Nurse-performed ultrasound-guided nerve block for hip fracture patients
Summary
Background: Ultrasound-guided fascia iliaca compartment block (US-FICB) is an important procedure for minimising opioid use during perioperative pain management for the expanding demographic of elderly patients with hip fractures. Nurse anaesthetists with specialised skills are emerging as valuable assets for the efficient delivery of this nerve block. Despite the growing implementation of US-FICB, studies have not yet detailed how its pain relief effects differ between men and women, or the differentiation of the effect on pain at rest and with movement. This study aims to evaluate the analgetic effect of US-FICB administered by nurse anaesthetists in patients with hip fractures, with a specific focus on variations based on the patient’s sex and the intensity of pain at rest and during movement.
Design: Prospective observational study involving systematic data collection to observe the effects of US-FICB in a clinical setting.
Method: Pain intensity at rest and with movement was recorded on a numeric rating scale (0–10). Then, nurse anaesthetists administered a US-FICB. After 60 minutes, pain intensity at rest and during movement were recorded once more. A decrease of 1.5 points was deemed clinically significant.
Results: Of the 33 patients with complete datasets, the mean pain reduction after US-FICB was 1.4 (95% CI: 0.5–2.4) for pain at rest and 2.6 points (95% CI: 1.8–3.5) for pain during movement. Clinically significant pain relief was noted in 17 patients (51.5%) at rest and 23 patients (69.7%) during movement. A high initial pain intensity at rest was a statistically significant predictor for the procedure’s effect (odds ratio 1.6; 95% CI: 1.1–2.3; p<0.01). The study did not reveal significant sex-based differences, but the sample size may not have been adequate for this determination. No serious adverse effects were recorded.
Conclusion: Nurse anaesthetist-delivered US-FICB can offer notable pain alleviation for hip fracture patients, particularly for movement-induced pain and for patients initially reporting high pain intensities.
Cite the article
Dahlen S, Temmesfeld M. Nurse-performed ultrasound-guided nerve block for hip fracture patients. Sykepleien Forskning. 2024;19(95976):e-95976. DOI: 10.4220/Sykepleienf.2024.95976en
Introduction
Hip fractures (HF) are an emerging worldwide public health challenge for the increasing geriatric population with an estimated annual global incidence of 14.2 million hip fractures in 2019 and an expected rise of 50% in 2050 (1, 2). In Norway, the annual hip fracture incidence is 166 per 100 000 inhabitants, and among the highest worldwide (3). Surgical treatment is mandatory for all patients except moribund patients, class V according to the American Society of Anesthesiologists (ASA) classification (4).
In Norway, the mean age of patients undergoing surgery for HF is 80 years, and 66% are women (3, 5). At hospital admission, hip fracture patients often experience severe pain. Acute confusion occurs in approximately 40% of older HF patients and uncontrolled pain is thought to increase the risk of developing delirium (6, 7).
Regional nerve blocks are a recommended supplement to oral and intravenous pain management to avoid side effects of the latter, including delirium, nausea, vomiting, rebound pain and altered mental state (4, 8). For example, in Lim et al.’s retrospective study of 252 hip fracture patients, regional nerve blocks reduced the incidence of delirium by about 45% (9). In particular, the ultrasound-guided fascia iliaca compartment block (US-FICB) has gained popularity in recent years, due to its relatively simple and safe application (10).
In a retrospective cohort study with 98 patients, US-FICB at hospital admission reduced opioid consumption and length of hospital stay in geriatric hip fracture patients to a statistically significant degree (11). However, the literature is conflicting: for example, in Salottolo et al.’s observational cohort study with 517 geriatric hip fracture patients, fascia iliaca compartment blocks neither decreased opioid consumption nor the incidence of delirium (12).
