Sleep quality of nurses in the specialist health service – a cross-sectional study
Summary
Background: Sleep is necessary for human functioning. The quality of sleep determines the extent to which a person’s need for sleep is met. Nurses may be a vulnerable group because shift work can lead to sleep problems, and consequently poorer health, quality of patient care and job satisfaction.
Objective: The aim of the study was to assess the sleep quality of nurses on hospital wards in the specialist health service. We also wanted to investigate the relationships between sleep quality and various demographic and work-related factors.
Method: We conducted a cross-sectional study of nurses working on hospital wards in the specialist health service in Norway from December 2020 to February 2021. Sleep quality was measured using the Pittsburgh Sleep Quality Index (PSQI). Poor sleep quality was defined as PSQI > 5. We analysed the relationships between sleep quality and demographic and work-related factors using Pearson’s chi-square test, Fisher’s exact test, the Mann-Whitney U test and linear regression analysis.
Results: A total of 259 nurses consented to participate. Of these, 235 (90.7%) worked on wards in the specialist health service and were therefore included in the study. The mean global PSQI score was 9.38 (standard deviation 3.42). Poor sleep quality was observed in 86.4% of participants. Short rest periods between evening and day shifts and greater involvement in drawing up their own shift rota were associated with poorer sleep quality. Satisfaction with the shift rota was associated with better sleep quality.
Conclusion: This study shows that nurses on hospital wards in the specialist health service have poor sleep quality. The sleep quality is poorer than for similar groups in other studies. For nurses on hospital wards in the specialist health service, it seems that rest time, involvement in shift planning and shift rota satisfaction are associated with sleep quality, and should therefore be examined in future studies.
Cite the article
Jacobsen V, Børøsund E, Henni S, Bergsaker A, Opheim R. Sleep quality of nurses in the specialist health service – a cross-sectional study. Sykepleien Forskning. 2024;19(96926):e-96926. DOI: 10.4220/Sykepleienf.2024.96926en
Introduction
Sleep is an important element of human functioning and can affect us both physically and mentally (1, 2). How much sleep we need varies from person to person. Nevertheless, the recommended sleep duration remains relatively constant at 7–9 hours per night from the age of 20 (2). Sleep quality is partly influenced by the circadian rhythm, which is regulated by a nucleus in the brain called the suprachiasmatic nucleus (2).
Shift work disrupts the circadian rhythm, and both sleep duration and sleep quality are negatively affected. This can contribute to a range of issues, such as heart disease, diabetes and mental disorders (2). Sleep quality is a complex concept and includes factors such as sleep quantity, sleep latency, sleep disturbances, depth of sleep and habitual sleep efficiency (3).
The Working Environment Act (4, section 10-8[1]) stipulates a minimum rest time of 11 hours between two work periods. This is in line with the EU’s Working Time Directive, which is applicable in Norway (5, Chapter 2, Article 3). However, the Working Environment Act allows for the rest period to be reduced, by agreement, to eight hours (4, section 10-8[3]). The most common short rest period is between evening and day shifts (6). Short rest periods and night shifts can be associated with poorer performance and sleep quality. Improving sleep quality may reduce the risk of errors (7, 8).
Shift work has a more negative impact on sleep duration and sleep quality among older shift workers than younger ones, particularly with short rest periods between evening and day shifts, as well as with night work (9-11). Research shows that the likelihood of experiencing good or poor sleep does not depend on the number of years of work experience (9, 10). However, there is evidence that the longer intensive care nurses have been working shifts, the higher their tolerance for sleep problems (11).
A systematic literature review of shift work and nurses’ health showed that shift work exacerbates sleep problems (12). Nurses report a high prevalence of sleep problems, which can lead to poorer health, quality of patient care and job satisfaction (6, 11, 13, 14). In a Norwegian study of intensive care nurses, 70% of participants reported poor sleep quality (11). Significant differences in sleep quality have also been observed among nurses across hospital departments (8).
There is little research on the relationship between sleep quality and job satisfaction, but some findings suggest that better sleep quality leads to higher job satisfaction, and vice versa (15, 16). A Swedish study found that short rest periods negatively affect nurses’ sleep quality and shift rota satisfaction (17).
