Effects of de-escalation training on student nurses' skills and confidence
Summary
Background: De-escalation training is widely recommended for reducing violent incidents in the workplace, but is rarely included in nursing curriculums. Research suggests that nursing students should learn skills that enable them to respond to violence in a calm manner.
Objective: To test whether a de-escalation training session could improve nursing students’ de-escalation skills and their confidence in coping with patient aggression.
Method: The study was designed as a cluster randomised controlled trial that included three clusters (classes) of third-year nursing students allocated either to the intervention group (two classes, n=35) or the control group (one class, n=10). Data were collected at a Norwegian university college of nursing in February, August and November 2019. For each class, all data were collected over a period of five hours in one day. All participants were exposed to two simulation scenarios. The intervention group participated in a 50-minute de-escalation training session in between scenarios. The primary outcome was de-escalation skills, and the secondary outcome was confidence in coping with patient aggression. To measure de-escalation skills, videos of participants during the two simulation scenarios were used to collect data pre- and post-intervention. The English Modified De-escalating Aggressive Behaviour Scale (EMDABS) was applied to code videos. Confidence in coping with patient aggression was obtained through a validated self-report questionnaire before and after the two simulation scenarios, pre- and post-intervention.
Results: After participating in the de-escalation training session, the students in the intervention group demonstrated positive changes in de-escalation skills compared to those of the control group. With regard to confidence in coping with patient aggression, both groups’ scores improved after they had attended simulation scenarios, but the largest improvements occurred after they had participated in the de-escalation training session.
Conclusion: The results suggest that de-escalation training has the potential to increase nursing students’ de-escalation skills and their confidence level in coping with patient aggression. Given the limitations of this study, replication with larger sample sizes is needed.
Cite the article
Nag T, Gjestad R, Senneseth M. Effects of de-escalation training on student nurses' skills and confidence. Sykepleien Forskning. 2023;18(92716):e-92716. DOI: 10.4220/Sykepleienf.2023.92716en
Introduction
Workplace violence is a major concern among healthcare professionals worldwide (1). It can have severe consequences at both an individual level and at an organisational level (2). It can also cause physical and emotional injuries, increase sick leave, reduce job satisfaction and increase staff turnover (3–5).
Nurses are particularly exposed to workplace violence, and nursing students may be especially vulnerable to its consequences (6–9). Ultimately, violent incidents may play a role in why nursing students consider leaving their profession (7).
National and global organisations recommend systematic training initiatives to address workplace violence (10, 11). Historically, many healthcare providers have viewed restrictive patient interventions as a safe and effective approach to managing violence (12).
However, recent practice standards have moved toward a more patient-centred and less restrictive approach (15). The National Institute for Health and Care Excellence (NICE) recommends using de-escalation techniques to prevent violent incidents (16).
De-escalation has been defined as ‘talking with an angry or agitated service user in such a way that violence is averted and the person regains a sense of calm and self-control’ (16, p. 30). It is a communicative approach to aggressive behaviour that is considered more dignified and humane, as well as less coercive compared to physical interventions (17).
A review of the evidence base for de-escalation found that participants in de-escalation training increase their knowledge and confidence level (18). However, there is still insufficient evidence of its effectiveness in improving staff performance (14, 15, 19, 20), and there have been few experimental studies that include control groups (13, 21).
In recent years, the four health regions in Norway have jointly developed a national staff training programme called the ‘Management of Aggression Programme’ (MAP), which is based on the existing international literature and evidence in the aggression management field (22). This programme is now being implemented nationwide in Norway.
One of the main parts in this programme is the de-escalation training, which focuses on creating a safe place both physically and psychologically (23), engaging empathically and exploring the other person’s point of view (24), and resolving underlying distress through collaborative problem-solving (23).
De-escalation training might have great potential for improving de-escalation behaviour in nurses, but there is limited knowledge about the extent to which such training actually contributes to improving skills. Due to the recent nationwide implementation, the present study aims to test the de-escalation training session used in the MAP model on nursing students’ de-escalation skills and confidence level in coping with aggression.
