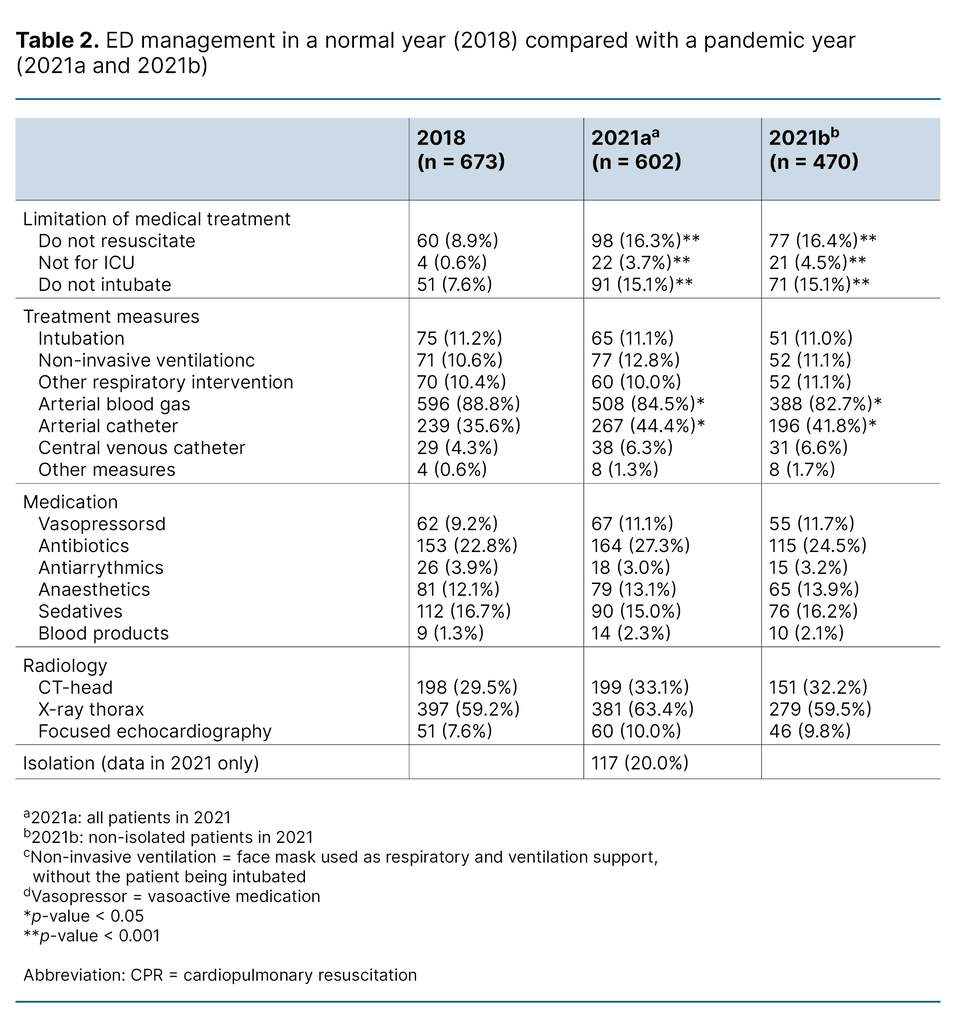
Table 2 shows interventions in the ED for both years. Intubation, NIV and vasopressors were stable at 10–12 per cent both years. There were few significant differences in interventions in the period 2018 to 2021.
The use of antibiotics rose somewhat in 2021 but not significantly. In contrast, there was a significant increase in the percentage of patients with LOMT, from less than 9 per cent to around 16 per cent. There was also a reduction in the number of arterial blood gases and an increase in insertion of arterial lines.