However, no studies appear to have explored the relationship between sleep quality and nurses’ shift rota satisfaction. A systematic literature review showed that employees who are able to influence their working day are more satisfied and are less likely to leave the labour force (18).
Objective of the study
The objective of this study was therefore to
- assess the sleep quality of nurses on hospital wards in the specialist health service, and
- investigate the relationships between sleep quality and various demographic and work-related factors.
Method
Design
In this descriptive cross-sectional study, data were collected via a questionnaire. This data collection method is well-suited for examining the relationships between factors at a specific point in time (19). The questionnaire included demographic and work-related questions, as well as a measurement of sleep quality.
Recruitment
The questionnaire was distributed via the ‘Sykepleieforskning’ (Nursing research) Facebook group, which had around 10 000 followers. We collected the data by distributing the survey twice: first on 28 December 2020, and then on 24 January 2021, before closing the questionnaire for responses on 4 February 2021.
Posts in the Facebook group were shared a total of 42 times. Responses to the questionnaire were collected via Nettskjema.no, the University of Oslo’s digital platform (20).
Measuring sleep quality
In this study, we used the Pittsburgh Sleep Quality Index (PSQI) as the primary outcome measurement for sleep quality (3). The PSQI consists of dichotomous questions and multiple-choice questions across seven standardised components: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication and daytime dysfunction (3, 21).
Each component is scored from 0 to 3, and the global score is measured on a scale from 0 to 21. A global score for the components of > 5 indicates poor sleep quality, meaning the participant has significant challenges in at least two components or moderate challenges in three or more components (3).
The PSQI was developed to provide a reliable, valid and standardised measure of sleep quality. Globally, the PSQI has been validated for many populations, including healthy adolescents and adults, as well as those with somatic and mental disorders (22). The PSQI is frequently used in research to measure nurses’ sleep quality (7–11, 23) and has been translated to Norwegian and validated among nursing home staff and students (21).
The original version of the PSQI has a Cronbach’s alpha of 0.83, and the Norwegian validated version has a Cronbach’s alpha of 0.77 (3, 21). In our study, the Cronbach’s alpha is 0.71, which indicates acceptable internal consistency in the study (19, 24).
Data collection, coding of variables and data analysis
The questionnaire included two screening questions for inclusion in the study: participants had to indicate that they consented to participate in the study and that they were working as nurses on a specialist health service ward. The sociodemographic and work-related variables in the study were as follows: sex, age, workplace (type of ward and regional health authority), work experience, percentage of full-time position, rest time between evening and day shifts, number of evening and night shifts per month and working time arrangements, involvement in shift planning and shift rota satisfaction.
All work-related variables were multiple-choice questions with a free text field option. The workplace was coded as medical, surgical and other types of wards, along with the specific regional health authority the nurses worked in. The percentage of full-time position was coded as full time (100%) or part time (< 100%).
Working time arrangements were denoted as single-shift rota, two-shift rota or three-shift rota and were further coded into two groups: all those working a three-shift rota (day, evening and night) and those working only one or two of the shift types. Involvement in shift planning and shift rota satisfaction were coded as dichotomous variables with the categories ‘small/very small/zero degree’ and ‘large/very large degree’ of involvement or satisfaction. The PSQI was coded according to the tool’s instruction manual (3).
The results are presented as descriptive statistics: categorical data as absolute numbers and percentages, and continuous data as median with range or mean with standard deviation (SD), depending on normal distribution.
Differences between categorical variables were analysed using Pearson’s chi-square test, with one exception where we used Fisher’s exact test because the expected value was five or less in the matrix. Group differences between good and poor sleep quality in continuous variables were analysed using Mann-Whitney’s U test, as the variables were not normally distributed.
A linear regression model was used to examine possible associations between sleep quality and demographic and work-related factors. Participants for whom there was not a complete dataset were excluded from this analysis (3.4%, 8/235).