Method
Aims
The present study aims to test the impact of the brief de-escalation training used in the MAP model on nursing students’ de-escalation skills and confidence level in coping with aggression.
The study aims to test two hypotheses:
- De-escalation training will improve the de-escalation skills of nursing students.
- De-escalation training will improve nursing students’ level of confidence in coping with aggression.
The study’s primary outcome is de-escalation skills, while confidence in coping with aggression is a secondary outcome.
Design
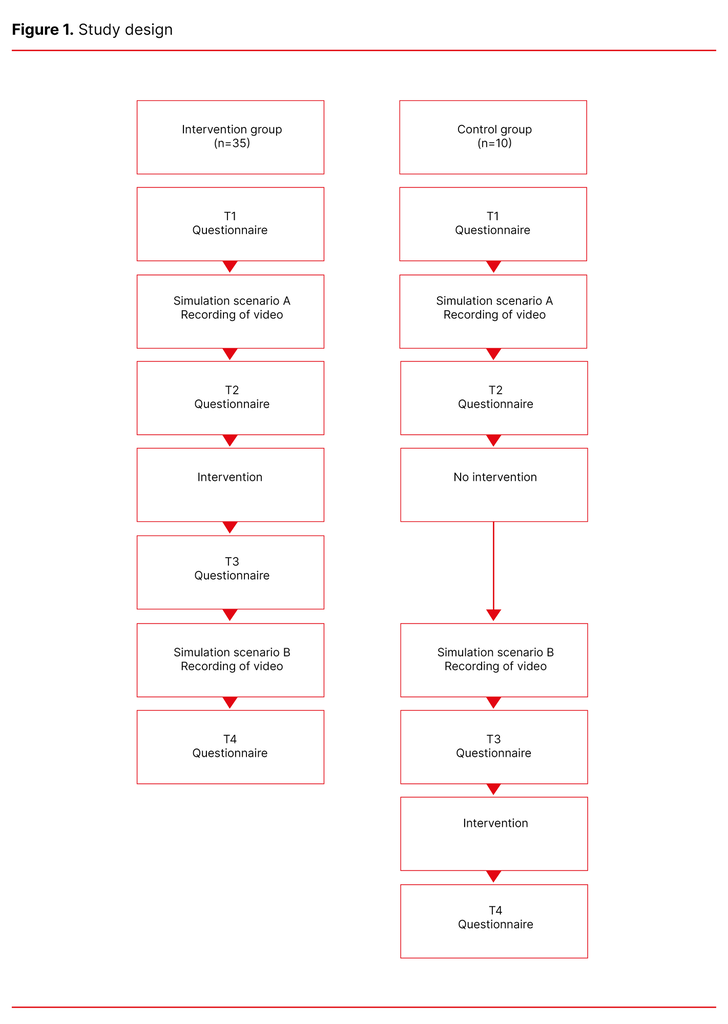
A cluster randomised controlled trial with a pre-post design was conducted to test the two hypotheses (Figure 1). Within one year (2019), the three classes of third-year nursing students at a Norwegian University College were randomly assigned to either the intervention or the control group. The classes represented natural clusters.
The randomisation sequence was created using the random number function in Microsoft Excel (2016) (25) prior to recruitment. Two of the clusters were allocated to the intervention group and one cluster to the control group. All three clusters were blinded; participants did not know which group they had been assigned to.
Due to ethical concerns, the university college where the students were recruited from, required all participants to receive the intervention independent of group allocation. Therefore, the participants in the control group also received the intervention, but not until data collection of the primary outcome was completed (Figure 1).