Our institution has implemented a fast-track system for geriatric hip fracture patients, which included the routine application of an FICB without ultrasound guidance by the orthopaedic surgeon on duty. However, there was some evidence for a superior analgetic effect of ultrasound guided FICB, compared to a non-instrumental method, often referred to as the ‘landmark approach’ (13, 14).
Additionally, the use of ultrasound guidance can significantly reduce the incidence of local anaesthetic systemic toxicity (LAST) in older patients (15).
Nevertheless, the abundance of hip fracture patients, combined with the limited availability of orthopaedic surgeons and anaesthesiologists, can compromise a swift and efficient US-FICB application. Nurse anaesthetists are highly qualified personnel and experienced with ultrasound-guided procedures. They can be a valuable resource to ensure adequate pain management in that fragile patient population. Gawthorne et al. demonstrated equal results and complication rates for US-FICB performed by nurses compared to medical doctors (6).
In our institution, nurse anaesthetists have performed US-FICB since 2019 with about 750 procedures in 2023 alone. Except for one case of a transient blood pressure drop without further consequences, no complications were reported. Given that a predominant number of hip fracture patients are female and recent neurobiological studies indicate notable differences in pain perception between the sexes, differentiating between male and female patients is of significance for optimising pain management strategies (16).
This study aims to evaluate the analgetic effect of nurse anaesthetist-administered US-FICB on pain intensity at rest and pain intensity during movement, differentiated by the patient’s age and sex. Furthermore, we aim to describe possible factors for the success of the procedure.
Method
Study design
Prospective observational study, compliant with the ‘Strengthening the Reporting of Observational Studies in Epidemiology’ (STROBE) guidelines (17).
Ethical aspects
The current study was approved by the Regional Ethics Committee (reference REK 2021/265106), and Akershus University Hospital’s data protection officer (reference 2021_159 21/0898). Patients provided informed written consent. Patients were not refused supplemental oral pain medication and received the same level of care as in guideline-based routine clinical practice.
Setting and eligibility criteria
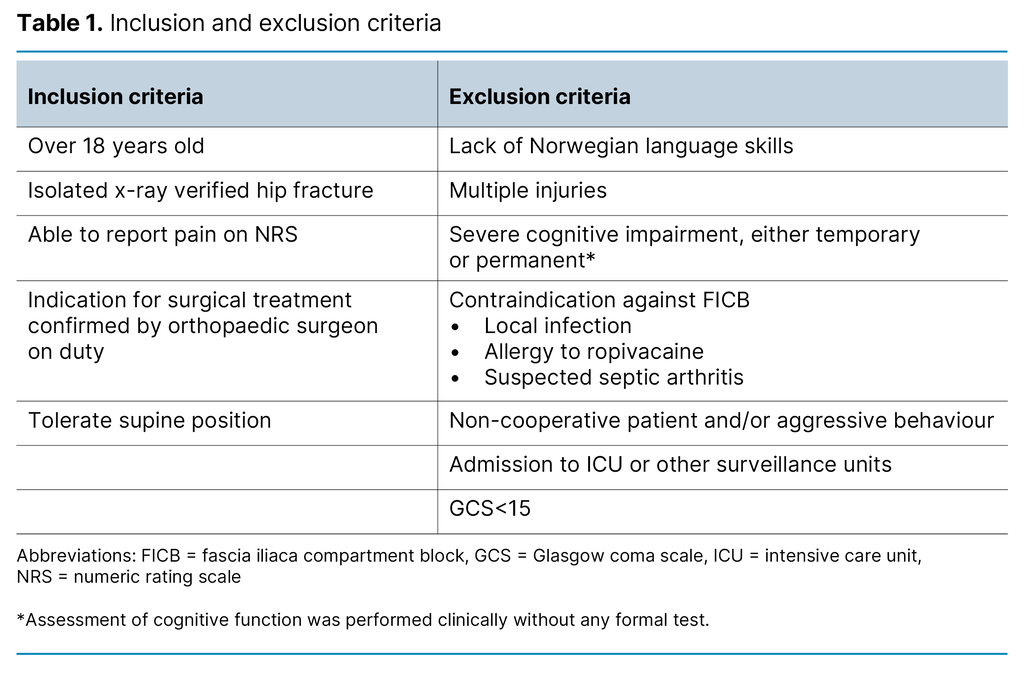
Patients over 18 years of age admitted to Akershus University Hospital with a radiologically verified isolated hip fracture between September and December 2021 were eligible for the study. Hip fracture was defined as either femoral neck fracture or trochanteric fracture, including subtrochanteric fracture, classified as 31-A1-3 and 31-B1-3 according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) and the Orthopaedic Trauma Association (OTA): Detailed inclusion and exclusion criteria are summarised in Table 1.