All variables were included in a univariable analysis. All variables that showed an association with sleep quality in the univariable analysis (p < 0.200), in addition to age, were included in a multivariable model. The variables were included simultaneously, thus controlling for the effects of other variables in the model (19).
The association is expressed as unstandardised beta coefficients, and the uncertainty of the estimates is given as a 95% confidence interval. The significance level is set at p < 0.05. The statistical analysis was performed using IBM SPSS Statistics version 28 for Mac (25).
Research ethics considerations
Participants were informed about the objective of the study and the time each participant would be required to spend on it. We told them that participation was voluntary and that the study was anonymous, and explained how the data would be used. Since we did not collect any direct or indirect personal information, Sikt – the Norwegian Agency for Shared Services in Education and Research found that the study was not subject to reporting (reference number 834431).
Results
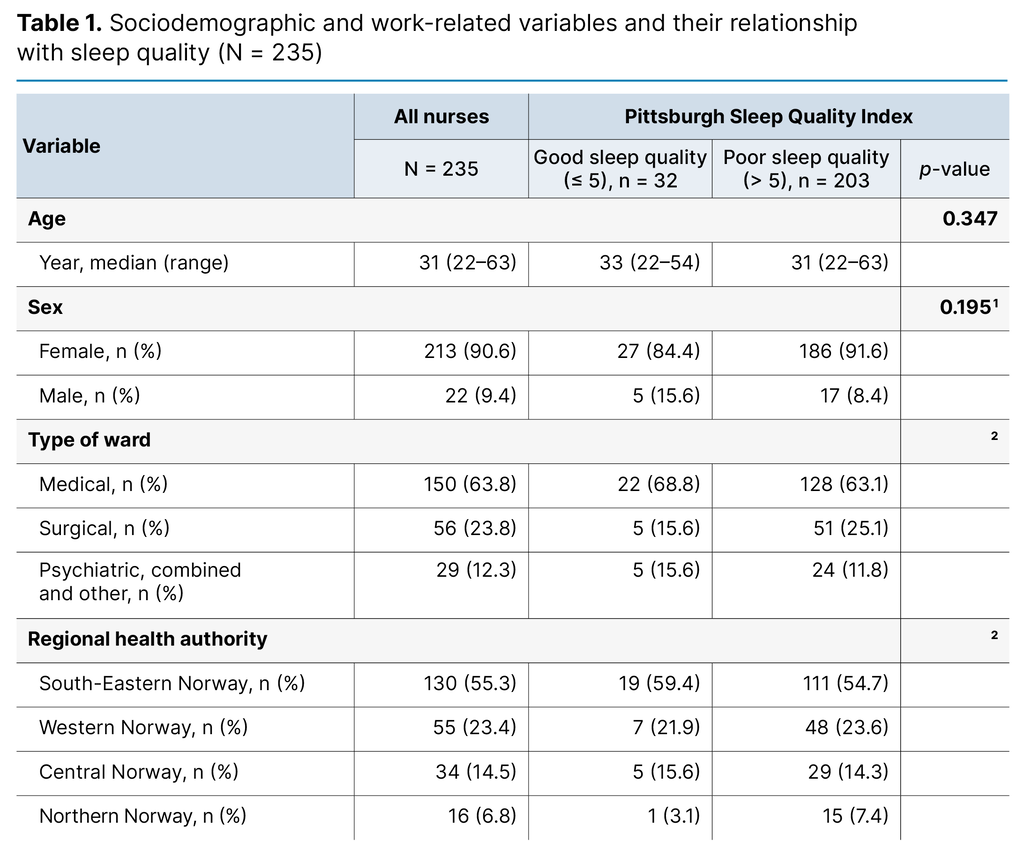
The survey received a total of 259 responses. Of these, 235 participants (90.7%) reported that they were working as a nurse on a hospital ward in the specialist health service, and they were included in the study. The participants had a median age of 31 years (range 22–63 years). The gender distribution was 90.6% female (213/235) and 9.4% male (22/235).
