Rehabilitation ward holiday closure and the course of sepsis
Summary
Background: Rehabilitation after critical illness improves functional outcomes, but in some countries, specialised rehabilitation wards are closed during holidays.
Objective: This study aimed to compare the length of hospital stay, discharge destination and survival in sepsis patients who were hospitalised during and outside holiday periods over 10 years.
Method: In a registry-based cohort study, 1,552 consecutive patients who had their first-time admission due to sepsis between 2003 and 2013 were included. Length of hospital stay, discharge destination and survival in patients hospitalised during (n=481) and outside (n=1071) holiday periods were compared.
Results: Patients hospitalised during holiday periods had a longer length of stay compared with patients hospitalised outside holiday periods (median 9 vs. 7 days, p<0.001, mean 14.5 vs. 11.2 days, 95% CI 1.6–5.0, p<0.001). The difference was even larger in a subgroup of patients (n=332) who were admitted to an intensive care unit or a monitoring unit (median 13.5 vs. 9 days, p<0.001, mean 22.8 vs. 15.2 days, 95% CI 2.5–12.8, p=0.004). There were no differences in discharge destination or survival between the groups.
Conclusion: We found that closing a rehabilitation ward during holidays prolongs the length of hospital stay in patients with sepsis. This may lead to increased costs and increased risk of complications, and it may be a burden for sepsis patients who want to return to normal life as soon as possible.
Cite the article
Thingstad A, Gustad L, Skei N, Lydersen S, Sagberg L. Rehabilitation ward holiday closure and the course of sepsis . Sykepleien Forskning. 2024;19(96226):e-96226. DOI: 10.4220/Sykepleienf.2024.96226en
Introduction
Sepsis leads to organ failure due to a dysregulated immune response to common infections, including bloodstream infections (BSIs) (1, 2). As sepsis patients are often in need of organ support (3), sepsis is one of the most common reasons for admission to an intensive care unit (ICU) (4) and the most common cause of death in hospitals (5).
Even with intensive care, sepsis mortality remains high, accounting for 11 million lives lost annually across the world (1). In population-based data, the overall mortality within 30 days for patients with infection and a positive blood culture is reported to be 15.8% (6).
For adult survivors, severe sepsis is associated with both functional and mental limitations (7), demanding a long and comprehensive individualised recovery process, with care delivered by multidisciplinary team members (3). Guidelines recommend that patients with critical illness start rehabilitation as early as clinically possible (8), and early rehabilitation in the ICU is a well-proven treatment to improve functional outcomes (9, 10).
Recent sepsis guidelines also recommend referral to a post-critical illness follow-up programme, if available (3). These guidelines state that evidence on effects of rehabilitation after the critical care phase is scarce, highlighting the need to gather evidence from different healthcare delivery systems (3).
During holiday periods, post-acute sepsis patients’ rehabilitation trajectories may be limited by a lack of staff members or even by unavailability of rehabilitation facilities. However, the impact of multidisciplinary rehabilitation wards closed during holidays and sepsis patients’ trajectories – including length of stay, discharge destination and long-term outcomes – is still unknown (11).
This study aimed to understand the impact of closing specialised rehabilitation wards during holidays on patients’ length of stay, discharge destination and survival over a 10-year period.
Method
Study design and study population
In this registry-based cohort study, data were extracted from the Nord-Trøndelag Hospital Trust’s (HNT HF) hospital-based Sepsis Registry at Levanger Hospital, Norway (12): a community hospital for approximately 100,000 inhabitants. All patients aged ≥18 years who had their first admission and were included in the Sepsis Registry between 2003 and 2013 were included in this study.
The Sepsis Registry and local routines
The HNT HF Sepsis Registry is a medical quality and research register established in 1994 for surveillance purposes. At the time of sepsis suspicion, all patients underwent a standard clinical examination to decide on a diagnosis. Blood cultures were drawn prospectively at the time of suspicion and routinely assessed by a microbiologist to evaluate the possibility for contamination.