The initial physical examination was performed by the orthopaedic surgeon, who reconfirmed the diagnosis and set up a treatment plan, including the prescription of the US-FICB. The patient’s pain intensity was recorded by staff nurses using a numeric rating scale (NRS) ranging from 0–10, where 0 indicated no pain and 10 represented the worst pain imaginable. Pain at rest was documented both before and after the US-FICB procedure.
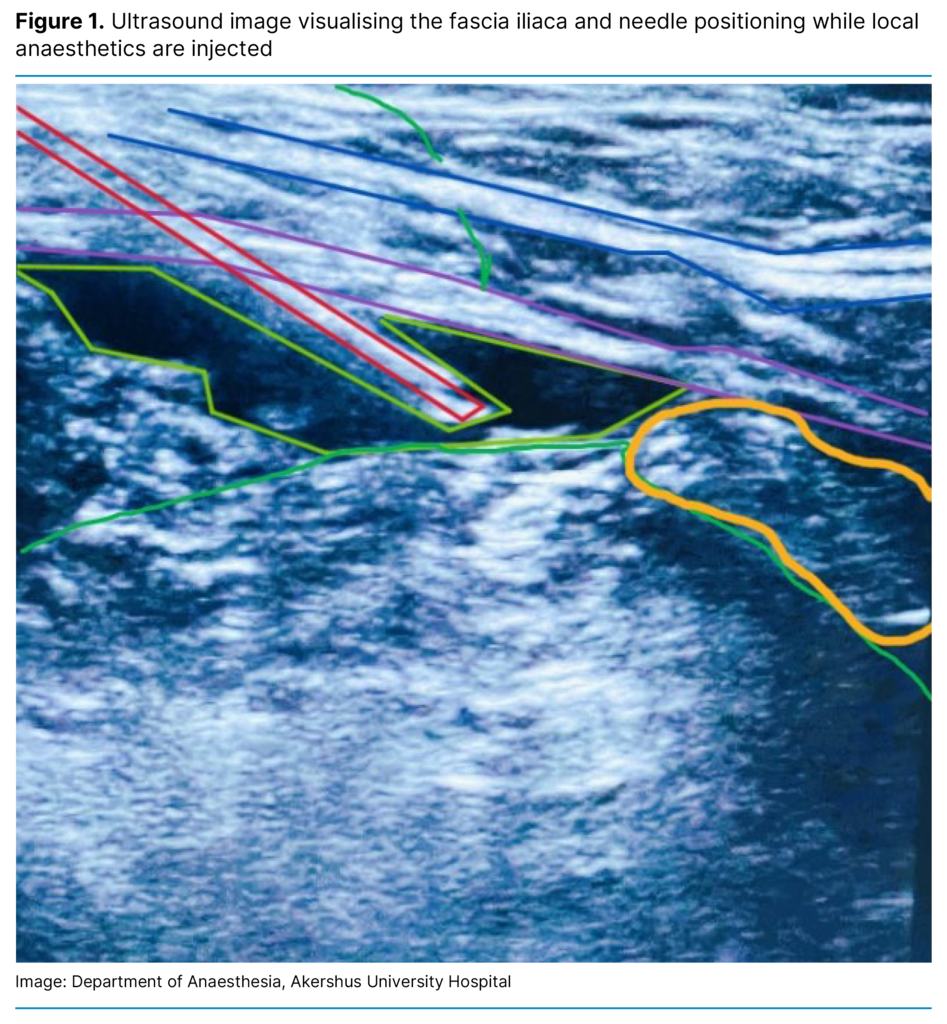
For the assessment of pain during movement, upon initial assessment, pain intensities were gauged when patients actively moved in bed. Nurse anaesthetists performed the US-FICB according to a standardised procedure implemented in our hospital. In brief, 20 ml of 0.9 mg/ml sodium chloride and 20 ml of ropivacaine 5mg/ml solution were mixed into a 40 ml solution and subsequently injected beneath the fascia iliaca, approximately 1–2 cm lateral to the femoral nerve under ultrasound guidance. See Figure 1.