Sample and participants
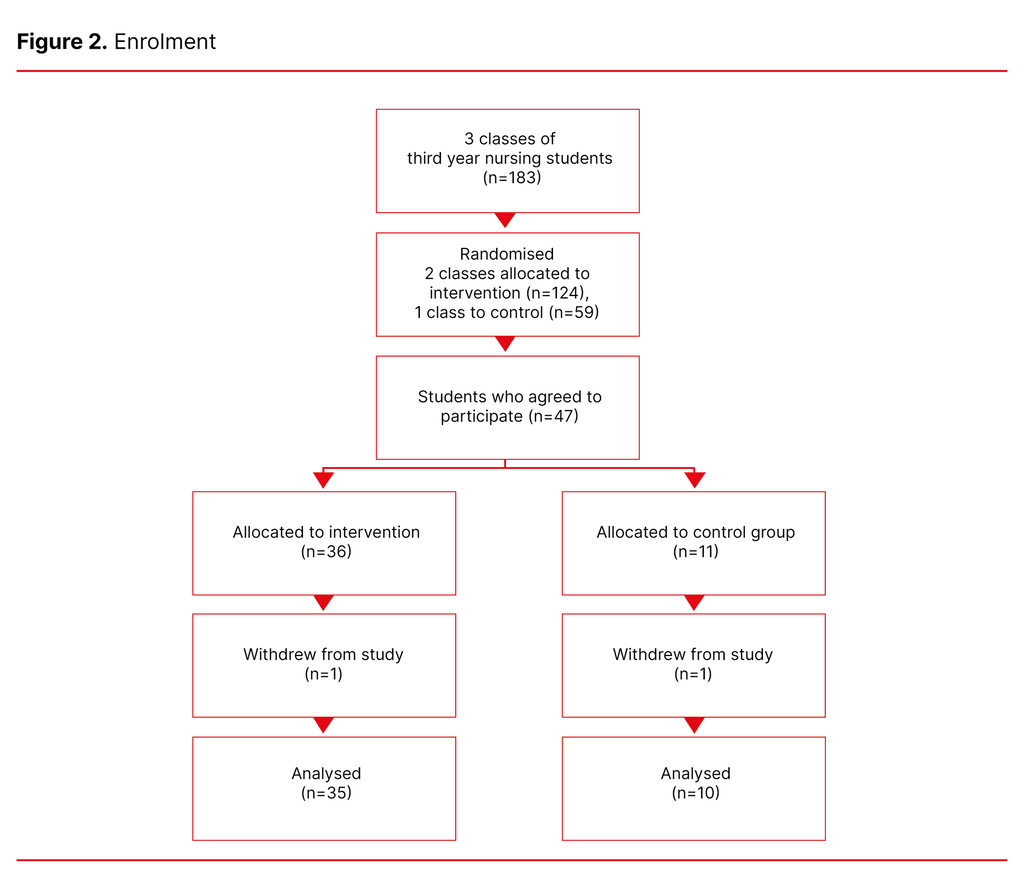
A self-selection sampling approach was used in the three clusters (classes) of third-year nursing students. The three classes consisted of 61, 63 and 59 students, respectively. A flow diagram of the study participants is outlined in Figure 2.
All students in the three classes were invited to participate in the experiment. The inclusion criterion was that they were able to both understand and communicate in Norwegian. A total of 47 students gave their informed consent. Two withdrew from participation, leaving 45 participants in the study. The majority of the participants were female.
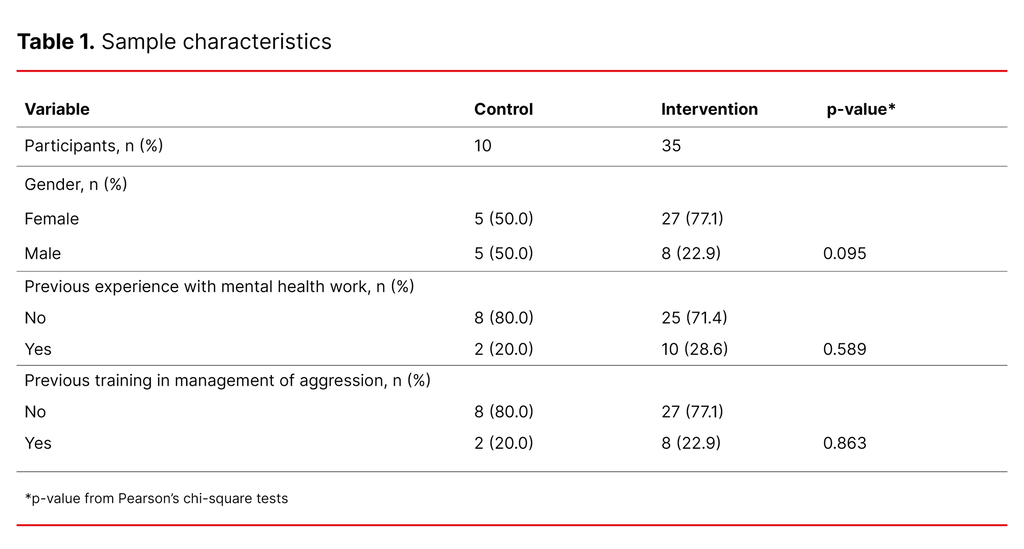
More than 70% had no previous training in the management of aggression. Ten were allocated to the control group and 35 to the intervention group. The size of the control group was small, as the recruitment from this particular class was lower than the other clusters (Table 1). Participant characteristics were similar in the groups.