All counties in Norway were represented, with the highest number from Oslo and the fewest from Nordland. Over half (55.3%, 130/235) worked in South-Eastern Norway Regional Health Authority. The median work experience was 6 years (range 1–36 years). A total of 81.2% of participants (190/235) worked in a three-shift rota, while 61.1% (143/235) worked full time. Rest time between evening and day shifts varied between 8 and 10 hours, with 87.7% of participants (206/235) reporting a rest period of 9 hours.
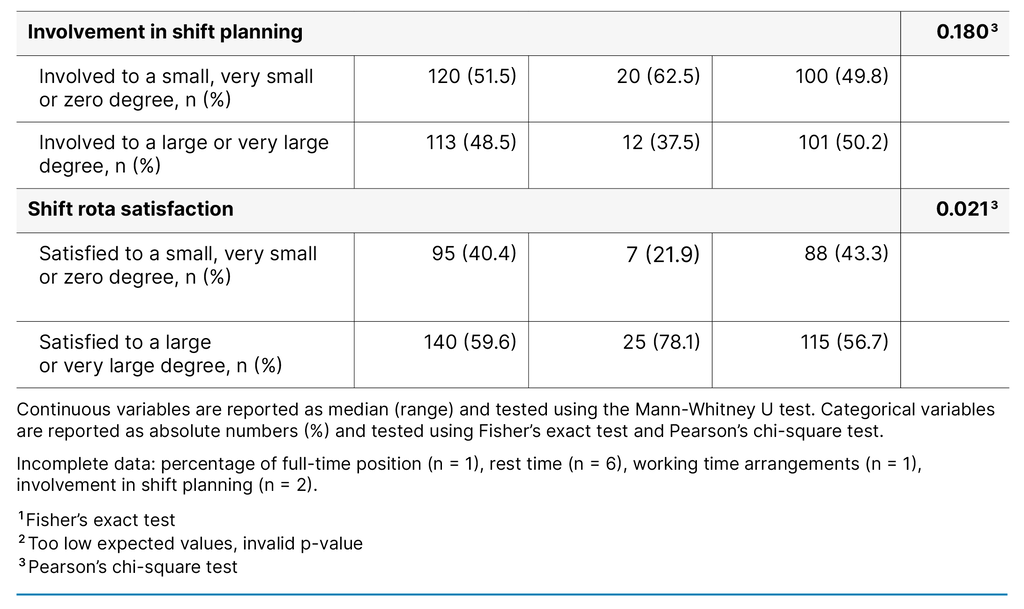
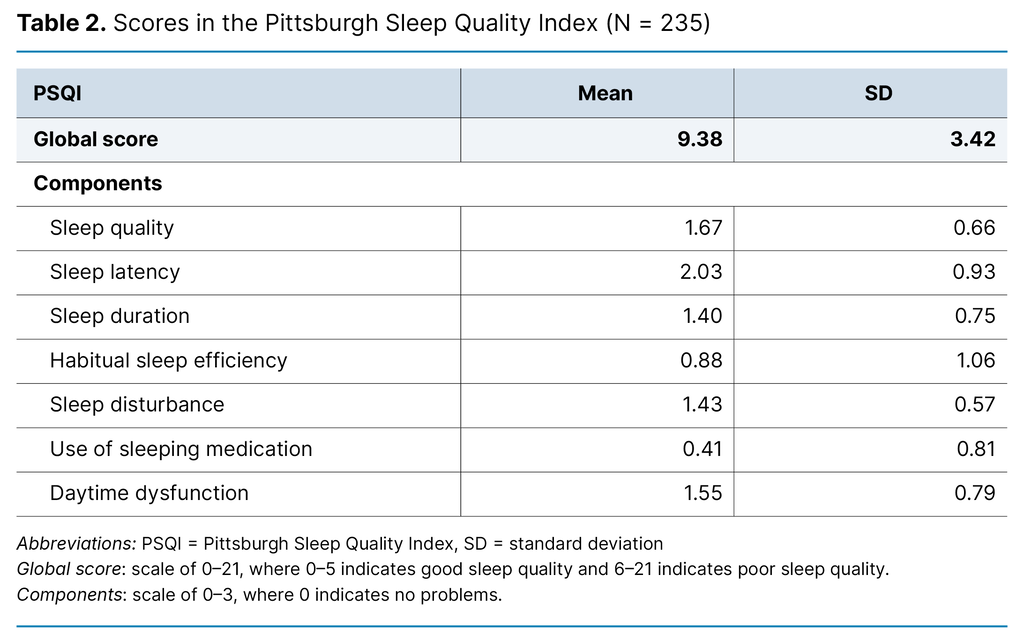
In the sample, 51.5% of participants (120/235) reported that they were involved in drawing up their own shift rota to a small, very small or zero degree. A total of 59.6% (140/235) stated that they were satisfied with their shift rota to a large or very large extent. Demographic and work-related data are presented in more detail in Table 1.