The details of the procedure are described in Appendix 1. All five nurse anaesthetists participating in the study had previously received four hours of theoretical training and had performed a minimum of 20 US-FICB procedures under supervision. After 60 minutes, staff nurses measured pain intensity using the NRS at rest and during movement again. Pain during movement after US-FICB was recorded by inserting a wedge underneath the patient’s femur, resulting in 20˚ hip and 40˚ knee flexion. In addition to NRS for pain measurement, the age and sex of the patient were recorded.
Success in pain relief was defined as the minimal clinically important difference (MCID) of ≥ 1.5 difference on the NRS, in accordance with Bijur’s MCID study for using NRS for pain measurement on 195 older patients (18).
Data analysis
The primary outcome in the present study was the change in pain intensity (NRS) before and after the US-FICB. Data were analysed with descriptive statistics for the whole study sample and for females and males, respectively. A two-tailed paired Student’s T-test was performed for the NRS scores recorded before and after US-FICB. Significant differences were assumed at alpha ≤ 0.05. A posthoc power analysis was provided for each Student’s T-test.
Logarithmic regression: the study population was divided into a ‘success’ and ‘no-success’ group, depending whether US-FICB reduced pain intensity with a minimum of 1.5 points on NRS or not. This was performed for both pain at rest and pain during movement. We postulated that the US-FICB procedure was especially efficient in patients with high initial NRS scores. Hence, we hypothesised that pain intensity measured before administering US-FICB could independently predict the chance of success for the treatment.
Two logarithmic regressions were modelled, one for pain at rest and one for pain with movement. The independent variables were age, sex and pain intensity assessment (NRS) before administering US-FICB. The dependent variable was the success of the procedure for pain at rest and pain during movement, respectively, as defined above.
Data were analysed with Stata 16 (Statacorp LLC, College Station, TX, USA).
Results
Descriptive statistics
A total of 35 eligible patients were included and received US-FICB from nurse anaesthetists. No adverse events were reported. Data from two patients were not included in the analysis due to missing NRS recordings. Out of 33 patients with complete datasets, 21 were female (63.6%).
The mean age was 78.6 years (95% CI: 74.6–82.7). Pain intensity (NRS) was normally distributed, except for pain intensity during movement before administering US-FICB. There was no association between the sexes in initial pain intensity, neither at rest nor during movement, but the sample size was underpowered (1-β=36.5%). Nor did we find any statistically significant difference between the sexes in pain reduction after US-FICB.