Intervention
The intervention consisted of the de-escalation training as described in the Norwegian staff training programme for the management of aggression, called ‘MAP’ (see Appendix 1 for details) (22). The de-escalation training is specifically designed to improve de-escalation skills. Participants received the intervention in a classroom at the university college.
The intervention group underwent the de-escalation training after being exposed to the first test scenario (simulation scenario A) and before being exposed to the second test scenario (simulation scenario B), while the control group underwent the training after exposure to both test scenarios (Figure 1). The intervention lasted for 50 minutes.
Data collection
Data were collected in February (intervention group), August (intervention group) and November (control group) 2019. For each of these three data collection time points, and for participants in the three classes respectively, all data were collected over a period of five hours in one day.
The primary outcome of this study was changes in de-escalation skills and the secondary outcome was changes in coping with patient aggression. To assess these outcomes, data were collected through two data sources: coding of recorded videos from two simulation scenarios (A and B) pre- and post-intervention, and self-reported questionnaires.
Recording and coding of videos of simulation scenarios
Video data were collected from participants’ simulation scenarios. Simulation scenarios A and B consisted of two different short role-plays in a somatic setting (Appendix 2), involving an aggressive simulated patient played by an experienced care provider (actor). There were two different actors for scenario A and scenario B. Each student interacted on their own with the simulated patient and was asked to manage the situation to the best of their ability.
The video data were recorded in a simulation lab equipped like a hospital room. A researcher was operating the video equipment from a control room nearby. Prior rehearsals were conducted to make sure that the simulation scenarios appeared realistic. The average run-time of the videos was four minutes. A successful verbal de-escalation can usually be accomplished within five minutes (24).
The coding of the recorded videos pre- and post-intervention constituted the baseline and post-test measures, respectively. The purpose of these videos was to assess the student’s baseline skill level and the effects of the intervention. The pre- and post-video recordings amounted to a total of 90 videos. Videos were coded by two external raters who were blinded to both pre- and post-training designation and the group allocation. Mean values were computed based on the raters’ scores.
Instruments
Both instruments were translated into Norwegian using back-translation with bilingual testing (26). Permission to translate and use the instruments in the present study was granted by the authors.
English Modified De-escalating Aggressive Behaviour Scale (EMDABS)
All videos were coded using the ‘English Modified De-escalating Aggressive Behaviour Scale’ (EMDABS) (Appendix 3). EMDABS is an observer-rated measure of de-escalation behaviour (27). It is based on the evidence presented by Nau et al. (28). EMDABS is psychometrically validated for use in both research and practice, and it is shown to have good inter-rater reliability and strong internal consistency (27).
The tool is designed to measure the de-escalation skills of staff, and does not measure the outcome of the de-escalation. However, it is suggested that the EMDABS may be a useful instrument for assessing the effectiveness of training in de-escalation (27). The scale consists of seven items, which are scored from 1 to 5, with lower scores indicating least desirable de-escalating practice and higher scores indicating most desirable de-escalating practice.
Confidence in coping with patient aggression scale
The confidence in coping with patient aggression scale (Appendix 4) was used to measure the nursing students’ confidence in managing an aggressive patient. It consists of ten items, which are scored from 1 to 11, with lower scores indicating less confidence and higher scores indicating greater confidence.