All patients with clinically suspected sepsis and confirmed BSI in two sets of blood culture bottles (BACTEC 9240 Vacutainer Culture Bottles until 2010, hereafter BACTEX FX (13)) were included in the Sepsis Registry. Clinical variables from electronic medical records were obtained by a trained research team and quality checked by an experienced consultant in infection medicine. All patients received information regarding inclusion in the registry and were given the option to withdraw.
Dependent on treatment needs, the sepsis patients were either admitted to a general medical ward, a monitoring unit (MU) or an ICU for more specialised care. After medical treatment, patients in need of interdisciplinary specialised rehabilitation were commonly transferred to a rehabilitation ward at the same hospital.
Since its opening at the end of 2002, the rehabilitation ward has been closed during holidays: for four weeks in July/August and during Christmas and Easter each year (see details in Appendix 1). In the present study, the holiday period is defined as one week before the rehabilitation ward closes until one week after reopening (patients admitted in this period are usually affected by the closed ward).
Data collection
Baseline and clinical variables – including length of stay, discharge destinations and survival – were retrieved from the Sepsis Registry. Data on discharge destination was not available before 2008. Functional status before sepsis hospitalisation was recorded as ‘independent’ when the patient lived at home without assistance, ‘partly independent’ if the patient lived at home with some assistance and ‘dependent’ if the patient either lived at home and received help with most daily life activities or in a nursing home or similar institution (14).
We also calculated the Charlson Comorbidity Index (CCI) (15) and the Sequential Organ Failure Assessment (SOFA) score (2). The SOFA score is a validated scoring system that measures the degree of acute organ failure in six organs (respiratory, cardiovascular, hepatic, coagulation, renal and neurological systems) (2).
Statistical analyses
Descriptive statistics are reported as median and interquartile range (IQR) for continuous variables and as count and percentage for categorical variables. Groups were compared for baseline differences using the t-test for continuous variables, the Wilcoxon–Mann–Whitney test for ordered categorical variables and the Pearson chi-squared test for dichotomous variables. Length of stay was calculated as the number of full days from the date of hospital admission to the date of hospital discharge.
Since means could be more relevant than medians when estimating costs and the need for health workers (16, 17), both medians with IQR and means with standard deviations (SDs) are presented for the length of stay, since the data were right-skewed. The differences in length of stay were assessed using the independent samples t-test, not assuming equal variances. This version of the t-test is robust to deviance from normality (18).
For discharge destination and survival at 30 and 90 days, the Pearson chi-squared test was used. Survival time was assessed from the time of the first admission to death (end of follow-up 31 December 2021). We used Cox regression to assess differences in survival between groups adjusted for age, sex, baseline functional status, comorbidity and SOFA score. The proportional hazard assumption was confirmed by visual inspection of Schoenfeld residual plots and log-log plots. We regarded a two-sided p-value <0.05 to represent statistical significance, and 95% confidence intervals are reported where relevant. Data were analysed using SPSS 27 and Stata 17.
Ethics and approvals
This study was approved by the HNT HF’s Data Access Committee (reference 2021/1221 - 9248/2021) and the Regional Committee for Medical and Health Research Ethics, Health Region IV in Norway (REK reference 230377).