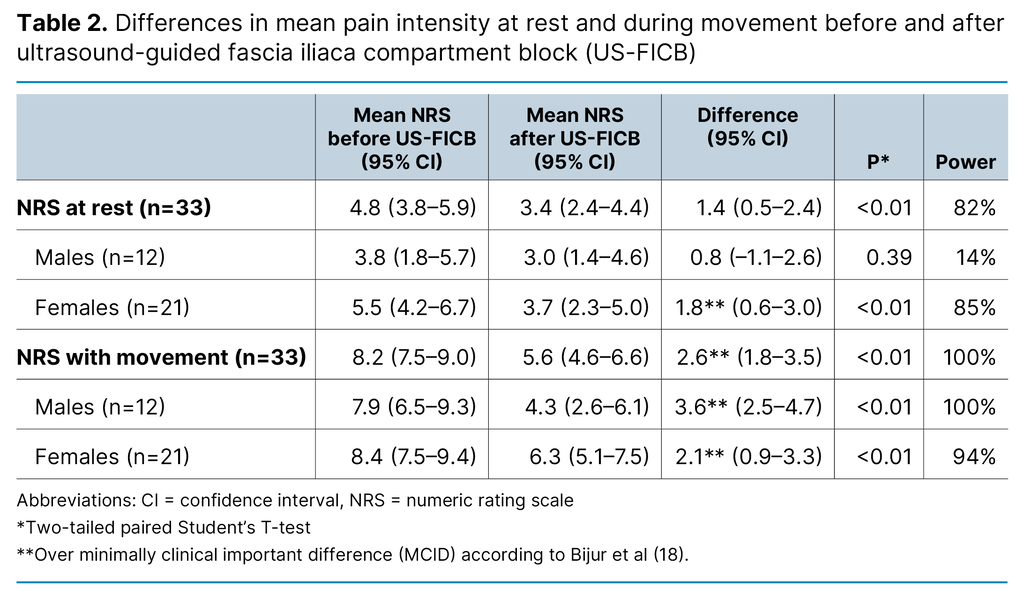
Pain intensity on the NRS scale was lower after US-FICB for pain at rest for females and for pain during movement for both sexes, to a statistically significant and clinically important extent. Further details are summarised in Table 2.
Stratifying (success/no success)
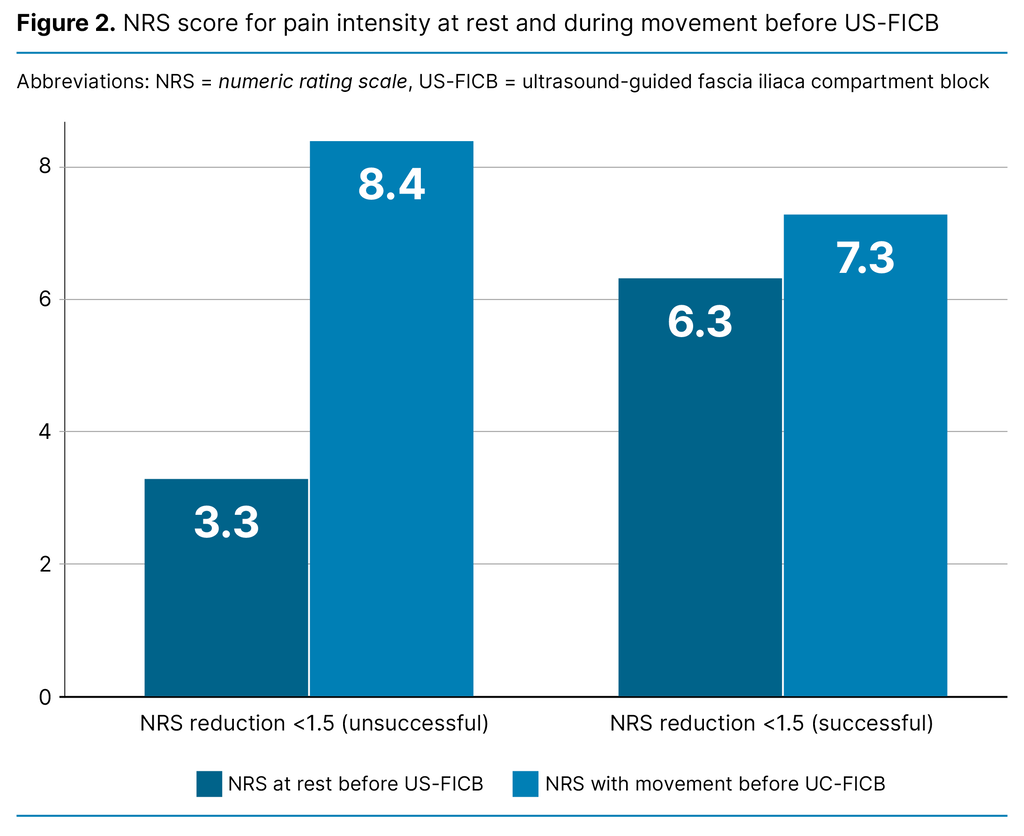
A reduction of minimum 1.5 NRS points for pain intensity was recorded in 17 patients for pain at rest, and in 23 patients for pain during movement. Patients who reported a minimum 1.5-point decrease in the NRS after the US-FICB (defined as success) reported a higher NRS score, i.e. more pain at rest before the procedure (6.3; 95% CI: 5.1–7.4), compared to patients whose NRS decreased by less than 1.5 points (3.3; 95% CI: 1.8–4.8). That difference of three NRS points was statistically significant, and the sample was adequately powered for this question (Student’s T-test; p<0.01; 1-β=93%).
Logarithmic regression
NRS scores at rest before US-FICB were associated with the success of the procedure (odds ratio 1.6; 95% CI: 1.1–2.3; p<0.01). However, for pain experienced during movement, NRS scores before US-FICB were not significantly associated with success (OR 0.98; 95% CI: 0.7–1.4; p=0.9), nor were age and sex. A high score for pain intensity at rest before nerve block increases the probability of pain reduction of more than 1.5 points after ultrasound-guided fascia iliaca compartment block (US-FICB) (Figure 2).
Discussion
In this prospective observational study with 33 hip fracture patients, ultrasound-guided fascia iliaca compartment block provided a clinically important analgetic effect for pain at rest in women and pain during movement in both sexes. Furthermore, a higher baseline NRS at rest was an independent predictor for clinically important pain relief by US-FICB. That finding indicates that patients experiencing a higher initial pain intensity are more likely to benefit from US-FICB.