The instrument has previously demonstrated a high degree of precision and internal consistency (29), and high levels of reliability (Cronbach’s alpha = 0.92) and validity (29). It has been widely used in a range of studies measuring confidence in dealing with patient aggression (30–32).
Students were asked to fill out the ‘Confidence in Coping with Patient Aggression’ questionnaire at four time points in order to detect any changes in their confidence levels throughout the study (Figure 1).
Data analysis
Data were analysed using SPSS software, version 24.0. The EMDABS outcome variables are analysed as continuous variables. Descriptive analyses included mean and standard deviation (SD) of continuous variables and frequencies of categorical variables. Cross-tabulation of frequencies was tested using a chi-square test. Within-group change was tested using a paired sample t-test.
General linear model (GLM) was used to model repeated measures ANOVA, testing group differences, time effects and group differences in changes over time (the interaction term). Effect sizes were calculated to compare the difference within and between groups, using the formula for Cohen’s d, assessed against criteria small (d=0.2), medium (d=0.5) and large (d≥0.8) (33).
Ethical considerations
Participants were informed about the study verbally and in writing, and they provided written consent prior to participation. They received two cinema tickets for participating. All students were offered an individual debrief in case of negative emotional impact. Five students accepted this offer.
The study was approved by the Norwegian Centre for Research Data (reference number 716537) and registered in clinicaltrials.org (registration number: NCT03924141).
Results
Improvement in students’ de-escalation skills
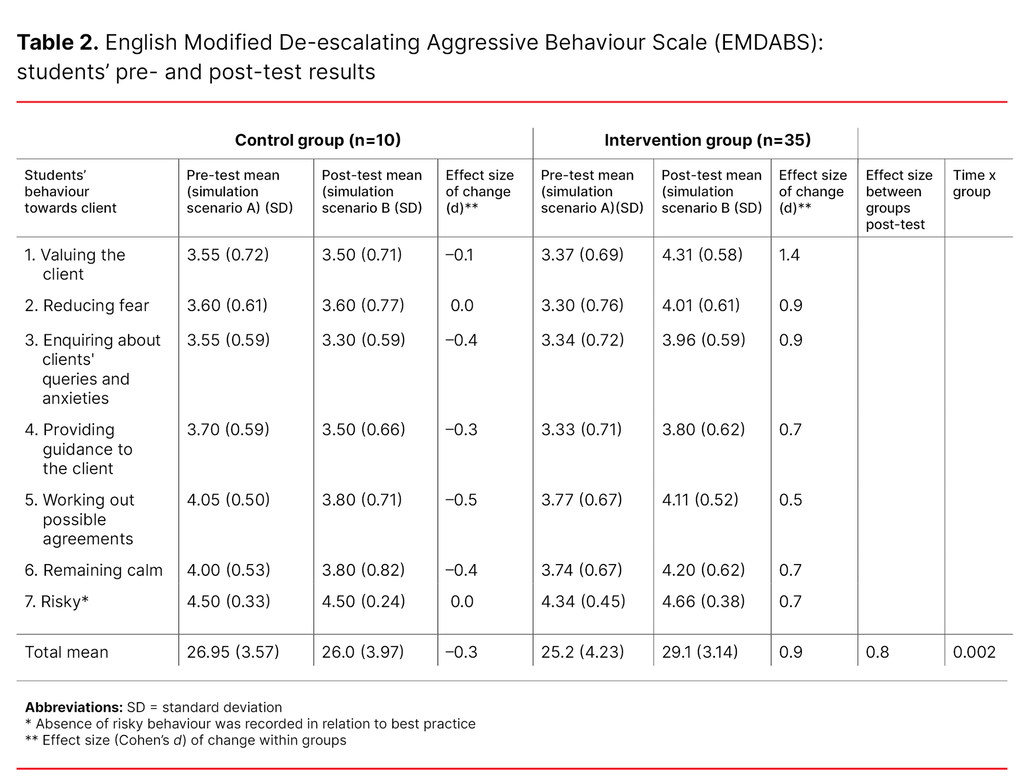
After the de-escalation training session, the students in the intervention group demonstrated significant positive changes in de-escalation skills (p<0.01). Compared to the control group, the intervention group demonstrated better de-escalation skills after the intervention, as indicated by the time x group interaction p=0.002 (Table 2). The effect size for the difference in de-escalation skills between groups after simulation scenario B was d=0.8. Significant improvements were also seen in each item of the EMDABS scale in the intervention group (p<0.01).