Patient outcomes
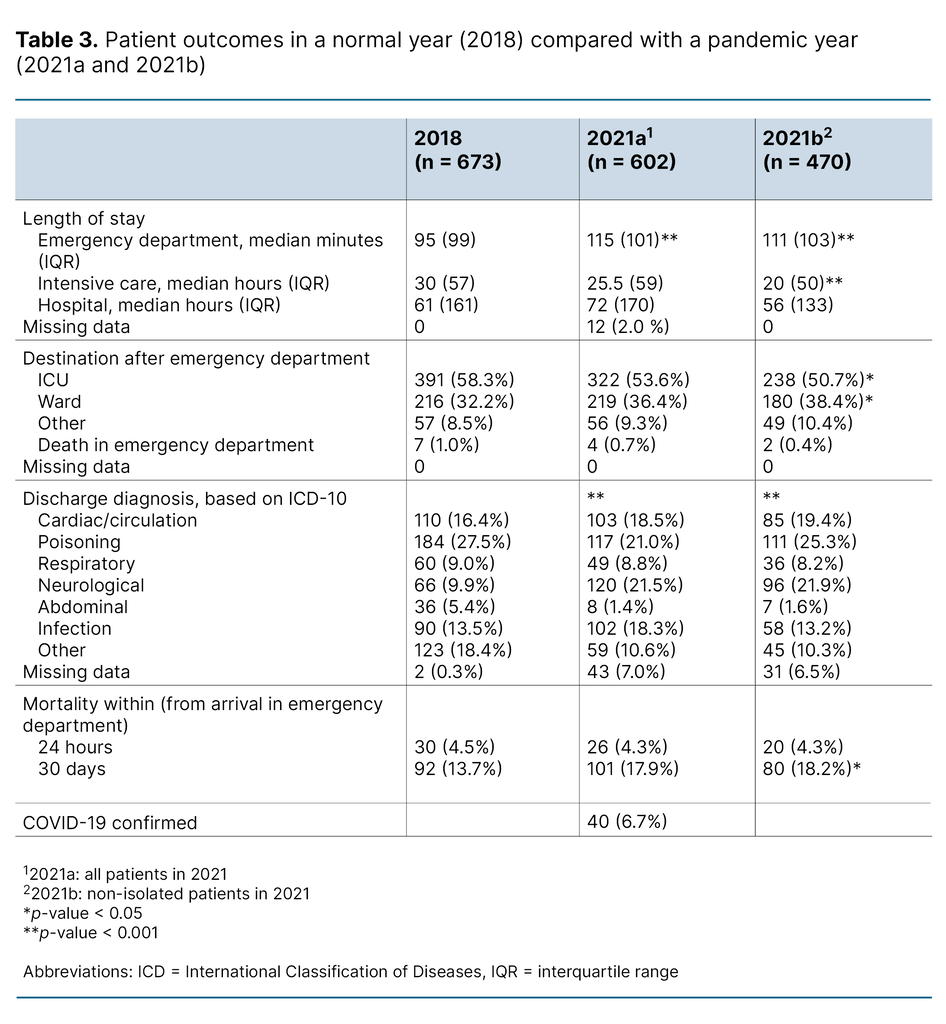
Table 3 shows patient outcomes for patients met by the medical team. LOS in the ED was under two hours in both years, and over half the patients were transferred to the ICU. The median LOS there was under 24 hours.
In 2021, LOS in the ED increased. There was a decline in poisonings and an increase in neurological and respiratory diagnoses. Infection diagnoses increased for 2021a, but not for 2021b. Moreover, 30-day mortality increased significantly in 2021. In the group of non-isolated patients (2021b), there was also a significant fall in the number of intensive care admissions and a reduction in LOS in the ICU.
Factors associated with admission to the ICU
In both years, a history of substance use, higher NEWS2 score, critical care medication and critical care interventions were associated with ICU admission, while LOMT in the form of ‘do not resuscitate’ and ‘do not intubate’ orders had a negative association (Figure 2). Younger age was associated with admission to intensive care in 2018 only, while psychiatric history was associated with ICU admission only in 2021.
Discussion
The majority of patients assessed by the medical team were men, and the patients were young with little comorbidity. Most had NEWS2 ≥ 5, and over half were admitted to the ICU. Acute poisoning was a common discharge diagnosis. In 2021, the percentage of women increased, and patients had less somatic but more psychiatric comorbidity. A number had LOMT, and LOS in the ED and 30-day mortality increased.
Fewer of the patients who were not in isolation were admitted to the ICU, and LOS there was shorter. Factors associated with ICU admission were relatively similar in both years, but in 2021, psychiatric history was an additional factor, and age was no longer associated with such admissions.
Patient characteristics
In our study, the majority of critically ill patients were men. This is in line with other studies of the same patient group (2, 3). Men are also more likely to be admitted to the ICU (15). This, coupled with the tendency for women to present with more vague symptoms (15) may have contributed to a higher number of men being treated by the medical team in our ED.