The advantages of fascia iliaca compartment blocks have been described in previous literature. Verbeek et al. concluded that regional nerve blocks relieve dynamic pain effectively and increase patient satisfaction (19). Furthermore, patients are also described as tolerating the positioning for spinal anaesthesia better after FICB (20, 21).
The mean NRS reduction for pain intensity during movement in our study was 2.6 and 69.7% of patients experienced a clinically important analgetic effect for pain during movement. This finding is in line with the observational study by Ridderikhof et al. with supra-inguinal FICB, with a mean NRS reduction of 2.5; and 59% of patients improving more than 1.5 points (22).
Guay and Kopp found a 2.5 NRS score reduction thirty minutes after both FICB and femoral nerve block (23). In Gawthorne et al.’s prospective cohort study, US-FICB resulted in a mean NRS reduction of 3.7 (SD: 2.9) and 3.3 (SD: 2.6), when performed by either medical doctors or emergency department nurses. However, neither of these papers differentiated between pain at rest and during movement, which makes a direct comparison to our study challenging (6).
Wennberg et al.’s findings from their case-control study of 135 patients indicate a better effect of US-FICB for movement-evoked pain, compared to pain at rest (25). We also found a statistically significant higher NRS reduction for movement-evoked pain compared to pain at rest 60 minutes after US-FICB.
Pain during movement is important to assess and treat because it can impede motion, which is essential for post-operative mobilisation and the prevention of respiratory and circulatory complications (24).
In our study, NRS recordings both at rest and during movement suggest that female participants report higher pain intensity than their male counterparts. In their review paper, Palmeira et al. demonstrate how sex hormones, genetics, and psychosocial and cultural differences affect pain perception (26). One finding was that men generally express a greater tolerance for pain, while women show a greater willingness to report pain (16, 26).