Differences between groups of good and poor sleep quality
Table 1 shows how sociodemographic and work-related data are distributed between the groups who reported good sleep quality and the groups with poor sleep quality. There was no difference across ages or between the sexes in terms of self-reported sleep quality. Neither were there any differences in work experience, percentage of full-time position, rest time between evening and day shifts, number of evening or night shifts, working time arrangements or involvement in shift planning.
A correlation was found between sleep quality and shift rota satisfaction. In the group of participants with poor sleep quality, 56.7% (115/203) were satisfied with their shift rota to a large or very large degree. In the group with good sleep quality, 78.1% (25/32) were satisfied with their shift rota (p = 0.021).
Nurses’ sleep quality
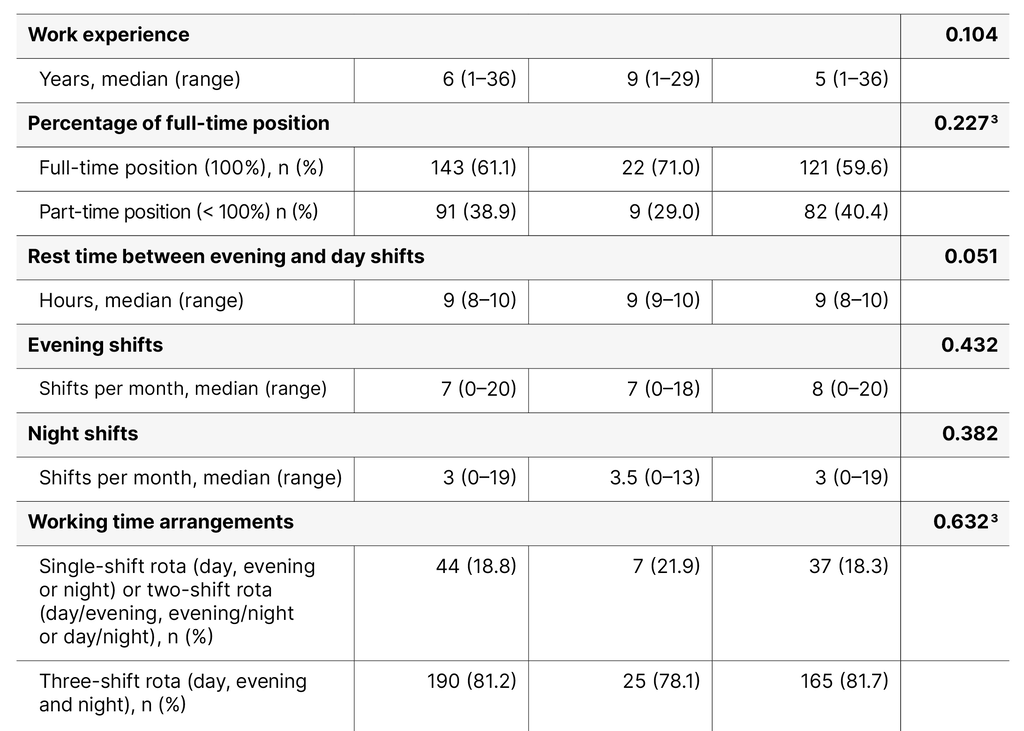
Table 2 presents the PSQI scores in the sample. The average PSQI score was 9.38 (SD 3.42, range 3–19). The mean scores for the PSQI components varied from 0.41 to 2.03. Among the components, sleep latency (mean 2.03, SD 0.93) had the highest score, indicating that many participants experienced long sleep onset times.