Results
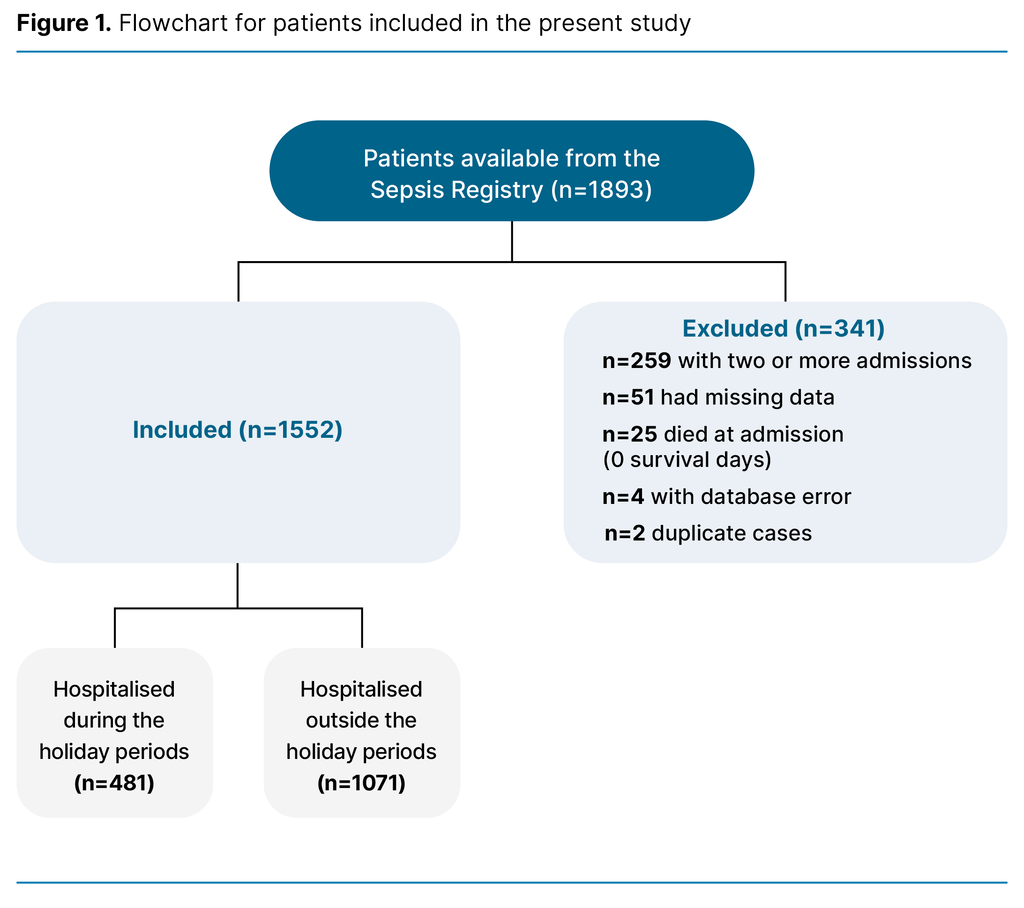
Of the 1,893 eligible patients, a total of 1,552 were included in the analysis. A flowchart for the inclusion process is presented in Figure 1. Of these, 481 patients were hospitalised during the holiday periods, while 1,071 patients were hospitalised outside the holiday periods. Baseline characteristics for patients admitted to the hospital during versus outside holiday periods are presented in Table 1, and there were no statistically significant differences between the groups.

The severity of illness and treatment characteristics were also similar for patients admitted to the hospital during holiday periods versus outside holiday periods (Table 2).

Length of hospital stay
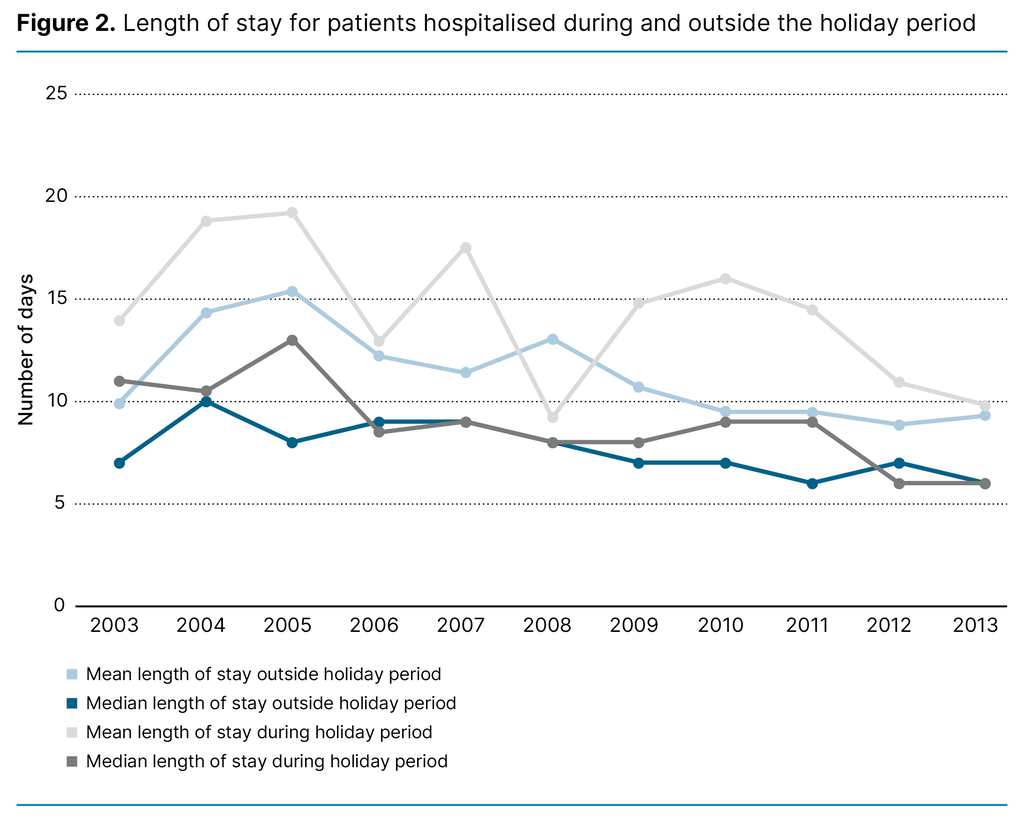