The control group showed a slight decrease in de-escalation skills from pre- to post-test, but this change was not statistically significant. No other significant changes were observed within the control group.
Effect sizes showed medium to large effects on each of the de-escalation skills within the intervention group, including the total mean (d=0.9). Conversely, all effect sizes within the control group were estimated to be trivial (d≤0.2) (Table 2).
Improvement in students’ level of confidence in coping with patient aggression
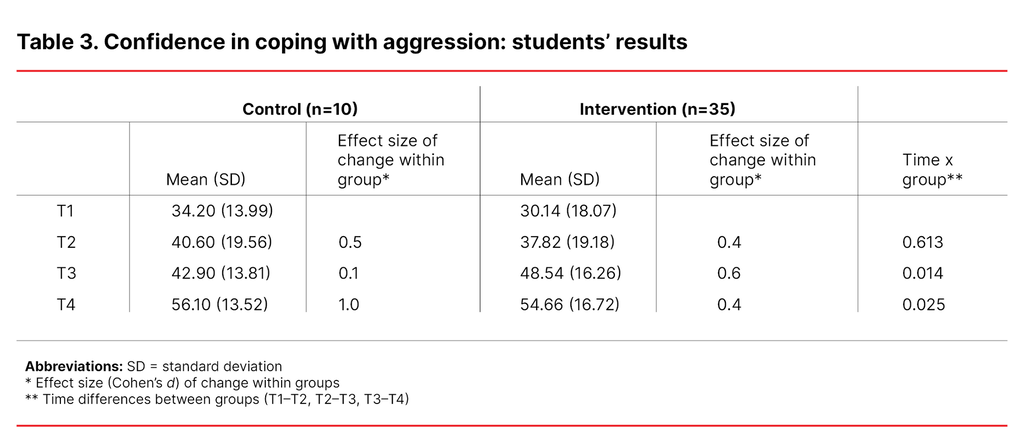
For both groups, improvement in the secondary outcome measure – nursing students’ level of confidence in coping with patient aggression – was seen after each simulation scenario, but the most substantial improvement occurred after de-escalation training (Table 3).
Baseline measures showed no significant differences between the groups’ level of confidence in coping with patient aggression. After the first simulation scenario (T2), both groups displayed an almost identical increase in self-reported confidence levels. The groups started to show divergent developments between intervals T2–T3 and T3–T4.
Between intervals T2–T3, the intervention group underwent the de-escalation training prior to simulation scenario B, resulting in a medium effect on confidence levels (d=0.6). In contrast, the control group proceeded directly to simulation scenario B, resulting in a trivial effect on confidence levels (d=0.1).
Between intervals T3–T4, the intervention group proceeded with simulation scenario B, while the control group underwent the de-escalation training. The intervention group showed a small effect (d=0.4) after completing simulation scenario B, while the control group exhibited a large effect (d=1.0) after undergoing the de-escalation training.
Both groups had almost identical mean scores on level of confidence in coping with patient aggression at T4, by which point all of them had received the intervention.
Discussion
The aim of this study was to test whether the 50-minute de-escalation training session, defined in the ‘Management of Aggression Programme’ (MAP), could improve nursing students’ de-escalation skills and levels of confidence in coping with aggression. The results suggest that the de-escalation training has the potential to foster such improvements. However, these results should be interpreted with caution due to the small control group in the present study. Future research efforts should focus on replicating these findings with larger samples.
In this study, significant positive changes in de-escalation behaviour were seen in the intervention group, while there were no changes in the control group. The extent of these changes indicates that these improvements could have clinically meaningful effects (33).
The simulation scenarios involved two rather different situations with different actors. The post-test results for the intervention group indicate that the students were able to translate the knowledge gained from the de-escalation training into practice. They were able to generalise and apply the skills to a situation for which they had not been specifically trained. This strengthens the assumption that the students learned skills that they could actually apply to a new context. This transferability of skills indicates potential for the training to be clinically significant (34).