The use of sleep medication (mean 0.41, SD 0.81) had the lowest score, suggesting that few participants used any form of medication to help with sleep onset. The proportion of participants who reported poor sleep quality (PSQI > 5) was 86.4% (203/235).
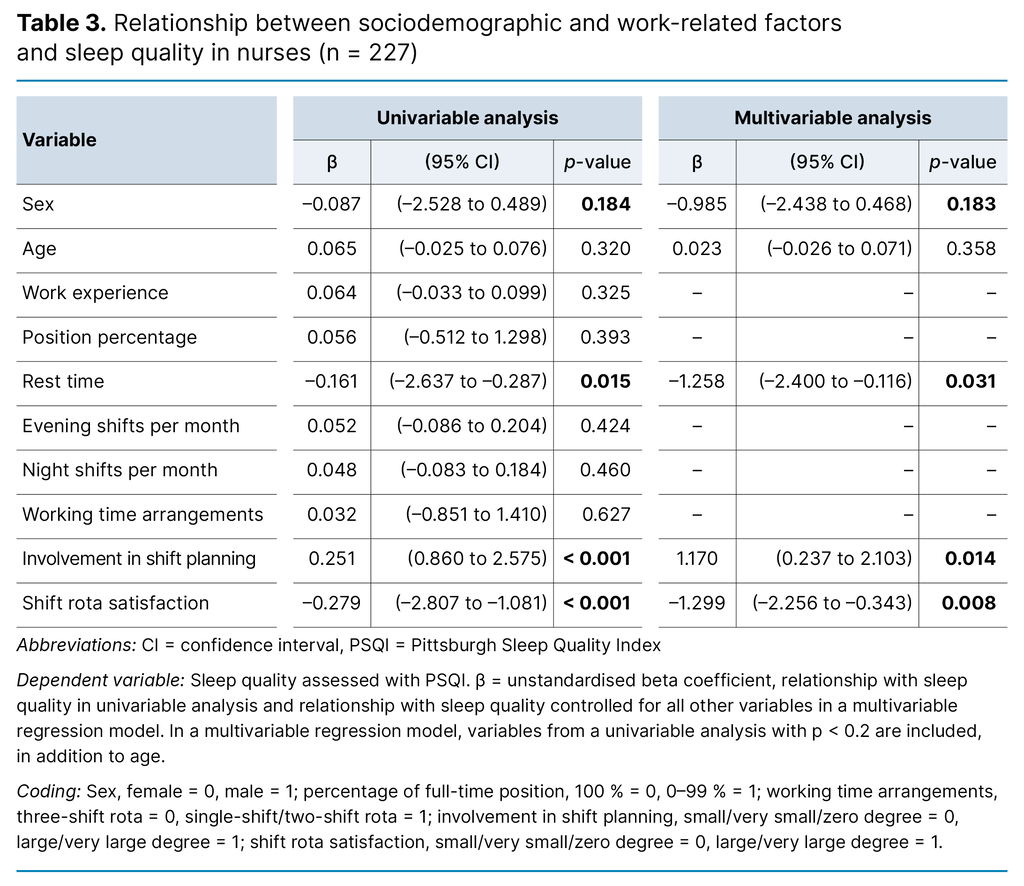
Relationship between sociodemographic and work-related factors and sleep quality
In the linear regression model examining the relationship between sociodemographic and work-related factors and sleep quality, a complete dataset was available for analysis for 96.6% of participants (227/235) (Table 3). Following the univariable analysis, sex, rest period, involvement in shift planning and shift rota satisfaction were included in the multivariable analysis. In the multivariable analysis, rest period, involvement in shift planning and shift rota satisfaction were associated with sleep quality (p < 0.050): for each additional hour of rest time, the PSQI score decreased by –1.26 (confidence interval [CI]: –2.4 to –0.1, p = 0.031).