The median length of stay was 9 days (IQR 5–17) for patients hospitalised during the holiday periods, compared with 7 days (IQR 5–12) for patients hospitalised outside the holiday periods (p<0.001). The mean length of stay was 14.5 days (SD 16.9) and 11.2 days (SD 13.3), respectively (mean difference of 3,3 days, 95% CI 1.6–5.0 days, p<0.001). As seen in Figure 2, there was a subtle, gradual decrease in the length of stay from 2003 to 2013, and the differences varied over the years.
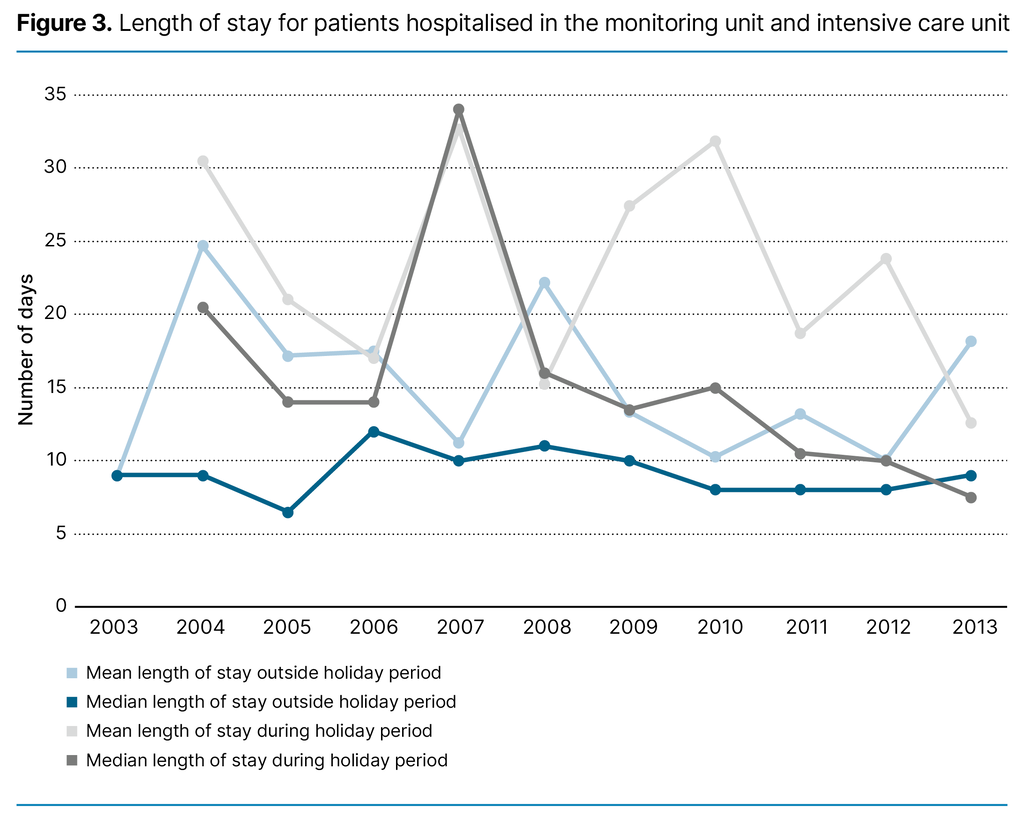
A subgroup analysis was performed on the 332 patients who were admitted to the MU and ICU, where 102 (30.7%) were hospitalised during the holiday periods and 230 (69.3%) were hospitalised outside the holiday periods. In this subgroup, the median length of stay was 13.5 days (IQR 7–28.3) during the holiday periods, compared with 9 days (IQR 5–16) outside the holiday periods (p<0.001).