In a similar de-escalation study on nursing students, Nau et al. (30) found a significant increase in skill levels after 24 hours of training. Results from the present study suggest that de-escalation training lasting just 50 minutes can also have positive effects and that increasing the training dosage could further improve skill levels. However, the brief duration of the de-escalation training in this study suggests that limited resources can still make an impact on delivering de-escalation training to nursing students. This could be a focus for future research.
The results of this study indicate that exposure to simulation scenarios alone may improve nursing students’ confidence in coping with patient aggression. Both groups experienced an increase in their confidence levels after attending the first simulation scenario.
It is worth noting that the control group with two sequential simulation scenarios did not experience a further increase in their confidence levels, but maintained the previous levels of achieved confidence in coping with patient aggression. This may indicate that a higher dose of simulation scenarios does not necessarily add additional benefits as regards confidence levels.
The largest increase in the nursing students’ confidence levels was found when the control group underwent the de-escalation training after completing both simulation scenarios. This may indicate that a higher dose of exposure induced by simulation scenarios increases the students’ receptivity to training. At the end of the experiment, the control group and the intervention group reported similar levels of confidence, despite undergoing the de-escalation training in a different order. This indicates that adding simulation scenarios to de-escalation training can have a synergistic effect on increasing nursing students’ confidence in coping with patient aggression.
Further, the total cumulative effect of the simulation scenarios and the de-escalation training was more important than the specific order in which the training was received. However, if the goal is to achieve the highest possible level of confidence in coping with patient aggression, specific training in de-escalation should be included.
Strengths and limitations
The strength of the present study was the randomised controlled experimental design, which included assessing participants’ behaviour and skills, rather than solely using self-report questionnaires. Furthermore, it was a strength that raters were blinded for participants’ group allocation.
Nevertheless, the study has several limitations. First, the small sample size may have resulted in less robust parametric testing procedures. This may affect the reliability of the results and limit the generalisability of the study. The absence of a control group is often noted in previous studies of de-escalation training (32). This study was therefore conducted as a cluster randomised controlled trial to account for unknown variables potentially affecting the outcomes. However, the cluster randomisation led to an unequal distribution of participants in the groups, and the sample sizes in both groups (particularly the control group) are relatively small.
The limitation caused by the small sample size is thus further reinforced by the relatively small size of the control group. Due to practical limitations set by the university college, we were only allowed to recruit students from three nursing classes. Thus, sample size calculations to ensure statistically meaningful results were not performed prior to conducting the study.
Second, the intervention was administered by the first author. However, to reduce potential bias, the author played no part in the randomisation process and coding of videos, and played only a limited part in the statistical analysis.
Moreover, this study tested de-escalation skills in a somatic environment. It would be of interest to examine whether the de-escalation training would give similar results in simulation scenarios that are adapted to another context, e.g. mental health services. Furthermore, it could be interesting to test if the skills have sustainability. This may be a focus for future studies.
Conclusion
Results from this study suggest that brief de-escalation training may improve students’ de-escalation behaviour as well as their confidence in coping with patient aggression. Exposure to simulation scenarios may help improve nursing students’ confidence levels. However, improvements in de-escalation behaviour and skills were associated with de-escalation training.
Replication in future longitudinal studies with larger samples is needed to increase statistical power and ensure higher internal validity and generalisability of results.
We would like to thank the participants in the study for their valuable contribution. In addition, we greatly appreciate the facilitating work of the Regional Competence Centre for Research and Education in Forensic Psychiatry at Helse Bergen.
Funding
The Regional Competence Centre for Research and Education in Forensic Psychiatry at Haukeland University Hospital funded translations of the instruments as well as students' compensation for participation.
Conflicts of interest
- Thomas Nag is the managing director of the Norwegian national staff-training programme ‘Management of Aggression Programme’ (MAP).
- Mette Senneseth is a member of the research and development group associated with the staff-training programme MAP.
- None of the authors have any commercial or financial interests in MAP.
Open access CC BY 4.0.
The Study's Contribution of New Knowledge

Comments