Additionally, the high number of patients with acute poisoning may have contributed to the greater number of men in our sample, as they have a higher rate of substance use and potentially more overdoses (16, 17). During the pandemic, we saw an increase in the number of women seen by the medical team. This increase was also seen in Norwegian ICUs (18). Reduced access to substances during the pandemic, and consequently fewer men with acute poisoning, may have been a contributing factor (19).
The mean age was 58–59 years, which is lower than in similar international studies, where the mean age was 65–70 years (2). These studies had fewer patients with acute poisoning (2), which may explain the difference, as patients presenting with poisoning are often young (16, 20).
In our study, young age may also entail that the patients were relatively healthy somatically before the hospitalisation in question. However, there was a considerable increase in patients with a psychiatric history in 2021. There was an increase in mental disorders during the pandemic, both in Norway and internationally (21). We can therefore assume that this is reflected in an increase in psychiatric history in patients admitted to the ED during the pandemic.
Despite low somatic comorbidity, the majority of patients in both years showed signs of organ failure, represented by high NEWS2 on admission. A high NEWS2 score is associated with ICU admission and increased mortality (22). The large proportion of patients requiring ICU admission and displaying signs of organ failure highlights the need for a rapid initial team assessment and management of this patient group.
Management
Interventions in the ED were relatively similar immediately prior to and during the pandemic. Measures such as intubation and vasopressors were used less frequently than in international studies (2). This may be because critical illness is defined differently and because our population had less organ failure than in these studies. International studies call for guidelines on the treatment of critically ill medical patients (2), and this is supported by our findings.
During the pandemic, far more patients had LOMT, despite a lower CCI. The number was also higher than in an earlier study at our hospital (3). This finding represented the biggest difference between the two years. Many countries had limited ICU capacity during the pandemic (6, 7), and this may have necessitated LOMT decisions in the ED.
There has been greater focus on the clarification of level of medical treatment for patients on admission to hospital (23). Studies, as well as our own experiences, indicate that such decisions are a key task for those treating critically ill patients (24).
Isolation can create problems with communication, equipment and logistics in patient care (5). Nevertheless, interventions were relatively similar prior to and during the pandemic. This may be because local guidelines were quickly developed, and simulation training was carried out when the pandemic started. Moreover, the routine for managing patients in isolation was fairly well established in 2021. Had the data been from 2020, there might have been greater differences in treatment measures.
Patient outcomes
LOS in both the ED and ICU was shorter than in international studies (2). The former may be explained by the fact that boarding time at our hospital were shorter than what is normally the case internationally (25, 26).
A median LOS in the ICU of 25–30 hours is considerably shorter than in German studies, where the LOS was 144–192 hours (2). The large number of patients with acute poisoning, lower somatic morbidity and age as well as less organ failure may have contributed to this finding (19). Germany also has better access to ICU beds than Norway (27), which may mean that the patients are not transferred to a ward as quickly.
The access to ICU beds may also explain why more patients in the German studies were transferred to the ICU. It is probably also significant that in the German studies, a higher percentage needed organ support. The patients in the German studies appeared to be sicker than in our study, and this is also reflected in the higher mortality (2). These differences underline the need for guidelines to identify and manage this patient group.
Several patient outcomes changed from 2018 to 2021. LOS in the ED increased, both for those in isolation and those who were not isolated, while other studies find the increase in LOS mostly for patients in isolation (28). Greater LOS for both groups may be due to longer waiting times for a place in the ICU, as one of the hospital’s ICUs only admitted COVID-19 patients.
Internationally, an extended LOS in the ED is associated with poorer patient outcomes (25), and we found an increase in 30-day mortality in 2021. The level was the same as in 2015 and 2016 (3), indicating that mortality in 2018 was lower than normal. The higher number of patients with LOMT during the pandemic may also have contributed to increased mortality.
There was a fairly large increase in neurological discharge diagnoses in 2021. COVID-19 can result in neurological symptoms and outcomes, both while infected and post-infection (29), but we do not know whether this can explain the whole increase. It is likely that the establishment of a stroke unit at the hospital in 2019 meant that more patients were seen by a medical team, but we have not investigated this further.
We also found fewer ICU admissions and shorter lengths of stay at the ICU for non-isolated patients during the pandemic. The drop in ICU admissions is in line with international figures, but shorter intensive care stays are not described in international studies (30). In this group, there were more patients with acute poisoning and fewer with infections, and this may also have impacted on LOS.