The mean length of stay during the holiday periods was 22.8 days (SD 23.4), compared with 15.2 days (SD 18.1) outside the holiday periods, with a mean difference of 7.6 (95% CI 2.5–12.8, p=0.004). The length of stay over time is shown in Figure 3.
Discharge destination
Discharge destination was recorded from 2008, thus we have complete data for 601 patients (n=414 (68.9%) outside the holiday periods and n=187 (31.3%) during the holiday periods). The distribution of discharge destinations between groups did not differ (p=0.739). Of the patients hospitalised during the holiday periods, 60.4% (113/187) were discharged to their residence versus 58.0% (240/414) of the patients hospitalised outside the holiday periods (p=0.571).
Further, 17.6% (33/187) were discharged to a nursing home or rehabilitation facility in the municipality during the holiday periods versus 16.7% (69/414) (p=0.767) outside the holiday periods. Transfer to another hospital occurred in 4.8% (9/187) in the holiday periods versus 4.3% (18/414) (p=0.799) outside the holiday periods. Discharge to a district medical centre occurred in 17.1% (32/187) of the patients during the holiday periods versus 21.0% (87/414) (p=0.266) outside the holiday periods.
Survival
A total of 13.5% (65/481) of the patients hospitalised during the holiday periods died within 30 days, compared with 15.1% (162/1071) in the other group (p=0.406). The proportion who died within 90 days was 21.8% (105/481) during the holiday periods, compared with 21.7% (232/1071) outside the holiday periods (p=0.941).
The hazard ratio (HR) for survival did not differ between groups; moreover, the patients hospitalised during holiday periods had an HR of 1.01 (95% CI 0.89-1.15) for death when adjusted for baseline characteristics, compared to the reference group that was admitted with sepsis during non-holiday periods (p=0.843). This estimate did not change with adjustment for two or more organ failures during hospital stay, as measured by a categorical SOFA score (value 0 if 0–1 organ failures, value 1 if 2 or more organ failures).
Discussion
In this study, we found that the sepsis patients admitted to the hospital during the holiday periods had a median 2 days longer and mean 3.3 days longer hospital stay, compared to patients who were hospitalised in non-holiday periods. In sepsis patients in need of MU or ICU treatment, the length of stay was a median 4.5 days and mean 7.6 days longer during the holiday periods. However, there were no differences in discharge destinations or survival between the two groups.
Previous studies in intensive care have reported positive outcomes for general patients and sepsis patients receiving early rehabilitation (9, 10, 19). Severe sepsis is associated with both physical and cognitive deficits (7), and the required rehabilitation can be complex. Thus, sepsis patients may have considerable potential for improvement.
Since prolonged length of stay is associated with an increased risk of complications and mortality (20, 21), the complication rates could have been increased during holiday periods, although this was not assessed in the present study. In addition, one study shows that rehabilitation provided on a general ward can be suboptimal and that some deaths following ICU discharge can be avoided (22).
However, we did not find any differences in survival between the groups in our study, and this may reflect a successful implementation of sepsis care bundles that secure good quality care both during and outside of the holiday periods. It is important to note the severe burden of sepsis that was demonstrated in our study: 1 out of 7 died within 30 days and one fifth after 90 days. The 30-day mortality rate corresponds to data from Denmark (6).