The score of participants who were involved in drawing up their own shift rota was 1.17 (CI: 0.2 to 2.1, p = 0.014) higher than those who were not. For participants who experienced shift rota satisfaction, the PSQI score was –1.30 (CI: –2.3 to –0.3, p = 0.008) lower than for those who were not satisfied. The regression model as a whole explained 12.8% of the variance in reported sleep quality (R² = 0.128, adjusted R² = 0.109, p < 0.001).
Discussion
The objective of this study was to assess nurses’ sleep quality and the potential sociodemographic and work-related factors associated with sleep quality. The study participants were nurses working on wards in hospitals throughout Norway. The instrument used to measure sleep quality is well-established and frequently used in sleep quality research.
The main finding of the study was a very high proportion of participants with poor sleep quality. Other important findings were that participants who were satisfied with their shift rota reported better sleep quality than those who were not satisfied. Participants who were involved in drawing up their own shift rota reported poorer sleep quality than those who were not. Furthermore, longer rest periods between evening and day shifts were associated with better sleep quality.
Sleep quality of nurses on hospital wards in the specialist health service
The participants in our study had considerably lower mean PSQI scores and sleep quality compared to previous Norwegian research on nursing home staff (mean 5.70; SD 3.42; PSQI > 5 = 44.6%) and intensive care nurses (mean 7.5; SD 3.0; PSQI > 5 = 69.7%) (11, 21).
In addition to the global score being higher, the mean score in our study was higher on all components compared to nursing home staff in a Norwegian study (21). In an Italian study that measured sleep quality among nurses on hospital wards, the proportion with poor sleep quality was 88%, which is in line with the results of our study (7).
In an Iranian study, differences in sleep quality were also found among nurses on different types of wards (8). These results may suggest that nurses on hospital wards in the specialist health service have poorer sleep quality than comparable shift-working populations studied in Norway, and that sleep quality can vary across hospital departments.
Our study sample shows a bias in the gender distribution. However, it is close to the gender distribution among nurses employed in the health service in Norway in 2020 (26), and among nurses in the studies with nursing home staff and intensive care nurses (11, 21). The Italian study had a somewhat lower proportion of female participants (84.3%) (7). Neither sex nor age could be associated with sleep quality in our study.
In our study, there was no difference between the various working time arrangements and sleep quality. Previous research has not reached a consensus on which working time arrangements yield the best sleep quality. An Iranian study found that nurses with three-shift rotas had better sleep quality than nurses working just a single-shift rota (15), which is in contrast to findings for intensive care nurses in Norway (11).
The discrepancies in findings indicate a need for further studies in this area in order to compare participants’ different working time arrangements and sleep quality.
Shift rota satisfaction
Almost 80% of the participants in our study who reported having good sleep quality also stated that they were satisfied with their shift rota. The finding that nurses with high shift rota satisfaction experience better sleep quality aligns with results from a longitudinal study of Swedish nursing students who went on to work as nurses: short rest periods negatively affected both sleep quality and shift rota satisfaction, albeit only slightly (17).
Involvement in shift planning
A somewhat surprising finding in our study was that participants who indicated that they are involved in drawing up their own shift rota have poorer sleep quality than those who are not. Our data do not provide a causal explanation for this, and we were unable to find any research on this topic. It may relate to individual nurses’ ability to draw up optimal shift rotas – a field in which managers, health and safety personnel and union representatives typically have more expertise.
The Working Environment Act stipulates that if working hours are at different times of the day, the shift rota is to be drawn up in collaboration with union representatives, rather than unilaterally by the employer (4, section 10-3). Nevertheless, it could be argued that this result contradicts findings from a systematic literature review of the reasons people leave the labour force (18), which recommends that employers give employees the opportunity to be closely involved in shaping their working day (18). The result in our study is therefore difficult to explain, as employees who are involved in drawing up their shift rota are in a better position to adapt their shifts to their lives outside of work.