In our study, we did not detect significant differences between the sexes. However, our study material was not adequately powered for this question. As already outlined by Templeton et al., future studies should include a sufficient number of patients for the generation of adequately powered stratified data for both sexes (27).
In our study, US-FICB achieved a significantly higher mean NRS reduction in patients reporting a higher initial pain intensity. Some authors have excluded patients with initial NRS ≤3, potentially affecting the results. (28). The minimally clinically important difference (MCID) for NRS recording was previously found to be 1.5 points (18).
Limitations
This observational study has inherent limitations compared to randomised controlled trials, such as the lack of a control group and a non-blinded design. Unfortunately, the time and resource limitations related to a master’s thesis, and delay at the regional ethics committee limited the available timeframe for data acquisition, resulting in the limited sample size. This may affect the internal and external validity of the results.
That is why we performed a post-hoc power analysis on all statistical tests, showing that our study was sufficiently powered for the majority of the statistical tests (see Table 2). Finally, previous history of chronic pain or chronic pain medication might be confounders for which we have no data.
Patients with nurse-diagnosed delirium and cognitive impairment were excluded, even though this patient group comprises a significant portion of all hip fracture patients. No formal screening and/or assessment tools for cognitive impairment and delirium were applied.
Seven patients report more pain at rest after US-FICB. One patient reports increased pain both at rest and during movement post-procedure. Possible explanations include statistic outliers and other potentially confounding patient-related factors which were not documented, such as anxiety, previous opioid (ab)use, or pain stimuli between the two NRS registrations, such as the moving of the patient from the stretcher to the hospital bed. Neither of these possible explanatory events was recorded during the scope of the study.
Given the resources dedicated to this investigation, only a single follow-up NRS registration after 60 minutes was performed. Ropivacaine achieves its onset of action within a timeframe of less than 15 minutes. Under ideal circumstances, multiple NRS registrations within 60 minutes might have revealed patients with non-clinically important responses to US-FICB earlier.
Additional registrations, e.g. after four hours, eight hours, and at the time of surgery could have provided more data about the longer-term effect of US-FICB. Ultimately, this study lacks data for the orally administered pain medication, which could potentially have influenced the NRS registrations.
In studies that examine clinical methods delivered by multiple providers, inherent inter-provider variability can introduce potential confounding factors. However, this study involves patients admitted unexpectedly at any time, making it challenging to have one or two dedicated nurse anaesthetists constantly available for the procedure.
Furthermore, NRS for pain with movement was recorded by two different methods before and after US-FICB. While pain with movement before US-FICB was defined as the patient’s spontaneous movements in bed, the pain after US-FICB was provoked by sliding a 20˚ wedge underneath the patient’s thigh. That methodological difference might potentially impair the validity of the results.
Finally, the sample size of 33 patients with complete datasets might limit the external validity of the results. The four-month timeframe was chosen with respect to the given resources dedicated to this study. Still, our principal findings correlate well with previous studies with significantly larger sample sizes (6).
Conclusion
US-FICB performed by nurse anaesthetists is a valuable tool for pain management with hip fracture patients, and our data indicate that it can have a clinically important analgetic effect, especially for pain during movement. Furthermore, it seems that US-FICB is particularly useful for patients with high initial pain intensity.
Larger studies, preferably randomised-controlled trials will be necessary to elucidate lingering issues, with a focus on the patient’s sex and the difference between pain at rest and movement-evoked pain. Finally, upcoming investigations should include cognitively impaired patients by applying existing tools for pain assessment in this patient group.
In the future, nurse anaesthetists will be required to master the use of ultrasound as a tool in clinical practice, hopefully for nerve blocks as well, to the benefit of an increasingly frail hip fracture patient population.
Acknowledgements
The authors would like to thank Prof. Marit Leegaard at Oslo Metropolitan University for her supervision and guidance.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge

Comments