An increased length of stay may also lead to a delayed start of necessary interdisciplinary rehabilitation (23) and be a burden for the patients. However, a small study demonstrated ward-based rehabilitation to be feasible if interprofessional coordination is ensured: the study found no difference in outcome with or without treatment in a specialised rehabilitation ward for sepsis patients (24).
Our study supports these findings. Nevertheless, there might be a risk of higher patient occupancy at the other wards due to closed rehabilitation wards, which could result in less time for healthcare workers to follow up on all patients. Further studies should therefore assess the outcome of all patient groups to obtain an overall overview of the consequences of closed rehabilitation wards.
Increased patient occupancy in the wards could also contribute to the need for extra personnel at work, and the cost of bed days at the medical ward, the MU or the ICU might be higher than at the rehabilitation ward. However, keeping a rehabilitation ward closed during holidays may also save costs, and further studies are needed to investigate the economic aspects of this issue.
A subtle decrease in hospital stay was found from 2003 to 2013 in our study, which corresponds to data from both Denmark and the United States (6, 25). This may reflect more efficient treatment over time or an increased incidence of discharge to an external health institution (6) where the treatment can be continued. However, the difference in length of stay between the two groups varied over the years and seemingly decreased towards the end of the period. This could potentially be explained by natural fluctuations, but it may also be a result of the 2012 Norwegian Coordination Reform (26).
This reform aimed to place responsibility upon the municipalities for patients ready for discharge, which has shown to decrease hospital stay and increase stay in municipal care (27). Based on this, the outcome in our study regarding discharge destination might have been different if the study had more recent data. In 2017, the national patient safety programme for early detection and treatment of sepsis was also implemented, and future studies should investigate whether this trend continues (28).
Strengths and limitations
A strength of our study is the large sample size and the use of population-based data, leading to a high degree of external validity. However, it is possible that the most critically ill patients are most affected by holiday closures, since they are at higher risk of functional disability. Consequently, the study may have yielded different results if only this group of patients had been included.
A limitation of our study is the use of historical data. At the time, sepsis was characterised by the systemic inflammatory response syndrome (SIRS) in response to an infection (Sepsis 2-definition) (2). However, sepsis is an evolving field in critical care, and limitations with this definition were later recognised. The Sepsis 3 definition was introduced in 2016 and identifies sepsis as a dysregulated host response to infection resulting in life-threatening organ dysfunction (2).
Considering the refined definition of sepsis, it is possible that a study utilising more recent data could have included patients with more severe illness. Regardless, since this study has a substantial sample size and the estimates for survival between the groups did not change with adjustments for SOFA score, the potential influence this has on the outcomes is likely minimal. We also find the topic to be highly relevant.
Prioritising rehabilitation for sepsis survivors might be imperative, given the escalating incidence of sepsis (29) and concurrent decline in mortality rates (30). Studies have shown that only two thirds of the non-ICU sepsis patients and half of ICU sepsis patients have resumed work at two years (31). Efficient rehabilitation not only addresses the physical and cognitive impairments experienced by sepsis survivors, but could also contribute to expedited recovery, potentially reducing the burden on healthcare resources.
Conclusion
We found that closing a rehabilitation ward during holidays prolonged the length of hospital stay in patients with sepsis but did not affect discharge destinations or survival. This may lead to increased risk of complications and be a burden for sepsis patients. Further studies are needed to investigate the economic aspects of this issue.
Acknowledgements
We want to thank the clinicians and other employees involved with the HNT HF Sepsis Registry for their support and for contributing to the data collection in this research project. This work was partly supported by grants from the HNT HF. The funder played no role in the design, interpretation or decision to publish the analysis presented herein.
Funding
This work was partly supported by grants from Nord-Trøndelag Hospital Trust. The funder played no role in the design, interpretation, or decision to publish the analysis presented herein.
Conflicts of interest
Lise Tuset Gustad declare a conflict of interest as she is editor-in-chief (EIC) in Sykepleien Forskning. She did not participate in the handling or decision-making process concerning this submission. The manuscript was overseen by an appointed EIC to ensure impartiality and fairness in the review and editorial process.
Open access CC BY 4.0
The Study's Contribution of New Knowledge

Comments