Factors associated with admission to intensive care
In both years, critical care interventions and critical care medications were associated with admission to the ICU. These findings have also been described previously (3), and it is natural that such management requires admission to intensive care to ensure monitoring and the continuation of treatment.
Earlier studies show that higher NEWS2 scores increase the probability of both admission to intensive care and mortality (22, 31). This is also reflected in our study, in which an increased NEWS2 score was associated with admission to intensive care. A higher score indicates greater organ failure and thus a need for a kind of monitoring and treatment that most wards do not offer. The negative association of LOMT with intensive care admission also corresponds with previous studies (3, 32).
A history of substance use was associated with admission to intensive care in both years, a finding that was not made in an earlier study at the same hospital even though the prevalence of this was relatively similar (3). Other studies have not examined history of substance use for this patient group (2). A possible explanation is that several of the patients with acute poisoning had a history of substance use, and many needed intensive care monitoring because of reduced consciousness and compromised airways. Several studies also found that approximately 20 per cent of ICU admissions are associated with substance use (33).
In 2021, psychiatric history was associated with admission to intensive care, which was not the case in 2018 or in the earlier study from the same hospital (3). There were significantly more patients with a psychiatric history in 2021 than in 2018, which may have contributed to this finding. Other studies of this patient group in EDs do not include data on psychiatric history (2), but it has been demonstrated that up to 30 per cent of intensive care patients have such a history (34).
Advanced age was negatively associated with ICU admission in 2018 only, not in 2021, despite several other studies also finding such a negative association (3, 32). A systematic literature review found that intensive care capacity may contribute to older patients not being admitted to the ICU (32). This is not reflected in our results despite the pandemic. It is possible that the oldest patients were not as critically ill as in 2018, and increased awareness of the benefits of intensive care for older patients may also have played a role (35).
Positive COVID-19 test results were not associated with admission to intensive care in 2021. This may be because there were relatively few patients with COVID-19, and that the third and fourth waves did not result in the same degree of critical illness as earlier in the pandemic (29). In other words, the patient’s diagnosis was less significant for the further treatment level than the patient’s condition.
Strengths and limitations of the study
Observational studies can have unknown biases that may affect the results or lead to difficulties determining causal effects. Another limitation of the study is that it was conducted at just one hospital. The sample varied somewhat compared with similar studies in other settings (2). This makes it difficult to generalise the findings even though many may be transferable. The results in our study can be compared with an earlier study at the same hospital. This strengthens the findings (3).
There is a risk of missing information in retrospective data. It has been difficult to minimise this risk because the data stem from a quality register. Consequently, we have only been able to carry out a critical review of the dataset. Conversely, the use of register data allowed us to include many patients in the study, and to identify associations and discuss possible explanations.
The study contains data from the pandemic year 2021, when the third and fourth waves of infection hit (12). Mass vaccination was started, and reports suggest that virus mutations carried a lower risk of a severe clinical course (12, 29). These aspects might have led to different results if we had used data from 2020.
Conclusion
This study provides greater insight into a patient group we know little about: potentially critical ill medical patients. Over half were admitted to the ICU, and about one quarter had acute poisoning. Organ failure and organ support treatment were the most significant factors for intensive care admission.
In 2021, the percentage of women increased, and more patients had a psychiatric history. More patients had limitation of treatment, and LOS in the ED increased. There was a reduction in ICU admissions and LOS for non-isolated patients.
There were few changes in management, indicating that the ED was able to offer the same service provision before and during the pandemic. The differences between the findings in our study and international studies confirms the need for guidelines to ensure consistent identification and management of this patient group. Until such guidelines are in place, the knowledge generated by this study can be used to plan care and treatment, and serve as a basis for competence development in healthcare personnel who manage these patients.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge
Corrected reference numbers under the headline «Ethics» (15.10.2025).
Original text:
The study was approved by the data protection officer at Oslo University Hospital with no requirement for informed consent (reference number 25502975). The Regional Committee for Medical and Health Research Ethics assessed the study as not subject to approval (reference number 469517).
Revised text:
The study was approved by the data protection officer at Oslo University Hospital with no requirement for informed consent (reference number 23/02877). The Regional Committee for Medical and Health Research Ethics assessed the study as not subject to approval (reference number 585260).


Comments