Rest time between evening and day shifts
None of the participants’ rest time between evening and day shifts exceeded the statutory minimum of 11 hours as provided for in the Working Environment Act (4, section 10-8[1]). Analysis of the number of hours in rest periods between evening and day shifts found very little difference in good and poor sleep quality between the groups with. However, a high proportion reported having nine hours of rest between these shifts.
Participants scored high in the PSQI component ‘sleep latency’, indicating that the sample population, on average, took more than 30 minutes to fall asleep at least once or twice a week. In the multivariable analysis, shorter rest periods were negatively associated with sleep quality, aligning with findings from studies involving nurses in Italy, Sweden and Norway, in which reduced sleep quality is associated with short rest periods (12, 17, 27).
Strengths and weaknesses of the study
Using the PSQI as a tool for measuring sleep quality is the subject of ongoing debate. Its use has been described as a strength in research because it provides a reliable, valid and standardised measure of sleep quality (10). However, it has been shown to be unsuitable for measuring the sleep quality of shift workers, as there are three key factors that can vary considerably from one week to another among this group: nocturnal sleep onset, sleep disturbances and sleep duration (23).
A majority of the participants worked three-shift rotas (81.2%). Over 40% of participants in our study and over 60% of participants in a corresponding Italian study reported good sleep quality, which was not in accordance with the global PSQI score results (7).
This finding may indicate that the threshold for good and poor sleep quality in the PSQI may be too low for shift-working nurses. Furthermore, the recruitment method employed in our study may have contributed to nurses with poor sleep quality being more inclined to participate in the study.
In our study, we categorised working time arrangements into two groups: three-shift rotas and two/single-shift rotas. This means that some participants with short rest periods between shifts are analysed together with participants who do not have short rest periods. A Taiwanese study found that shift workers who only work night shifts have shorter sleep duration than nurses with other working time arrangements (28).
Norwegian nurses have been shown to have a higher prevalence of insomnia when working two-shift rotas compared to when they only work night shifts (27). Our categorisation of working time arrangements may, therefore, have contributed to a bias in the groups when examining differences in reported sleep quality and the various working time arrangements.
Furthermore, it is a weakness of the study that we do not have information on participants’ levels of burnout, or mental health and insomnia, since these factors have been shown to affect shift workers’ sleep after a shift (28). If participants had responded to questions about their own sleep quality with a one-month interval, this would have provided a better basis for identifying which disturbances are temporary and which are long-term (3).
Research shows that differences have been found between women and men in terms of how they describe sleep quality. Women score higher (29) and view sleep quality as a combination of sleep disturbances and daytime dysfunction, while men relate sleep quality to sleep duration and sleep efficiency. The lack of differences between the sexes in our study may be related to the low number of male participants (9.4%, 22/235). The results of our study cannot, therefore, be generalised to male nurses.
Data were collected between late December 2020 and late January 2021. The COVID-19 pandemic had been ongoing for about a year at that time, and the pressure on the health service was particularly high. The tool for measuring sleep quality asks for responses to be related to the past month and does not account for any long-term variations in daily life, and this may have impacted on the results of our study.
Wang et al. examined the validity and reliability of the PSQI among doctors and nurses working with COVID-19 patients in Wuhan, China, at the start of the pandemic (30). The findings of the study indicate that the PSQI was reliable and valid for research on healthcare personnel, including during the pandemic (30).
The data for our study were collected during a period that included a national holiday, when workloads and capacity in the health service are lower than usual. No account was taken of possible reduced activity in either the questions or analyses, but the deviation from normal activity may have impacted on participants’ self-reporting of sleep quality over the past month.
Although the linear regression model in the study was statistically significant (p < 0.001), it explained only 12.8% of the variance in reported sleep quality. This result indicates that much of the variation in sleep quality cannot be explained by the included variables but by unknown factors outside the scope of the study.
Conclusion
The results of this study clearly indicate that nurses on hospital wards in the Norwegian specialist health service have poorer sleep quality than other comparable groups. For nurses on hospital wards in the specialist health service, it appears that rest time, involvement in shift planning and shift rota satisfaction are factors associated with sleep quality, and should therefore be the subject of future studies.
The author declares no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge

Comments